Deceased organ donation efficiency in Switzerland from 2014 to 2023 compared to other
European countries according to the Donor Conversion Index (DCI) – an ecological study
DOI: https://doi.org/https://doi.org/10.57187/s.4609
Andreas
Elmera,
Julius
Weissa,
Nathalie Krügela,
Markus Béchirab,
Christian
Brunnerac,
Sabine
Camenischad,
Raphaël
Giraudae,
Yvonne
Hilpertshauseraf,
Matthias
Peter Hiltyag,
Marco M. Ruscaah,
Kai Tisljarai,
Franz F. Immera
a Swisstransplant,
Bern, Switzerland
b Centre for
Internal Medicine, Hirslanden Clinic Aarau, Aarau, Switzerland
c Centre for Internal Medicine, Cantonal Hospital
Lucerne, Lucerne, Switzerland
d Department of Intensive Care Medicine, Bern University Hospital, Bern, Switzerland
e Intensive Care Division, Department of Acute
Care Medicine, Geneva University Hospitals, Geneva, Switzerland
f Division of Intensive Care Medicine, Cantonal
Hospital St. Gallen, St. Gallen, Switzerland
g Institute of Intensive Care Medicine,
University Hospital of Zurich, Zurich, Switzerland
h Department of Intensive Care Medicine, Lausanne
University Hospital, Lausanne, Switzerland
i Clinic for Intensive Care Medicine, University
Hospital Basel, Basel, Switzerland
Summary
AIMS OF THE STUDY: Deceased donation activity is typically calculated as the number
of donors per year per
million people (pmp) and is referred to as the donation rate. To assess donation
efficiency rather than donation activity, concepts such as the Donor Conversion
Index (DCI) consider that not every death is eligible for organ donation. These
are primarily deaths resulting from diseases associated with potentially
devastating cerebral injury leading to brain death. We present the 2014–2023 evolution
of the deceased donation activity and efficiency in Switzerland compared with selected
European countries. How does Switzerland perform when organ donation programmes
are evaluated using the DCI instead of the donation rate? The results are
discussed in the context of implemented measures in Switzerland to increase
organ donation activity.
METHODS: We calculated the DCI (number of
donors divided by the number of eligible deaths, multiplied by 100), donation
rate (number of donors divided by the number of residents, multiplied by 106),
and mortality rate (number of eligible deaths divided by the number of
residents, multiplied by 105) for each country and year using population-based
data from the Global Observatory on Donation and Transplantation (GODT) and
Eurostat. Eligible deaths for deceased organ donation include deaths from
diseases associated with potentially devastating cerebral injury related to
brain death, as defined by selected ICD-10 codes suggested by the European
Directorate for the Quality of Medicines & Healthcare. We present trends
for the years 2014–2023 for all three indicators and compare the results of Switzerland
with those of seven European countries (Austria, France, Germany, Italy, the
Netherlands, Spain, and the United Kingdom).
RESULTS: Over the 10-year study period,
efficiency, as measured by the DCI, increased by 2–72% in all countries. In Switzerland,
the DCI rose from 3.2 donors per 100 eligible deaths in 2014 to 5.5 donors per
100 eligible deaths in 2023, representing the largest increase in efficiency among
the countries analysed (+2.3 donors per 100 eligible deaths, or +72%). The
primary driver of Switzerland’s improved donation efficiency was increased
donations after circulatory determination of death (DCD) since 2016. The DCI offers
a different perspective on
donation activity compared with the donation rate expressed in pmp. The upward
trend over the past decade in the countries analysed is less pronounced for the
donation rate than for the DCI. This divergence is accompanied by a declining
mortality rate of diseases eligible for donation during the period studied. At
the end of the study period, Switzerland's total DCI ranked second among the
countries analysed, following Spain, while its donation rate in pmp ranked
fourth, following Italy and France. Among the countries analysed, Switzerland
had the lowest mortality rate of diseases eligible for organ donation
throughout the study period.
CONCLUSIONS: Despite declining next-of-kin consent
rates, Switzerland's organ donation programme is among the most efficient in
Europe, according to the DCI. If consent matched that of other countries,
efficiency could be even higher. The increase in the DCI from 2014 to 2023 suggests
that measures to increase organ donation rates in Switzerland may have been
effective. Swiss emergency and intensive care staff appear to appropriately identify,
refer, and manage potential deceased organ donors. When comparing trends in
organ donation figures between countries, it is important to consider
differences in mortality due to eligible diseases associated with potentially
devastating cerebral injury leading to brain death.
Introduction
The activity and efficiency of national
deceased organ donation programmes are assessed by different methodologies,
which primarily differ in how they define donor potential [1]. A common and straightforward
approach determines donor potential at the level of the entire population of a
country or region, dividing the number of donors by the number of residents.
This figure is typically known as the donation rate and is expressed as donors per
million population (pmp). Up-to-date national census data are readily available
and enable quick and easy comparisons between countries. However, this approach
has limitations. Most importantly, not all causes of death in the population
are eligible for organ donation, and mortality due to those causes (mostly
potentially devastating cerebral lesions related to brain death) may vary
between countries and over time [2]. This may introduce bias when the donation rate
pmp is used for country
comparisons or when the evolution of national deceased organ donation
efficiency is assessed over time.
An alternative approach is to define the
deceased donor potential at the hospital level, that is, as the number of
hospitalised patients who meet medical eligibility criteria [3–7]. However, this approach
presupposes
the review and analysis of medical records in all hospitals with intensive care
units (ICUs), as is the case in Switzerland with the Swiss Monitoring of
Potential Donors (SwissPOD) [8, 9]. In addition to data protection issues that arise
when collecting
individual health-related data, such a monitoring system requires significant
financial and human resources. Furthermore, it is not always obvious whether a
patient in the ICU or emergency department fulfils the medical eligibility
criteria for deceased organ donation, and data collected in this way are not internationally
comparable. In addition, monitoring deceased donor potential at the hospital
level fails to assess the ability of an organ donation system to refer
potential donors to hospitals with adequate facilities and resources for donor
management.
A third approach, proposed by Weiss et al. [10] and others [11, 12], utilises official
national cause-of-death
statistics, which are typically available online or upon request by national or
supranational administrations. The deceased donor potential is estimated at the
population level using a set of causes of death that are eligible for deceased
organ donation, with ICD-10 codes applied for diseases associated with
potentially devastating cerebral injury leading to brain death. Weiss et al. (2018)
proposed the utilisation of the Donor Conversion Index (DCI) as a metric for evaluating
the efficiency of national deceased donation programmes, replacing the donation
rate pmp approach. This is because the DCI provides an unbiased assessment,
unaffected by variations in mortality rates resulting from deaths eligible for
organ donation.
In this article, the efficiency of the Swiss
organ donation programme is analysed and compared with that of selected
European countries over a 10-year period from 2014 to 2023 using the DCI
approach. Efficiency metrics are presented for programmes of donation after
brain death (DBD pathway), programmes of donation after circulatory
determination of death (DCD pathway), and overall national programmes combining
DBD and DCD pathways. In comparison with previous publications that have used
the DCI [10, 13], the
present study refines the methodology and uses more precise ICD-10 data,
enabling a clearer definition of the deceased donation potential in accordance
with the Guide to the Quality and Safety of Organs for Transplantation [14]. The DCI
metric is compared with donation
rates pmp, and the underlying specific mortality rates are presented to determine
whether they vary between European countries and over time.
Materials and methods
Study design and setting
We retrospectively analysed routinely collected
annual health data on organ donation (i.e. the number of actual donors) and
causes of death (i.e. the number of eligible deaths) from 2014 to 2023. The Donor
Conversion Index (DCI), a measure of donation efficiency; the donation rate (in
pmp), a measure of programme activity; and the organ donation-specific mortality
rate, which reflects the pool of eligible donors, were calculated for Switzerland
and seven European countries (i.e. Austria, France, Germany, Italy, the
Netherlands, Spain, and the United Kingdom).
Donor Conversion Index (DCI) = (number of donors / number of eligible deaths) × 102 per year
Donation rate (in pmp) = (number of donors / number of residents) = × 106 per year
Mortality rate = (number of eligible deaths / number of residents) × 105 per year
We followed the Reporting of Studies Conducted
using Observational Routinely Collected Data (RECORD) guidelines [15]. All data were
fully aggregated at
the country level, consistent with an ecological study design. As no individual
health-related data were used, ethics committee approval was not required for
this study.
Data sources and population selection
Organ donation data
Annual data on deceased organ donation (2014–2023)
for each country were obtained from the Global Observatory on Donation and
Transplantation (GODT), a collaboration between the World Health Organization
(WHO) and the Spanish Transplant Organization, Organización Nacional de
Trasplantes (ONT). The dataset was downloaded from the GODT website [16]. The numbers
of total actual
deceased donors, actual DBD donors, and actual DCD donors were used. An actual
donor is a deceased person on whom an operative incision was made with the
intent of organ procurement for transplantation.
Data on causes of death eligible for deceased organ donation
Annual data on specific causes of death (2014–2023)
for each country were obtained from Eurostat upon request (data extracted on
10.12.2024). The selection of causes of death eligible for deceased organ donation
was based on the European Directorate for the Quality of Medicines & Healthcare's
(EDQM) “Guide to the quality and safety of organs for transplantation” (table
2.3: International Classification of Diseases [ICD]-10 codes of conditions associated
with potentially devastating cerebral lesions related to brain death) [14] and included
the following groups
of cerebral lesions:
- cerebrovascular
accidents (ICD I60–I66 and all sub-classifications)
- cerebral
damage (ICD G93.1, G93.5, G93.6, and all sub-classifications)
- cerebral
neoplasms (ICD C71, D33, and all sub-classifications)
- CNS
infections (ICD G00, G01, G02, G03, and all sub-classifications)
- V01-V99,
Y85 (transport accidents), used as a proxy for trauma because the corresponding
ICD-10 codes were not available (i.e. S02 fracture of skull and facial bones, S06.1
traumatic cerebral oedema, S06.2 diffuse brain injury, S06.3 focal brain
injury, S06.4 extradural haemorrhage, S06.7 intracranial haemorrhage with
prolonged coma, S06.8 other intracranial injuries, S06.9 intracranial injury
unspecified, according to table 2.3 of the EDQM guide to the quality and safety
of organs for transplantation)
Note that potential DCD donors may have causes
of death other than those listed above. However, we assume that patients who
are successfully resuscitated but later undergo withdrawal of life-sustaining
therapy are classified under anoxic brain damage (ICD code G93.1) according to
the ICD. The extent to which this may limit the applicability of the DCI
concept to DCD donors is addressed in the limitations section of the study.
The cause of death dataset included a total of 1,634,507
deaths. For 246 deaths (0.15‰), the underlying causes were withheld by Eurostat
to prevent the identification of individuals. This information is withheld when
fewer than four deaths have occurred for a certain cause in any combination of
country, sex, year, and age group. These deaths may or may not have fallen
under the relevant ICD classifications; therefore, they were removed from the
dataset for analysis. Deaths in the Principality of Liechtenstein were added to
the number of deaths in Switzerland, as organ donors from Liechtenstein are
included in the Swiss donation figures.
In the time series of causes of death, certain
years were missing for some countries. These missing data points were imputed
using the PROGNOSE.ETS function in Microsoft Excel when they occurred at the
end of the time series (2019–2023 for the UK, 2022–2023 for Germany and Italy,
2023 for all other countries). For missing data within the time series (Austria,
2019 only), the moving average of the preceding and the following year was
used.
Demographic data
Census data (2014–2023) for each country were retrieved
from the Eurostat Data Browser [17] and are based on the resident population on 1
January of each year. The
latest available numbers of the resident population, provided by Eurostat, were
used as the denominator to calculate consistent donation rates pmp. Our
donation rates may slightly differ from those published elsewhere due to the use
of different population data in those sources.
Data cleaning and analysis
Country identifiers in all datasets were
harmonised using ISO 3166-1 alpha-2 country codes with the R package “countrycode”
to ensure consistency across
sources. Data cleaning and processing were performed using R version 4.4.2 (R
Project for Statistical Computing).
Donation efficiency (DCI) and donation activity
(donation rate) were analysed separately for each country and for both the DBD
and DCD pathways. Specifically, DCI was calculated as the number of DBD or DCD
donors divided by the number of eligible deaths, and the donation rate was
calculated as the number of donors per million residents. These metrics were
also computed for both pathways combined (i.e. the total number of donors
divided by the number of eligible deaths and the total number of donors divided
by the number of residents, respectively).
To assess the evolution of donation efficiency
over time in individual countries, DCI time series were plotted, and both absolute
and relative changes (in percentages) in the DCI from 2014 to 2023 were
calculated. Donation efficiency was then compared to donation activity by analysing
country rankings according to both the DCI and donation rate at the end of the
study period (2023). Additionally, we conducted a qualitative visual comparison
of trends in the DCI and donation rate over the entire study period using their
respective line plots.
Results
Efficiency of national organ donation programs
from 2014 to 2023
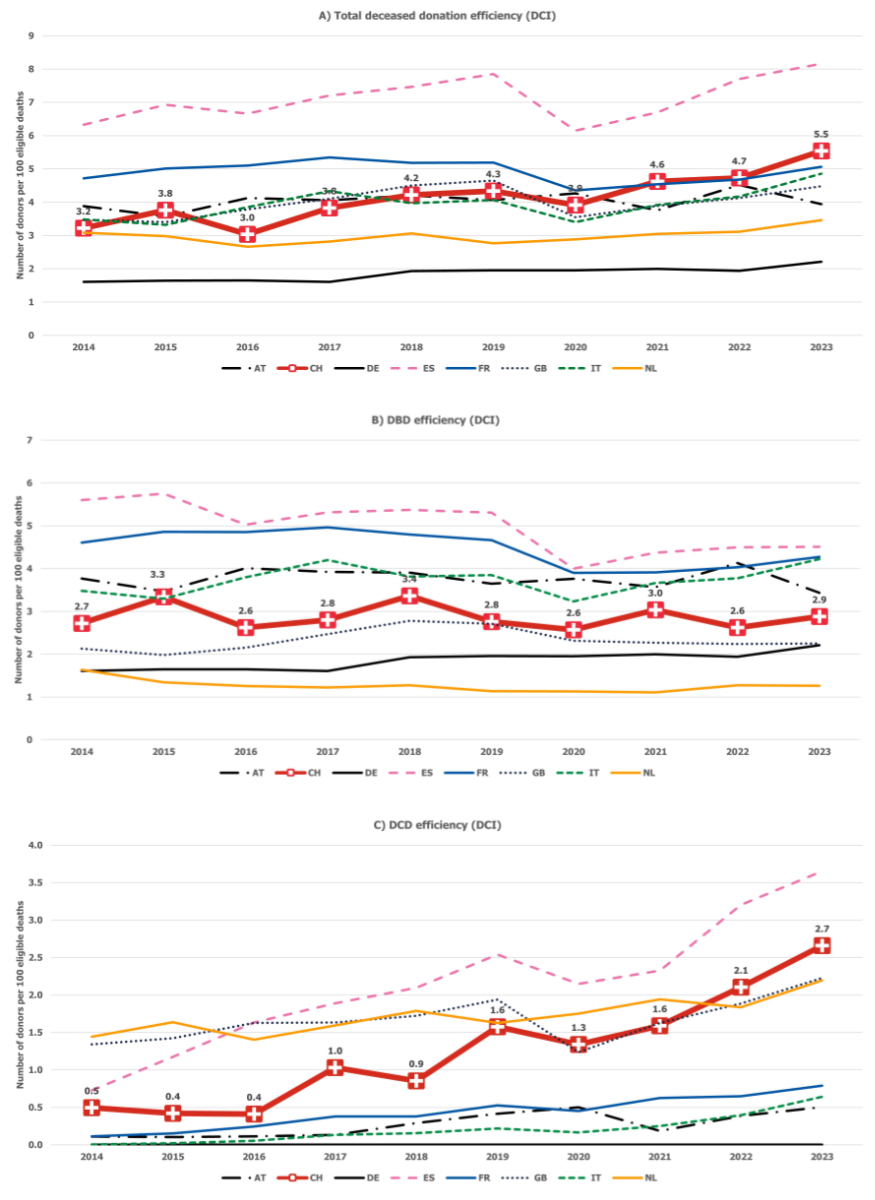
The efficiency of deceased donation programmes
was measured in eight European countries using the Donor Conversion Index
(DCI), which calculates the number of donors per 100 eligible deaths. Over the
10-year study period, efficiency increased in all countries by 2–72%.
Switzerland demonstrated an increase in the DCI, which rose from 3.2 donors per
100 eligible deaths in 2014 to 5.5 donors per 100 eligible deaths in 2023. This
represents the most substantial improvement in efficiency among all countries (+2.3
donors per 100 eligible deaths, or +72%). Switzerland's efficiency increase is
attributable to a 6.75-fold increase in DCD activity since 2016, from 0.4 to
2.7 donors per 100 eligible deaths. Swiss DBD activity remained relatively
stable throughout the study period (from 2.7 in 2014 to 2.9 in 2023). Spain and
the UK showed comparable trends to Switzerland, with a substantial increase in
overall donation programme efficiency (+29%), also primarily driven by increased
DCD activity rather than DBD activity (figure 1, table 1).
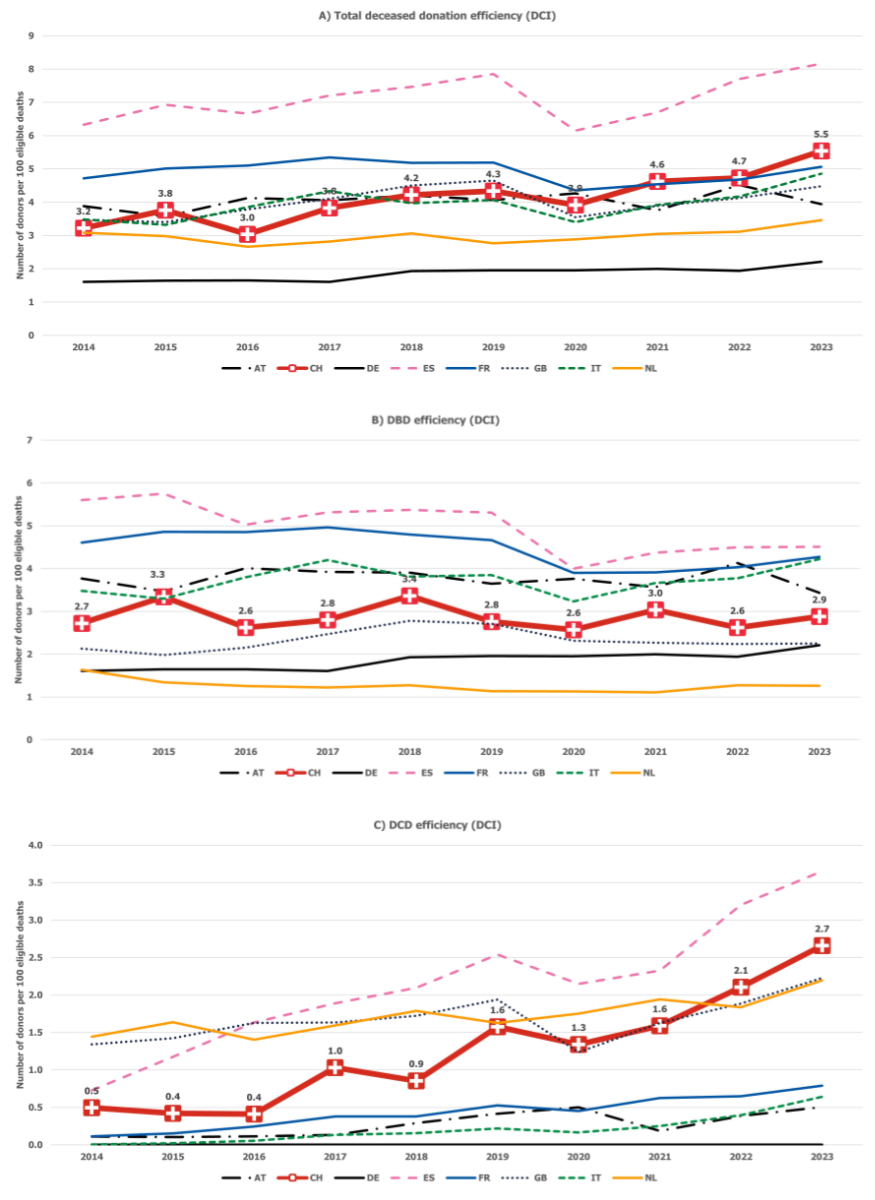
Figure 1Total (A), DBD (B), and DCD (C)
efficiency of national organ donation programmes according to the donor
conversion index (DCI). Germany (DE) has no DCD programme
(prohibited by law). In the time series of eligible deaths (the denominator in
the DCI), data had to be imputed for certain years and countries (see the “Materials
and methods” section for details). DBD:
donation after brain death; DCD: circulatory determination of death; AT:
Austria; CH: Switzerland; DE: Germany; ES: Spain; FR: France; GB: the United
Kingdom; IT: Italy; NL: the Netherlands.
Table 1Efficiency of deceased organ donation programmes (DBD and DCD) by country
according to the DCI at the beginning and end of the study period, as well as
absolute and relative DCI changes. Countries are ordered by 2023 DCI.
| Country |
Donor conversion index (DCI) |
| |
2014 |
2023 |
Absolute change |
Relative change |
| Spain (ES) |
6.3 |
8.2 |
1.9 |
29% |
| Switzerland (CH) |
3.2 |
5.5 |
2.3 |
72% |
| France (FR) |
4.7 |
5.1 |
0.3 |
7% |
| Italy (IT) |
3.5 |
4.9 |
1.4 |
39% |
| United Kingdom (GB) |
3.5 |
4.5 |
1.0 |
29% |
| Austria (AT) |
3.9 |
3.9 |
0.06 |
2% |
| The Netherlands (NL) |
3.1 |
3.5 |
0.4 |
12% |
| Germany (DE) |
1.6 |
2.2 |
0.6 |
38% |
Other countries also substantially increased
their organ donation efficiency over the 10-year study period, primarily due to
an increase in DBD activity, as demonstrated in Italy (+39%) and Germany
(+38%). While Germany has no DCD programme due to legal prohibition, Italy has
relatively few DCD donors compared with most other countries. In contrast, in
the Netherlands, the United Kingdom, and Switzerland, the proportion of DCD donors
among all donors increased steadily, with DCD accounting for almost half or
even more than half of all donors in 2023 (figure 1, table 1).
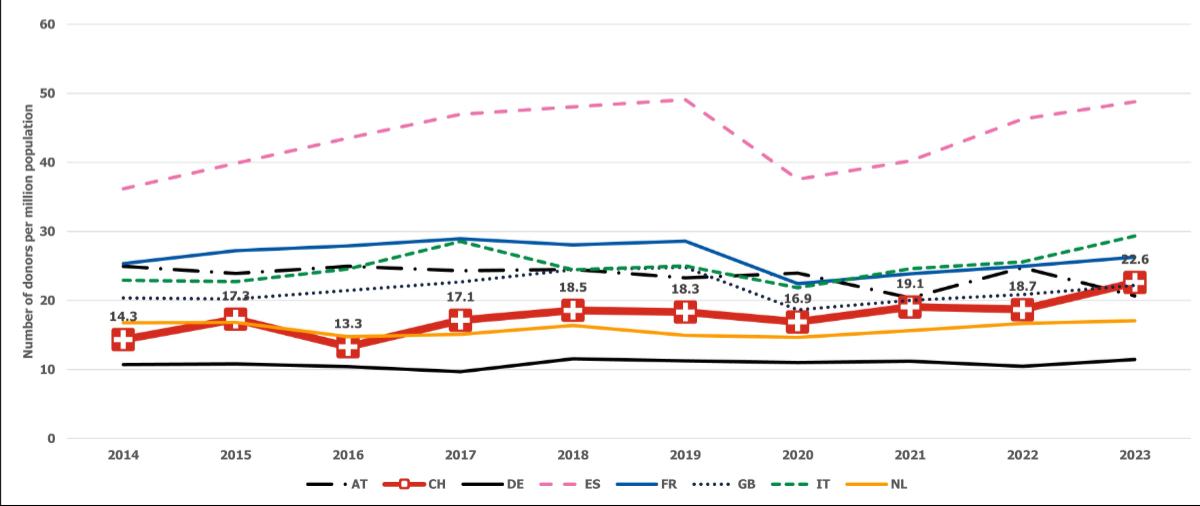
The DCI provides different results from the
donation rate pmp. For instance, the positive trend over the past decade is
less pronounced for the donation rate than for the DCI. While the DCI increased
in all countries from 2014 to 2023 (by 2–72%), the organ donation rate
increased by 2–58%, and Austria's organ donation rate declined by 17% (figure 2).
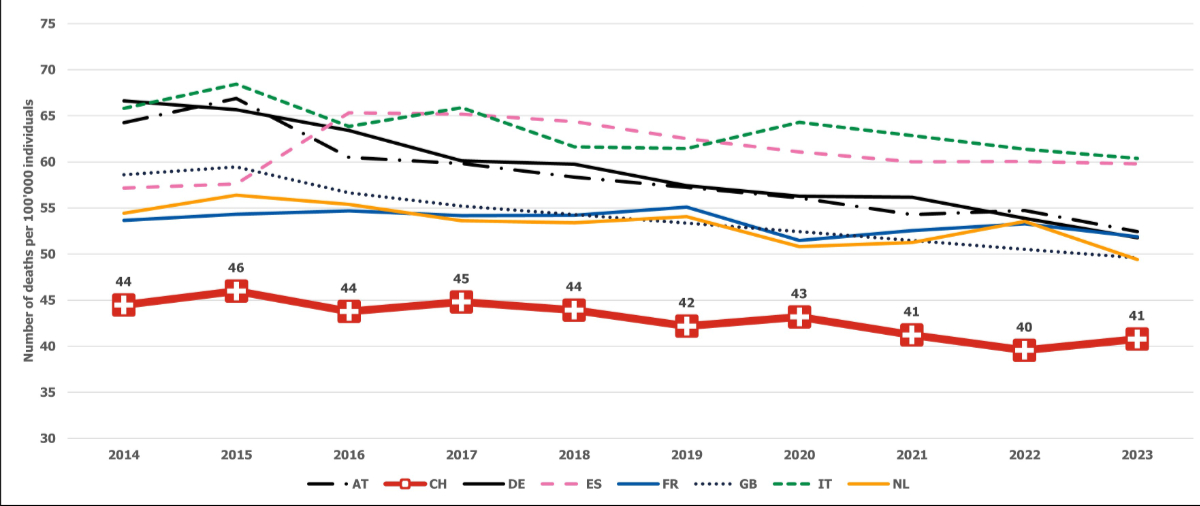
The divergent evolution of the DCI and donation rate is accompanied by a decrease
in mortality from diseases associated with potentially devastating cerebral
lesions leading to brain death. Mortality also declined over the study period (except
in Spain) (figure 3). In Spain, the UK, and Switzerland, a previously positive
trend in organ donation efficiency halted in 2020. A similar drop in efficiency
was observed in France and Italy during the same period (figure 1).
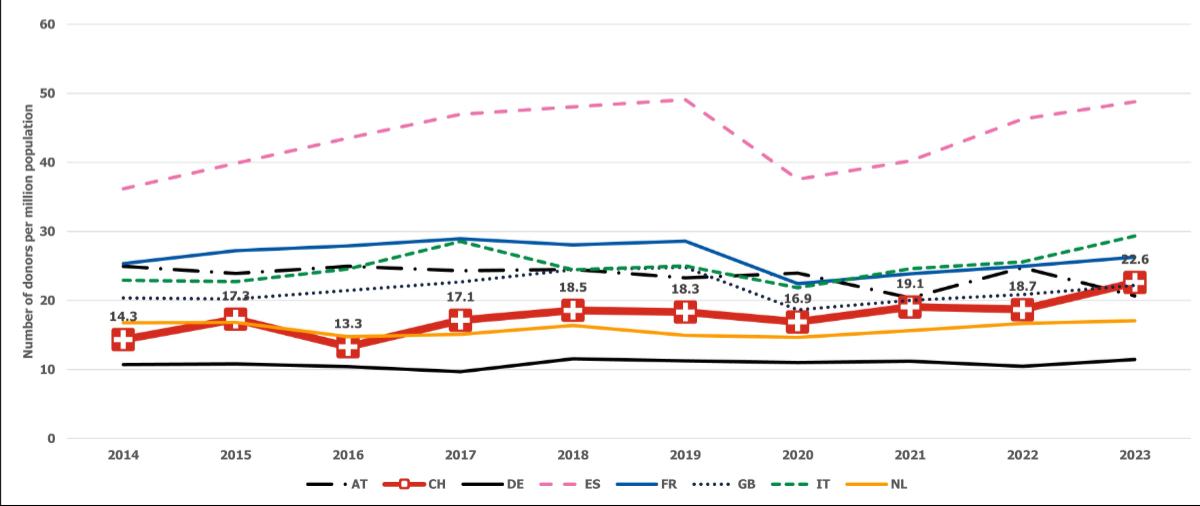
Figure 2Deceased organ donation rates per
million population (pmp). AT: Austria; CH: Switzerland; DE: Germany; ES: Spain;
FR: France; GB: the United Kingdom; IT: Italy; NL: the Netherlands.
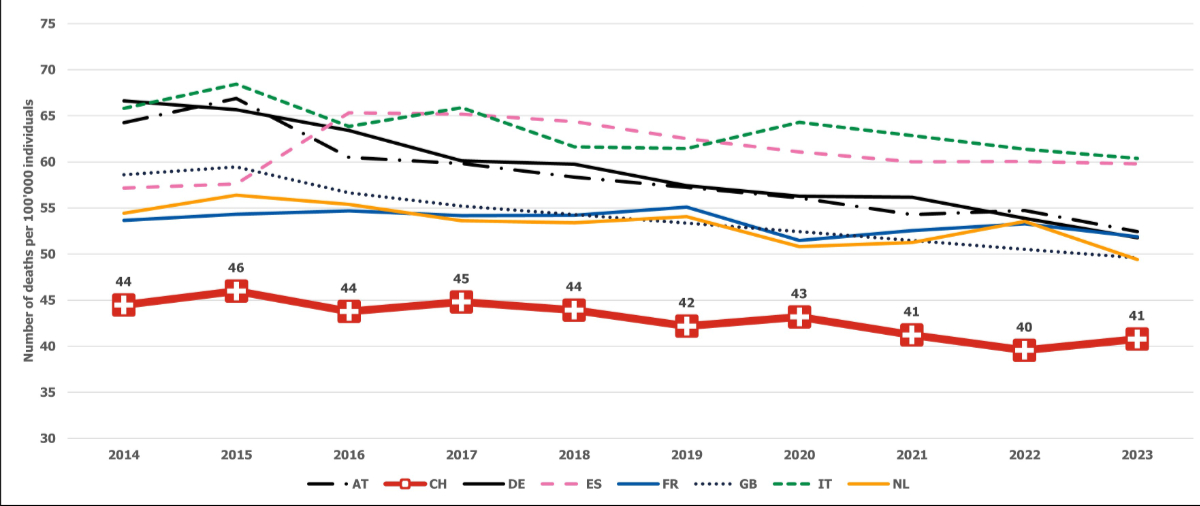
Figure 3Mortality rates of diseases
associated with potentially devastating cerebral lesions related to brain death
(not age-standardised deaths eligible for organ donation). AT: Austria; CH:
Switzerland; DE: Germany; ES: Spain; FR: France; GB: the United Kingdom; IT:
Italy; NL: the Netherlands.
Efficiency of national organ donation
programmes in 2023
A comparison of the countries at the conclusion
of the study period in 2023 reveals that the DCI presents a different picture
from simple donation rates. For instance, Switzerland's total DCI ranked second
among the countries analysed, following Spain, while in terms of donation rate
pmp, Switzerland ranked fourth, after Italy and France. Notably, although countries
such as Italy and France exhibit higher donation rates than Switzerland, their
DCI figures are lower (table 1 and table 2). This discrepancy is accompanied by
higher mortality rates in Italy and France for diseases associated with
potentially devastating cerebral lesions leading to brain death (figure 3). Switzerland
has fewer organ donors pmp than Italy and France, but its potential for organ
donation relative to the population is also lower. Consequently, as of 2023, Switzerland's
organ donation programme is more efficient than those of Italy and France, given
Switzerland’s comparatively lower organ donor potential.
Table 2Organ donation activity (number of donors per million population [pmp]) and
efficiency (donor conversion index [DCI]: number of donors per 100 eligible
deaths) at the end of the study period in 2023. Countries are ranked by
activity; in the right-most column, which presents each country’s rank by
efficiency, the difference from the activity ranking is shown in brackets.
| Country |
Activity |
Efficiency |
| |
pmp |
Rank |
DCI |
Rank |
| Spain (ES) |
48.8 |
1 |
8.2 |
1 |
| Italy (IT) |
29.3 |
2 |
4.9 |
4 (−2) |
| France (FR) |
26.3 |
3 |
5.1 |
3 |
| Switzerland (CH) |
22.6 |
4 |
5.5 |
2 (+2) |
| United Kingdom (GB) |
22.2 |
5 |
4.5 |
5 |
| Austria (AT) |
20.6 |
6 |
3.9 |
6 |
| The Netherlands (NL) |
17.1 |
7 |
3.5 |
7 |
| Germany (DE) |
11.4 |
8 |
2.2 |
8 |
Figure 3 also shows that Switzerland had the
lowest organ donation-eligible mortality rate of all countries throughout the
study period. In 2023, Switzerland recorded 41 eligible deaths per 100,000
individuals, compared with 49 to 60 eligible deaths per 100,000 individuals in the
other countries analysed. Since 2015/2016, mortality from organ donation-eligible
diseases declined in all countries, with an average decrease of approximately 10%.
This decline reflects a reduction in the potential for organ donation, as fewer
individuals die from causes associated with potentially devastating cerebral injury
leading to brain death.
Discussion
The increase in Switzerland’s organ donation
efficiency from 2014 to 2023 is encouraging. Overall efficiency, measured as the
number of donors per 100 eligible deaths, increased by 72% over the 10-year
period, representing the greatest increase among the nations analysed. At the
conclusion of the study period in 2023, Switzerland’s deceased donation programme
ranked among the most efficient in Europe, second only to Spain. This suggests
that Swiss emergency and ICU staff effectively identify, refer, and manage potential
deceased organ donors.
This positive trend is mainly attributable to a
significant increase in DCD activity since 2016. DCD activity increased 6.75-fold
over seven years, while DBD activity has remained relatively stable since 2014.
The stability of DBD activity despite the rise in DCD activity is noteworthy,
as there were initial concerns that the introduction of DCD would come at the
expense of DBD activity. Switzerland, along with other countries such as Spain
and the UK, demonstrates that this does not necessarily have to be the case.
DCD programmes were reintroduced in 2011 and
subsequently promoted by Swisstransplant and the National Committee for Organ
Donation in numerous hospitals. To date, 10 out of 14 organ procurement
hospitals have established a DCD programme, and 3 more are in the process of doing
so. In addition, other measures have been undertaken in Switzerland to increase
the efficiency of deceased organ donation. The national action plan "More
organs for transplants" (2013–2021) [18, 19] is regarded as a fundamental prerequisite
for various initiatives, including the promotion of DCD.
This plan established the necessary structures and resources to develop and
implement specific measures. The action plan comprised four fields of action: (1)
training healthcare professionals; (2) process and quality management; (3) hospital
structures and resources; and (4) public awareness campaigns and public
relations. Each of these was implemented as a sub-project. The first three
sub-projects were led by Swisstransplant and the National Committee for Organ
Donation (CNDO), while the fourth was led by the Federal Office of Public
Health. The effectiveness of such fundamental national measures typically becomes
apparent only after a delay. Our results are consistent with the intended
impact of the national action plan.
Swiss Monitoring of Potential Donors (SwissPOD)
may have also contributed to the positive developments observed in Switzerland.
Since 2012, this quality assurance tool has facilitated the ongoing evaluation
and improvement of donation processes at the hospital level and promoted awareness
of deceased organ donation among critical care personnel in hospitals [9]. In 2021,
Swisstransplant developed
and introduced the Donor Evaluation Tool. This digital tool supports local
hospital organ donation coordinators in reporting potential donors to
Swisstransplant and assists with eligibility decisions in uncertain or complex
donor cases, potentially increasing the number of actual donations. For
example, in 2022, more than 50% of potential donors assessed and initially accepted
through the tool became actual donors [20].
In Switzerland, consent for organ donation from
the deceased is required, and this is discussed with the next of kin at the
donor hospital. If the wishes of the deceased are unknown, the next of kin must
be asked on their behalf. Since 2021, Switzerland’s consent rate in approaches involving
next of kin (number of consents divided by the number of next-of-kin
approaches) has been declining. By 2023 (the end of the study period), only 42%
of these approaches resulted in consent to organ donation, while in 58% of
cases, organ donation was refused [21]. Compared with other countries, Switzerland’s
refusal rate is high; most
analysed countries reported lower refusal rates (Germany, 46%; the Netherlands,
45%; the UK, 39%; Italy, 30%; and Spain, 19%; no data are available for Austria
and France) [22]. Switzerland’s encouraging efficiency figures must be interpreted
in
light of these relatively high refusal rates. If Switzerland’s refusal rate were
comparable to those of other countries, the efficiency of the deceased organ
donation programme could be even higher. On 15 May 2022, the Swiss population
voted to introduce an opt-out system (also known as deemed or presumed consent),
and refusal rates are expected to decline once this system comes into force. Additional
measures have also been proposed in the literature to reduce refusal rates in next-of-kin
approaches, including the introduction of specialised nurses [23, 24].
Our results suggest that deceased organ
donation programmes should not be assessed solely by their donation rate pmp, which
reflects donation activity rather than efficiency. While the prevailing
donation rate pmp reflects national donation activity, the DCI metric better reflects
national donation efficiency by accounting for variations in mortality from
diseases associated with potentially devastating cerebral injury leading to
brain death. Mortality rates due to these causes differ substantially between Western
European countries and have continued to decline over time. Therefore, the
potential for organ donation does not represent the same proportion of the total
population in each country, and in all analysed countries, this potential has
been shrinking since 2016. When assessing and comparing organ donation
efficiency, differences in donor potential must be considered, as is the case in
the DCI approach. The DCI approach reduces this bias and enables fairer
comparisons. This is particularly important for countries such as Switzerland, which
has a relatively low mortality rate from diseases associated with potentially
devastating cerebral injury leading to brain death.
We observed a decline in donation efficiency in
2020 across most countries, which we attributed to the global COVID-19
pandemic. This temporary decrease is most likely due to the restriction or
suspension of donation processes during the pandemic, rather than an increase
in organ donation-specific mortality. An analysis of mortality data revealed no
evident impact of the pandemic on the number of deaths eligible for organ
donation.
Strengths and limitations of the study
The DCI accounts for variation in mortality
from eligible diseases by country and over time, enabling a less biased comparison
of the evolution of deceased organ donation activity across countries compared with
the simple comparison of donation rates pmp. In other words, the DCI allows for
a comparison of donation efficiency rather than donation activity. Furthermore,
the DCI is easy to understand, as donation efficiency is expressed as the
percentage of donors among eligible deaths. Finally, the required data are readily
available from standardised databases in many countries, and the ICD classification
is widely accepted worldwide.
The DCI concept is based on diseases associated
with potentially devastating cerebral injury leading to brain death. However,
potential donors for DCD are not limited to these patients; they also include individuals
with circulatory failure who are medically suitable for organ donation. This
means that the DCI may slightly overestimate donation efficiency in countries
with a high proportion of DCD, as these countries have more actual donors (numerator)
who may not be fully represented by the number of eligible deaths (denominator).
In the case of controlled DCD, in which cardiac arrest is planned and expected
following the withdrawal of life-sustaining therapy, we estimate that approximately
95% of deaths are captured by the DCI. This is because controlled DCD cases are
mostly associated with underlying conditions that also cause potentially
devastating brain injury leading to brain death. For example, 2023 data from
the Swiss Organ Allocation System show that 56% of DCD donors died from anoxia,
29% from cerebrovascular accidents, 9% from traumatic brain injury, and only 5%
from other causes [25]. It is assumed that in countries where controlled DCD predominates,
the
distribution of causes of death among DCD donors is relatively uniform. Therefore,
the bias introduced by the DCI, specifically the potential to overestimate donation
efficiency when comparing countries, is expected to be minimal. However, the
DCI may somewhat overestimate donation efficiency in countries where
uncontrolled DCD is common, such as France and Spain, because a higher
proportion of actual donors in those countries are not captured by the number
of eligible deaths used in the denominator. Uncontrolled DCD refers to donation
from individuals who die following an unexpected cardiac arrest and cannot be
successfully resuscitated [26].
It should also be noted that statistics on
causes of death are only available with a two-year delay. To ensure data
timeliness, figures for the most recent years had to be imputed (2022: three
countries; 2023: all eight countries). Notably, due to the UK's exit from the
EU, data for the UK were only available until 2018 and were imputed for 2019 to
2023. In addition, the ICD-10 codes that define traumatic brain injury, as
listed in table 2.3 of the EDQM’s Guide to the Quality and Safety of Organs
for Transplantation [14], were not available from Eurostat. As a proxy, transport accidents were
used instead.
Conclusion
The DCI clearly demonstrates Switzerland’s high
donation efficiency compared with other European countries. Despite declining consent
rates in next-of-kin approaches, Switzerland's
organ donation programme remains among the most efficient in Europe, according
to the DCI. If consent rates were comparable to those in other countries,
overall efficiency could be even higher. The data indicate that Swiss emergency and
intensive
care staff effectively identify, refer, and manage potential deceased organ
donors and suggest that measures implemented in recent years to increase organ
donation rates have been effective. When comparing organ donation trends across
countries, it is important to consider differences in mortality from diseases
associated with potentially devastating cerebral injury leading to brain death.
Data sharing statement
The data used for this study are publicly
available. Corresponding contacts or internet addresses are referenced in the
Materials and methods section. Any code used for data cleaning and processing
is available from the corresponding author upon request.
Acknowledgments
The authors would like to thank the National Committee
for Organ Donation (CNDO) and the five Swiss organ donation networks for their
continuous support in establishing and implementing the standardised clinical
procedures for organ donation in Switzerland.
Franz F. Immer, MD
consultant cardiovascular
surgeon FMH
Swisstransplant
Effingerstr 1
CH-3011 Bern
franz.immer[at]swisstransplant.ch
References
1. DeRoos LJ, Zhou Y, Marrero WJ, Tapper EB, Sonnenday CJ, Lavieri MS, et al. Assessment
of National Organ Donation Rates and Organ Procurement Organization Metrics. JAMA
Surg. 2021 Feb;156(2):173–80. doi: https://doi.org/10.1001/jamasurg.2020.5395
2. Quality of Medicines & HealthCare of the Council of Europe (EDQM). Guide to the quality
and safety of organs for transplantation - 9th Edition [Internet]. 9th ed. Strasbourg:
COUNCIL OF EUROPE; 2025 [cited 2025 May 13]. Available from: www.edqm.eu/store
3. Wight C, Cohen B, Beasley C, Miranda B, Deblander G. Donor action: a systematic approach
to organ donation. Transplant Proc. 1998 Aug;30(5):2253–4. doi: https://doi.org/10.1016/S0041-1345(98)00609-5
4. Wight C Sr, Cohen B, Roels L, Miranda B. Donor Action: A Quality Assurance Program
for Intensive Care Units That Increases Organ Donation. J Intensive Care Med. 2000 Mar;15(2):104–14.
doi: https://doi.org/10.1177/088506660001500204
5. Roels L, Wight C Sr. Donor Action: an international initiative to alleviate organ
shortage. Prog Transplant. 2001 Jun;11(2):90–7. doi: https://doi.org/10.1177/152692480101100203
6. Roels L, Spaight C, Smits J, Cohen B. Donation patterns in four European countries:
data from the donor action database. Transplantation. 2008 Dec;86(12):1738–43. doi: https://doi.org/10.1097/TP.0b013e3181908e08
7. Domínguez-Gil B, Delmonico FL, Shaheen FA, Matesanz R, O’Connor K, Minina M, et al. The
critical pathway for deceased donation: reportable uniformity in the approach to deceased
donation. Transpl Int. 2011 Apr;24(4):373–8. doi: https://doi.org/10.1111/j.1432-2277.2011.01243.x
8. Weiss JH, Keel I, Immer FF, Wiegand J, Haberthür C; Comité National du Don d’Organes
(CNDO). Swiss Monitoring of Potential Organ Donors (SwissPOD): a prospective 12-month
cohort study of all adult ICU deaths in Switzerland. Swiss Med Wkly. 2014 Oct;144(4344):w14045.
doi: https://doi.org/10.4414/smw.2014.14045
9. Swisstransplant. SwissPOD [Internet]. 2024 [cited 2024 Nov 25]. Available from: https://www.swisstransplant.org/de/organ-gewebespende/fakten-und-zahlen/swiss-pod-reporting
10. Weiss J, Elmer A, Mahíllo B, Domínguez-Gil B, Avsec D, Nanni Costa A, et al.; Council
of Europe European Committee on Organ Transplantation (CD-P-TO). Evolution of Deceased
Organ Donation Activity Versus Efficiency Over a 15-year Period: An International
Comparison. Transplantation. 2018 Oct;102(10):1768–78. doi: https://doi.org/10.1097/TP.0000000000002226
11. Coppen R, Friele RD, Gevers SK, Blok GA, van der Zee J. The impact of donor policies
in Europe: a steady increase, but not everywhere. BMC Health Serv Res. 2008 Nov;8(1):235.
doi: https://doi.org/10.1186/1472-6963-8-235
12. Bendorf A, Kerridge IH, Kelly PJ, Pussell B, Guasch X. Explaining failure through
success: a critical analysis of reduction in road and stroke deaths as an explanation
for Australia’s low deceased organ donation rates. Intern Med J. 2012 Aug;42(8):866–73.
doi: https://doi.org/10.1111/j.1445-5994.2012.02792.x
13. Weiss J, Elmer A, Béchir M, Brunner C, Eckert P, Endermann S, et al.; Comité National
du Don d’Organes (CNDO). Deceased organ donation activity and efficiency in Switzerland
between 2008 and 2017: achievements and future challenges. BMC Health Serv Res. 2018 Nov;18(1):876.
doi: https://doi.org/10.1186/s12913-018-3691-8
14. Quality of Medicines & HealthCare of the Council of Europe (EDQM). Guide to the quality
and safety of organs for transplantation – 8th Edition [Internet]. 8th ed. Strasbourg:
COUNCIL OF EUROPE; 2022. Available from: www.edqm.eu
15. Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al.; RECORD
Working Committee. The REporting of studies Conducted using Observational Routinely-collected
health Data (RECORD) statement. PLoS Med. 2015 Oct;12(10):e1001885. doi: https://doi.org/10.1371/journal.pmed.1001885
16. The World Health Organization (WHO), The Spanish Transplant Organization, Organización
Nacional de Trasplantes (ONT). Global Observatory on Donation and Transplantation
(GODT) [Internet]. Global database on donation and transplantation. 2025 [cited 2025
Feb 11]. Available from: https://www.transplant-observatory.org/data-charts-and-tables/
17. Eurostat. Population on 1 January [Internet]. Eurostat Data Browser [cited 2025 Feb
13]. Available from: https://ec.europa.eu/eurostat/data/database
18. Bundesamt für Gesundheit. Wirkungsmodell Aktionsplan ‘Mehr Organe für Transplantationen’
[Internet]. 2013. Available from: https://www.bag.admin.ch/dam/bag/de/dokumente/biomed/transplantationsmedizin/wirkungsmodell-aktionsplan-mehr-organe.pdf.download.pdf/wirkungsmodell-aktionsplan-mehr-organe.pdf
19. Bundesamt für Gesundheit. Wirkungsmodell Aktionsplan ``Mehr Organe für Transplantationen’’
2019-2021 [Internet]. 2018. Available from: https://www.bag.admin.ch/dam/bag/de/dokumente/biomed/transplantationsmedizin/wirkungsmodell-aktionsplan-mehr-organe-2019-2021.pdf.download.pdf/bag_faktenblatt_wirkungsmodell_aktionsplan_de_v02.pdf
20. Imbimbo C, Nauwerk M, Cammarota T, Beyeler F, Krügel N, Elmer A, et al. Donor Evaluation
Tool: A New Technology Improves Donor Enrolment on ICU. Transpl Int. 2024 Jul;37:12227.
doi: https://doi.org/10.3389/ti.2024.12227
21. Swisstransplant. SwissPOD (Swiss Monitoring of Potential Donors) Report 2024 [Internet].
2025 Apr [cited 2025 Apr 11]. Available from: https://www.swisstransplant.org/fileadmin/user_upload/SwissPOD_Reporting_2024_DE_Schweiz.pdf
22. Global Observatory on Donation and Transplantation (GODT). International Report on
Organ Donation and Transplantation Activities. December 2024 [Internet]. 2024 Dec
[cited 2025 Mar 17]. Available from: https://www.transplant-observatory.org/wp-content/uploads/2025/02/2023-data-global-report-20022025.pdf
23. Singh JM, Ball IM, Hartwick M, Malus E, Soliman K, Boyd JG, et al. Factors associated
with consent for organ donation: a retrospective population-based study. CMAJ. 2021 Nov;193(45):E1725–32.
doi: https://doi.org/10.1503/cmaj.210836
24. Radford S, D’Costa R, Opdam H, McDonald M, Jones D, Bailey M, et al. The impact of
organ donation specialists on consent rate in challenging organ donation conversations.
Crit Care Resusc. 2023 Oct;22(4):297–302. doi: https://doi.org/10.51893/2020.4.OA1
25. Swisstransplant. Jahresbericht 2023 [2023 annual report] [Internet]. 2024. Available
from: https://www.swisstransplant.org/de/swisstransplant/jahresbericht
26. Coll E, Miñambres E, Sánchez-Fructuoso A, Fondevila C, Campo-Cañaveral de la Cruz JL,
Domínguez-Gil B. Uncontrolled Donation After Circulatory Death: A Unique Opportunity.
Transplantation. 2020 Aug;104(8):1542–52. doi: https://doi.org/10.1097/TP.0000000000003139