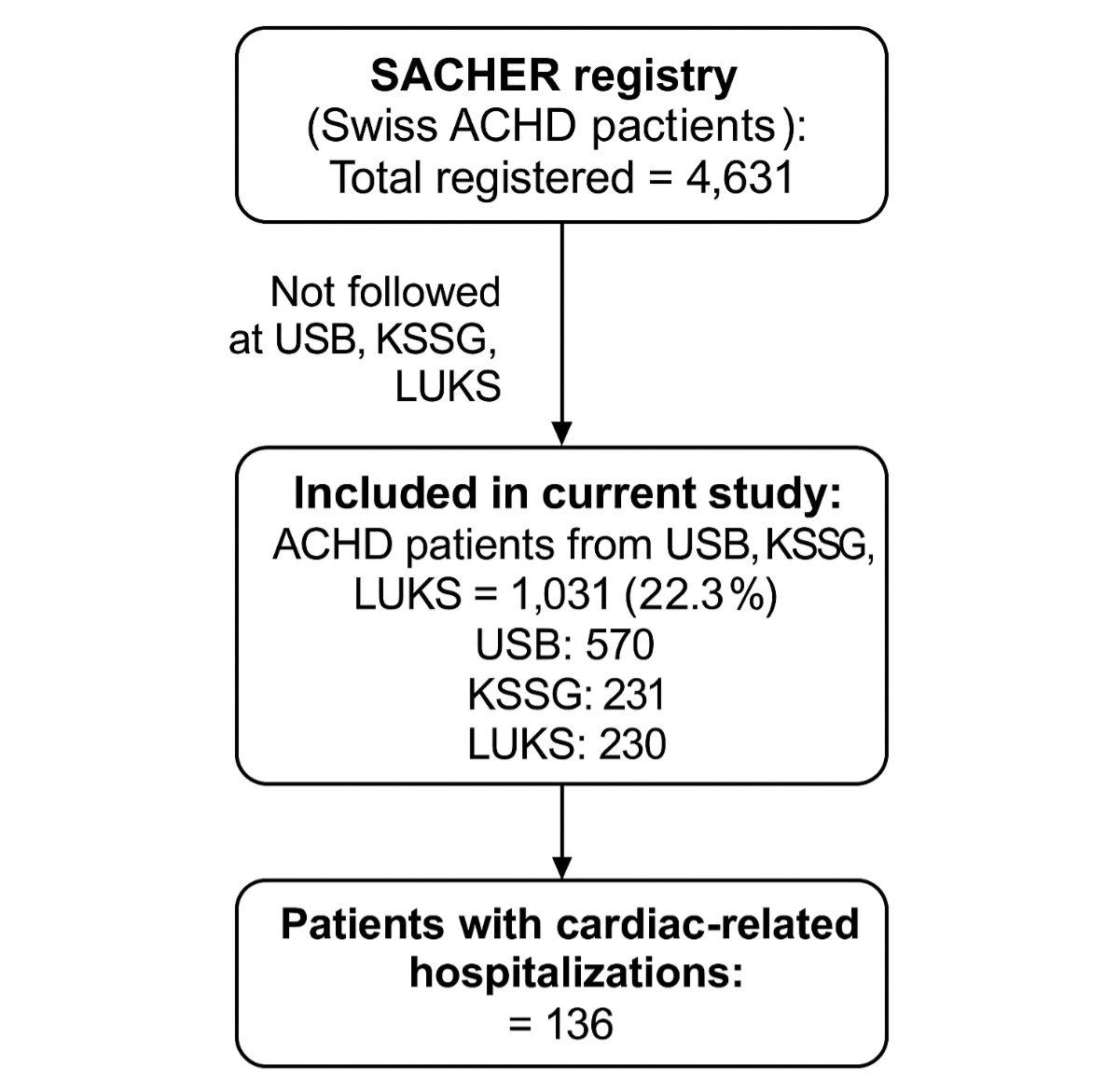
Figure 1Patient cohort.
DOI: https://doi.org/https://doi.org/10.57187/s.4459
Adults with congenital heart disease present a rapidly growing patient cohort in adult cardiology. Due to improvements in all aspects of care, starting with prenatal screening [1], evolving surgical techniques and overall progress in medical care over the last few decades, today the majority of patients with congenital heart disease (CHD) reach adulthood [2]. Although most patients have undergone surgical repair in childhood, they are not cured and need lifelong specialist care as they are at risk of cardiac complications and many require further interventions.
The Swiss Working Group for Adults and Teenagers with Congenital Heart Disease (WATCH) has published recommendations for standards of care of adult congenital heart disease (ACHD) patients in Switzerland [3]. Treatment facilities for adult congenital heart disease patients have been categorised as regional and supraregional ACHD centres. All ACHD centres collaborate with paediatric cardiology services and have a structured transition process. Infrastructural and staff requirements differ between regional and supraregional centres and the key difference is the provision of highly specialised interventions (such as congenital heart surgery and complex cardiac percutaneous interventions) and access to the heart transplant programme among the supraregional ones.
Since the publication of these national recommendations, a comprehensive description of cardiac-related hospitalisations, including their causes and management among patients followed at regional ACHD centres in Switzerland, has not yet been published. We therefore aimed to assess the extent of cardiac-related hospitalisations in adult congenital heart disease patients followed at Swiss regional ACHD centres. Such data may help in defining requirements for resource allocation for optimal care of patients with adult congenital heart disease in Switzerland.
For this study, adult congenital heart disease patients from regional ACHD centres (University Hospital Basel [Universitätsspital Basel], St Gallen Cantonal Hospital [Kantonsspital St Gallen] and Lucerne Cantonal Hospital [Luzerner Kantonsspital]) enrolled in the SACHER registry were analysed (figure 1). Patients enrolled in the SACHER registry who were not being followed at one of the above-mentioned centres were excluded. The SACHER registry (Swiss Adult Congenital HEart disease Registry; www.sacher-registry.com; ClinicalTrials.gov Identifier NCT2258724) is a nationwide prospective cohort study of adult patients with congenital heart disease. Patient inclusion into the registry began in May 2014. For the purposes of our analysis, follow-up data for the period from 1 January to 31 March 2022 were reviewed. The follow-up period was calculated from the date of enrolment of each patient to a fixed administrative censoring date of 31 March 2022. Patients were followed and treated by pre-specified care protocols complying with national and international recommendations [4]. Adverse events were prospectively collected. Details on the structure and protocols of the registry have previously been published [5].
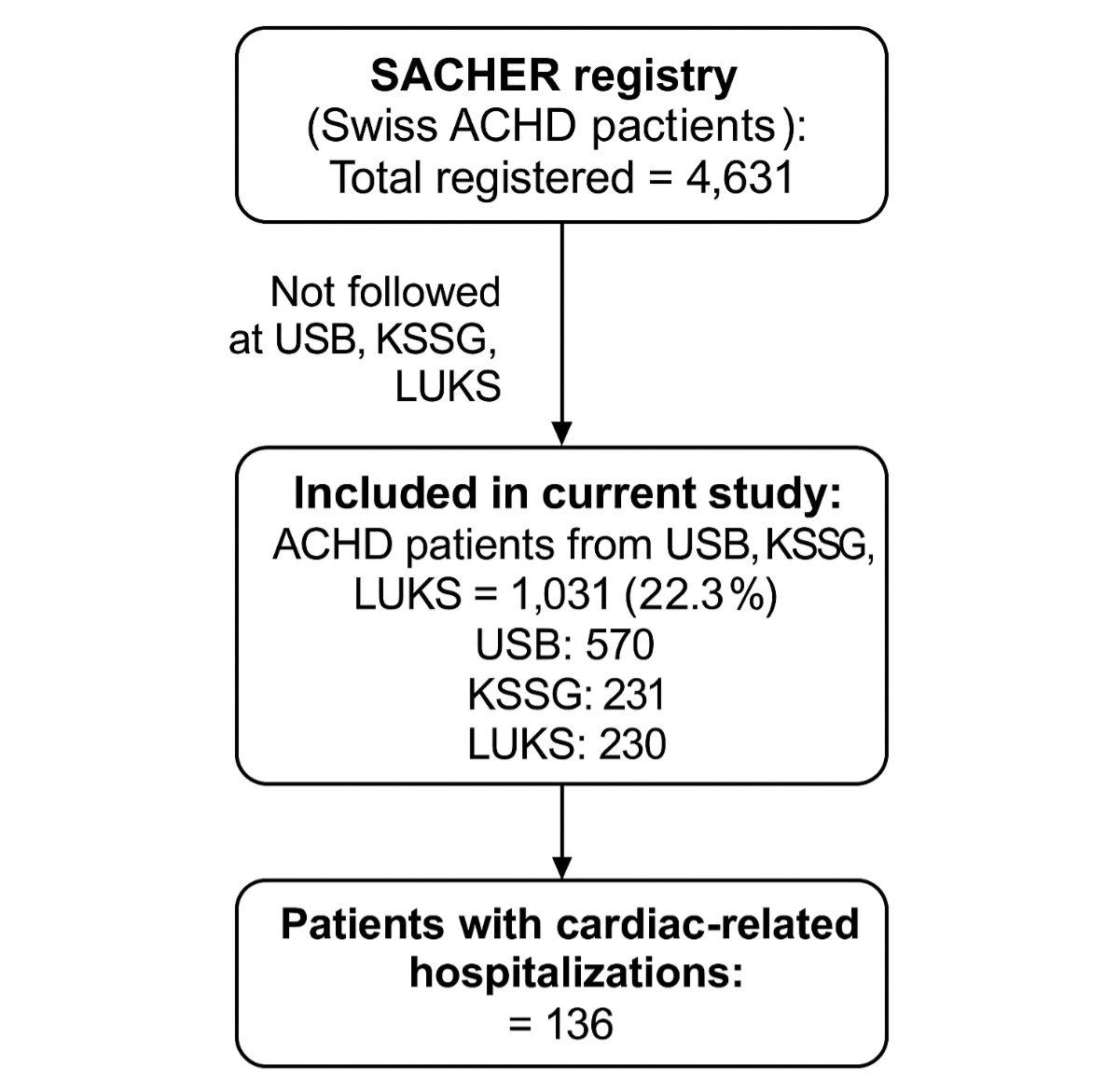
Figure 1Patient cohort.
For each patient, the first documented clinical visit in the registry was defined as the baseline visit. The last documented clinical visit was regarded as the follow-up appointment. Data of participants were encoded with pseudonyms and collected in an electronic, web-based database (secuTrial®). All patients had given written informed consent, and the study was approved by the local ethics committees.
Baseline characteristics were extracted from the SACHER registry and included demographic data as well as data about cardiac anatomy and function, surgical and medical history as well as congenital heart disease complexity. Categorisation into mild, moderate and severe was done according to current guidelines [4]. Diagnoses were grouped according to given working diagnoses [5].
Adverse cardiac outcome and hospitalisation data were collected by local chart review. They included all recorded adverse cardiac events that occurred between the time of inclusion into the study and the last recorded physician or hospital visit within the study period. We included date of hospitalisation, place of management (regional vs supraregional) and reason for hospitalisation (elective vs emergency).
The primary outcome was the occurrence of a cardiac-related hospital admission (elective and emergency visit, for heart surgery or cardiac interventions, or for other predefined cardiac complications). The following events were considered cardiac-related interventions: any form of interventional percutaneous valve replacement, ablation procedures for the treatment of arrhythmias, percutaneous interventions other than ablation procedures, and cardiac device placement/replacement.
The following events were considered cardiac-related complications: cardiac-related death, heart failure requiring hospitalisation, sustained supraventricular/ventricular tachycardia requiring anti-arrhythmic treatment or hospitalisation, myocardial infarction, stroke and infective endocarditis.
Analyses were performed in R v4.4.0 (R Foundation for Statistical Computing, Vienna, Austria). As continuous variables did not follow a normal distribution (based on Shapiro-Wilk tests), they are presented as medians with interquartile ranges (IQR) and were compared using the Mann-Whitney U test. Categorical variables are presented as counts with percentages and compared by means of the chi-squared test. One patient had a missing date of inclusion and was excluded from follow-up and incidence rate analyses. Additionally, 13 hospitalisation records lacked hospitalisation dates, and 13 patients had missing data on congenital heart disease complexity. These patients were excluded from the corresponding analysis in table 1. Two-sided p-values <0.05 were considered significant.
Table 1Patient cohort.
| Cardiovascular-related hospitalisation | No (n = 895) | Yes (n = 136) | p-value* | |
| Age in years at first cardiovascular-related hospitalisation, median (Q1, Q3) | – | 37 (25, 49) | ||
| ... Unknown, n | 895 | 13 | ||
| Age in years at baseline, median (Q1, Q3) | 27 (22, 35) | 36 (23, 47) | <0.001 | |
| ... Unknown, n | 351 | 31 | ||
| Congenital heart disease complexity | <0.001 | |||
| ... Simple, n (%) | 466 (53) | 47 (35) | ||
| ... Moderate, n (%) | 322 (36) | 56 (42) | ||
| ... Severe, n (%) | 96 (11) | 31 (23) | ||
| ... Unknown, n | 11 | 2 | ||
| Hospitalisation type | ||||
| ... Elective, n (% of type total) | 61 (44.5) | 76 (55.5) | <0.001 | |
| ... Emergency, n (% of type total) | 19 (19) | 81 (81) | ||
| Treating centre | <0.001 | |||
| ... St Gallen Cantonal Hospital, n (%) | 191 (21) | 40 (29) | ||
| ... Lucerne Cantonal Hospital, n (%) | 218 (24) | 12 (9) | ||
| ... University Hospital Basel, n (%) | 486 (54) | 84 (62) | ||
* Wilcoxon rank-sum test; Pearson’s chi-squared test
Overall, 1031 adult congenital heart disease patients were included (570 at University Hospital Basel, 231 at St Gallen Cantonal Hospital and 230 at Lucerne Cantonal Hospital), accounting for 22.3% of the 4631 Swiss adult congenital heart disease patients included in SACHER. The median (IQR) age at baseline was 29 years (22–40) and 475 patients (40%) were female. The median (IQR) follow-up duration was 6.40 years (4.75–7.72). The 1031 patients contributed a cumulative total of 6008 person-years of follow-up. During this period, there were 237 hospitalisations related to cardiovascular complications in 136 (13.2%) patients. This corresponds to a hospitalisation rate of 3.9 cardiovascular hospitalisations per 100 person-years. The follow-up duration varied significantly across participating centres (p <0.001). The median follow-up duration was longest at University Hospital Basel (7.4 years; IQR: 5.9–8.0), followed by St Gallen Cantonal Hospital (6.5 years; IQR: 4.8–7.3) then Lucerne Cantonal Hospital (4.7 years; IQR: 3.3–5.3).
The cardiac diagnosis groups of admitted patients are illustrated in figure 2. Baseline characteristics stratified by the occurrence of cardiac-related hospitalisation during follow-up are outlined in table 1. Patients meeting the primary outcome (those who experienced at least one cardiovascular-related hospitalisation during the follow-up) were older compared to those without hospitalisations – median (IQR) age of 36 [23–47] and 27 (22–35) years, respectively (p <0.001) – and had more complex congenital heart disease, with moderate or severe complexity accounting for 65% and 47% of patients, respectively (p <0.001). Overall, 157 (66%) of all hospitalisations were managed at the regional ACHD centres and 80 (34%) were admitted or transferred to supraregional ACHD centres. There were 100 (42%) emergency hospitalisations, of which 81 (81%) were managed locally at the corresponding regional ACHD centre. Of 137 (58%) elective hospitalisations, 61 (44.5%) occurred at supraregional ACHD centres. Reasons for hospitalisations in regional and supraregional ACHD centres are illustrated in figure 3.
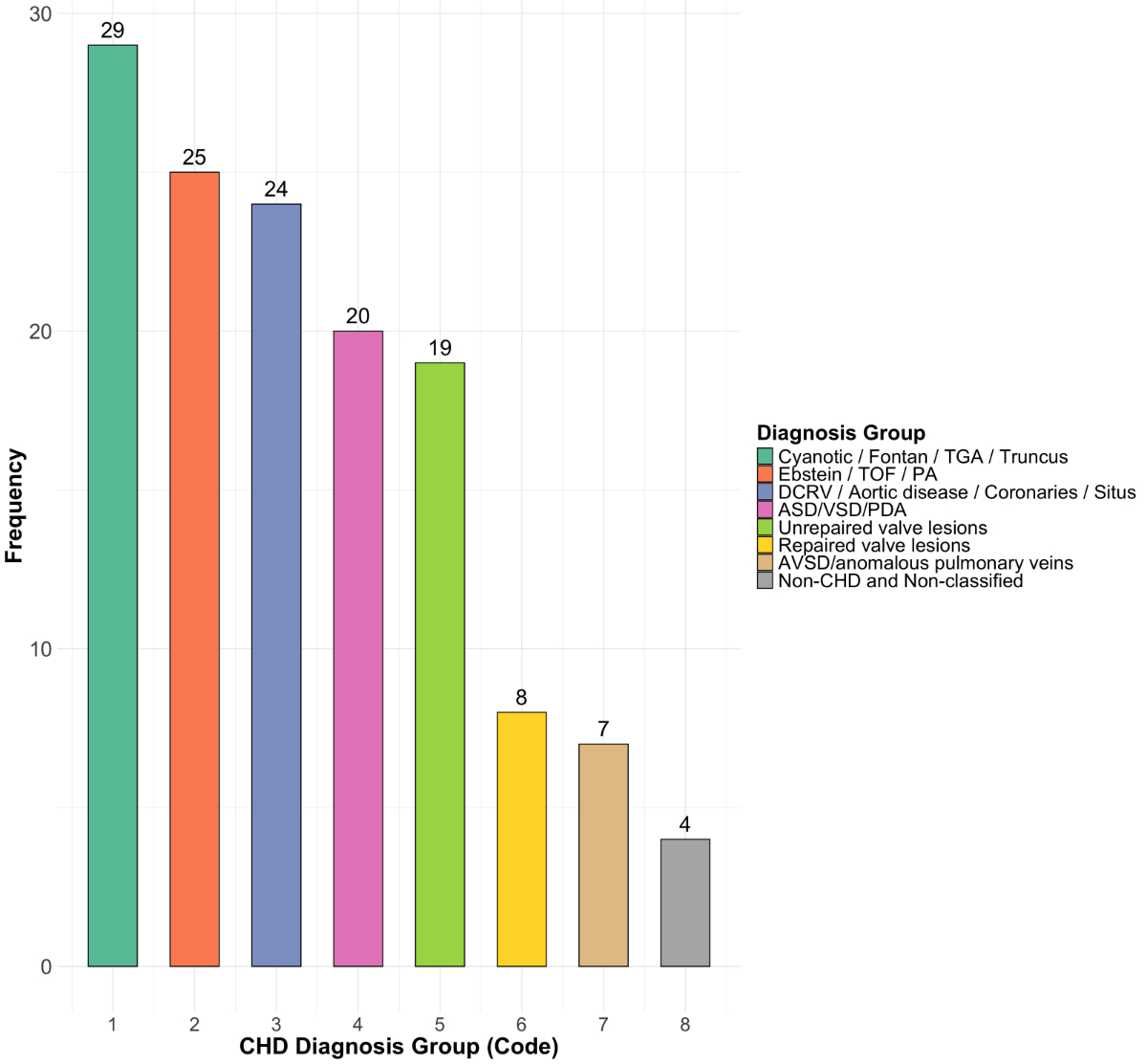
Figure 2Frequency of congenital heart disease diagnoses group (unique patients, n = 136) of admitted adult congenital heart disease (ACHD) patients. ASD: atrial septal defect; AVSD: atrioventricular septal defect; CHD: congenital heart defect; DCRV: double-chambered right ventricle; PA: pulmonary valve atresia; PDA: patent ductus arteriosus; TGA: transposition of the great arteries; TOF: tetralogy of Fallot; VSD: ventricular septal defect.
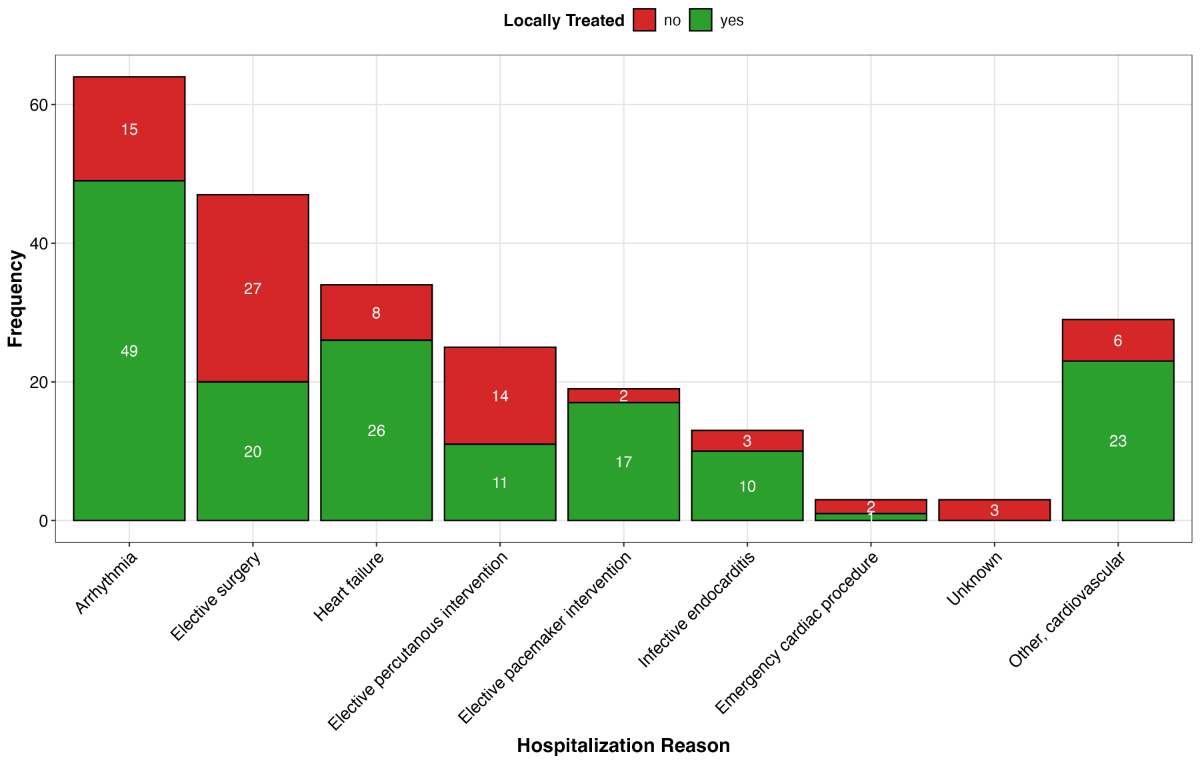
Figure 3Cardiac-related hospitalisations of adult congenital heart disease (ACHD) patients (n = 136) during follow-up. The X-axis presents the number of outcomes, the Y-axis states the type of cardiac outcome.
Arrhythmias leading to hospital admission were the most frequent cardiac-related complications. Of the 64 arrhythmia events, recorded in 37 patients, most were atrial flutter and intra-atrial re-entrant tachycardia (n = 26, 41%). Most arrhythmia events (n = 49, 77%) were managed locally at regional ACHD centres. In 31 cases (48%), arrhythmias led to an emergency admission, of which 24 (77%) were managed locally. Overall, 11 (17%) arrhythmia cases were managed with antiarrhythmic drugs, 18 (28%) by electrical cardioversion and 33 (52%) by interventional ablation procedures, of which 25 (76% of ablations) were performed at the regional ACHD centres.
The second most common reason for cardiac-related hospitalisation was heart failure (n = 34) in 14 patients. Most heart failure admissions were emergency admissions (n = 29, 85%), which were mainly managed in regional ACHD centres (25/29, 86%). One patient with a history of implantation of a mechanical aortic valve in childhood for congenital aortic valve stenosis was referred twice to the supraregional ACHD centre for acute heart failure. The patient was evaluated for heart transplantation at the supraregional ACHD centre. However he died at the regional ACHD centre due to heart failure. Other reasons of cardiac complications leading to an admission are displayed in figure 3.
During follow-up, 56 heart surgeries were performed. Of these, 32 (57%) were performed at supraregional ACHD centres. Most surgeries managed at supraregional centres were elective (29/32, 91%). The emergency referrals to a supraregional ACHD centre for heart surgery were all due to aortic dissection or pseudoaneurysm for aortic valve and aortic ascendens replacement. Elective reasons for referral to the supraregional centre were surgical treatment of the left ventricular outflow tract, aortic valve and aorta in 20 cases (subaortic myectomy, aortic cusp repair, aortic valve implantation, Ross procedure, replacement of the ascending aorta, aortic arch repair), pulmonary valve replacement in 5 cases, a Baffle repair in 1 case, surgery for shunt lesions in 4 cases and Other in 2 cases.
Facilities for open-heart surgery were available at two of the three regional centres participating in this study (University Hospital Basel and Lucerne Cantonal Hospital). The most common reasons for heart surgery at the regional ACHD centres were surgical treatment of the aortic valve and the aorta in 19 cases (aortic valve replacement in 14, Ross procedure in 1, David operation in 1, aorta-other in 3), surgery for shunt lesions in 2 cases and other in 2 cases.
Complex cardiac percutaneous interventions were exclusively performed at supraregional ACHD centres (3 pulmonary valve replacement procedures [3/3, 100%] and 7 balloon dilation of aortic coarctation procedures [7/7, 100%). Percutaneous interventions at the regional centres were performed for atrial septal defect (ASD) and patent ductus arteriosus (PDA) closure and coronary interventions.
Frequencies of surgical and interventional procedures in regional and supraregional ACHD centres are illustrated in figure 4.
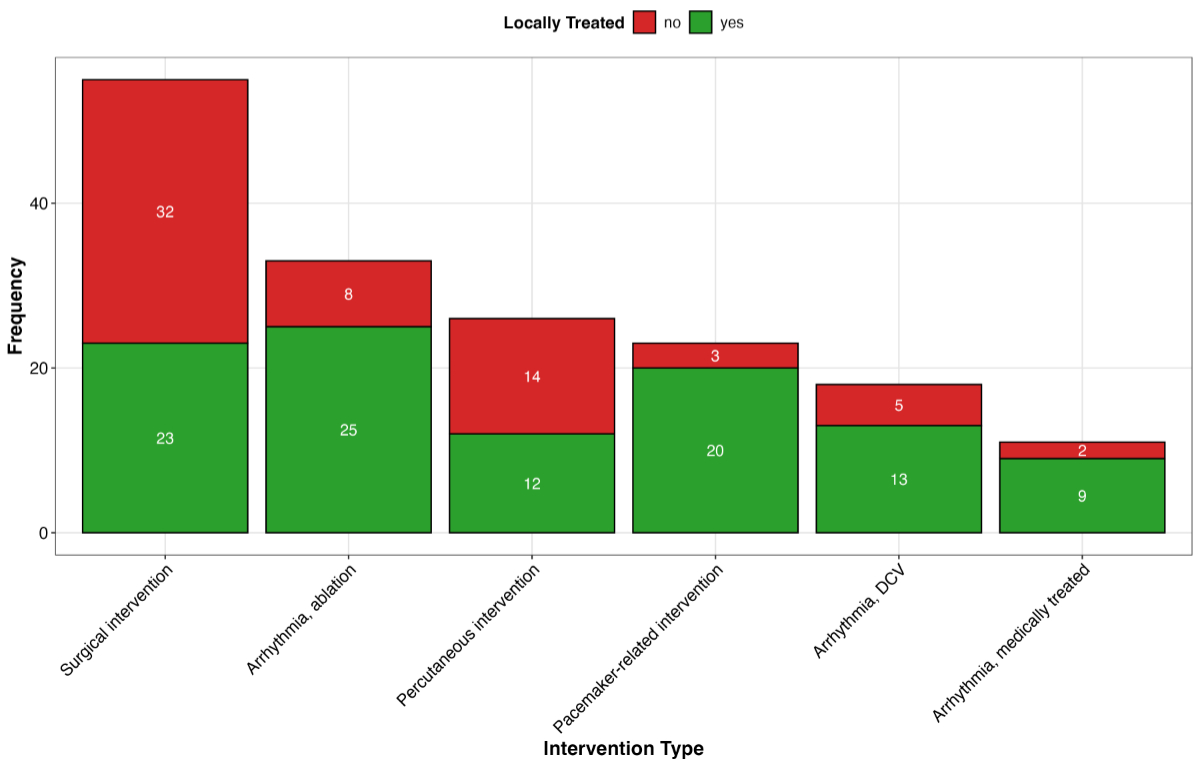
Figure 4Frequencies of interventions in adult congenital heart disease (ACHD) patients (n = 136) during follow-up. The X-axis presents the number of outcomes and the Y-axis states the type of cardiac outcome. DCV: Direct current cardioversion.
During follow-up, 16 (1.6%) patients died. Median (IQR) age at death was 47 (30–60) years. Of these patients, 8 (50%) died at regional ACHD centres, 3 (19%) at a supraregional ACHD centre and 5 (31%) out of hospital. The most frequent cause of death was cardiac-related death (heart failure in 6 [36%], sudden cardiac death in 4 [25%] and endocarditis in 1 [6%]); 1 death was periprocedural and 4 deaths were not cardiac-related. All 3 patients who died at a supraregional ACHD centre had severe disease complexity (transposition of the great arteries [TGA] after arterial switch operation; TGA after Mustard operation; congenital corrected TGA), and died after cardiac complications or complex surgery.
In this study, we explored cardiac-related hospitalisations of adult congenital heart disease patients followed at regional ACHD centres in Switzerland. About a quarter of adult congenital heart disease patients in Switzerland are mainly followed at regional ACHD centres; therefore these centres contribute substantially to overall care of this patient cohort. Although the patients studied in this cohort were young (mean age of 29 years at baseline) and follow-up was rather short (3 years), a substantial proportion (13%) required at least one hospitalisation. This highlights the complexity of this patient cohort. Most adult congenital heart disease patients who needed hospitalisation for cardiac reasons could be managed locally at regional ACHD centres. This was particularly true for emergency admissions and cardiac complications such as tachyarrhythmias and heart failure. Regarding heart surgery and percutaneous interventions, patients with aortic and aortic valve lesions such as aortic valve stenosis and thoracic aortic aneurysm and patients with simple shunt lesions were typically managed at the regional ACHD centres whereas complex percutaneous cardiac interventions such as interventional pulmonary valve replacement and dilation of aortic coarctation were exclusively performed at supraregional ACHD centres.
Our data highlight the importance of regional ACHD centres in the care of adult congenital heart disease patients in Switzerland. Half of the patients followed at regional ACHD centres have moderate or severe disease complexity (such as patients with a Fontan palliation, patients with a systemic right ventricle and patients with cyanotic heart disease) and therefore, as recommended by the Swiss Working Group for Adults and Teenagers with Congenital Heart Disease (WATCH), these centres need adequate staff and institutional requirements such as dedicated adult congenital heart disease specialists, an adult congenital heart disease outpatient clinic, as well as 24/7 access to an emergency service, general adult medicine inpatient unit and an intensive care unit. It must be emphasised that well-trained adult congenital heart disease specialists are needed not only in supraregional centres, but also in regional centres in order to optimise patient care and coordination with supraregional centres. According to the Swiss recommendation on adult congenital heart disease care, adult congenital heart disease cardiologists must have a nationally recognised certification in Cardiology or Paediatric Cardiology with a minimal educational training of 24 months in adult congenital heart disease. These 24 months should include at least 18 months in a supraregional ACHD centre and can be complemented by 6 months in adult cardiology for paediatric cardiology trainees and 6 months of paediatric cardiology for adult cardiology trainees [3].
As most arrhythmias and heart failure complications have been treated locally, collaboration with dedicated specialists in other disciplines, such as cardiac imaging, electrophysiology and heart failure is crucial.
Close cooperation and collaboration between regional and supraregional ACHD centres are very important, as some patients will require more advanced surgical and interventional expertise and resources. In Switzerland, this collaboration between regional and supraregional centres is well established. Furthermore, in the last few years, regional centres in Switzerland have played a pivotal role in delivering scientific publications aimed at improving evidence-based care for these patients in Switzerland [6–8].
Many complex adult congenital heart disease patients can and should be treated locally at regional ACHD centres, particularly in emergency situations. The lack of expertise in regional adult congenital heart disease would lead to a higher referral to supraregional ACHD centres, delayed adequate treatment and likely hamper the outcome [9]. Referral to specialised ACHD centres was shown to be associated with a significant mortality reduction [10]. Thus, we would like to emphasise the importance of care networks with close collaboration between regional and supraregional centres for optimal care by ACHD centres.
Regional ACHD centres may also provide consulting services for primary care physicians, taking care of adult congenital heart disease patients with low-to-moderate disease complexity and especially being equipped to treat and triage adult congenital heart disease patients with cardiac complications needing hospitalisations.
The study has the following limitations: First, patients from only three regional ACHD centres in Switzerland were included in the study. However, the remaining centres have similar structure and collaboration to those of the supraregional ACHD centres and data from these centres will very likely not be very different. Furthermore, there are differences in the prevalence of cardiac-related complications and cardiac-related interventions between the three analysed regional ACHD centres. These differences are caused by longer follow-up durations and a larger patient cohort from University Hospital Basel compared to St Gallen Cantonal Hospital and Lucerne Cantonal Hospital. Second, the study only describes the current situation in regional ACHD centres, and we did not analyse outcomes in supraregional centres. Third, it is very likely that local adult congenital heart disease patients, particularly the more complex ones, have their regular follow-up at supraregional ACHD centres. Therefore, a selection bias within our cohort is possible. Fourth, follow-up duration was calculated using a fixed administrative censoring date (31 March 2022), corresponding to the end of the follow-up data collection period. As data updates occurred over a three-month window (January to March 2022), this approach may not capture the precise follow-up duration for all patients. This limitation should be considered when interpreting follow-up estimates and event rates.
In Switzerland, regional ACHD centres play an important role in the management of a substantial proportion of adult congenital heart disease patients. Most hospitalisations occurring during follow-up were managed locally. This was particularly true for emergencies, arrhythmias, and heart failure hospitalisations. The main reasons for referral to supraregional ACHD centres were complex congenital heart surgery and complex percutaneous interventions.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
This study received no funding.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. – Ruperti Repilado: research grant from the Swiss National Science Foundation, outside of the submitted work. – Stämpfli: travel grants, speaker fees, consulting fees, or proctoring fees from Abbott Structural Heart, Alnylam, AstraZeneca, Bayer, Bristol-Myers Squibb, Edwards, Novo Nordisk, Polares Medical, Pfizer, and Takeda as well as research grants from Pfizer and GAMBIT Foundation, unrelated to this article. Advisory board role for Alnylam, AstraZeneca, Bayer, Bristol-Myers Squibb, Novo Nordisk and Pfizer, unrelated to this article. – No other potential conflict of interest related to the content of this manuscript was disclosed.
1. Sun HY. Prenatal diagnosis of congenital heart defects: echocardiography. Transl Pediatr. 2021 Aug;10(8):2210–24. doi: https://doi.org/10.21037/tp-20-164
2. Chan A, Aijaz A, Zaidi AN. Surgical outcomes in complex adult congenital heart disease: a brief review. J Thorac Dis. 2020 Mar;12(3):1224–34. doi: https://doi.org/10.21037/jtd.2019.12.136
3. Bouchardy Judith GM. Schwerzmann Markus, Attenhofer Jost Christine, De Pasquale Gabriella, Oxenius Angela, Rutz Tobias, Wustmann Kerstin, Balmer Christian, Tobler Daniel. Grown-up congenital heart disease: recommendations for standards of care. Cardiovasc Med. 2015;18(04):144–5.
4. Baumgartner H, De Backer J, Babu-Narayan SV, Budts W, Chessa M, Diller GP, et al.; ESC Scientific Document Group. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur Heart J. 2021 Feb;42(6):563–645. doi: https://doi.org/10.1093/eurheartj/ehaa554
5. Tobler D, Schwerzmann M, Bouchardy J, Engel R, Stambach D, Attenhofer Jost C, et al.; On Behalf Of Sacher. Swiss Adult Congenital HEart disease Registry (SACHER) - rationale, design and first results. Swiss Med Wkly. 2017 Oct;147(4344):w14519. doi: https://doi.org/10.4414/smw.2017.14519
6. Nussbaumer C, Schwerzmann M, Elchinova E, Goulouti E, Tobler D, Greutmann M, et al. Association of reduced peak left atrial strain with supraventricular arrhythmia in adults with congenital heart disease. Int J Cardiovasc Imaging. 2024 Oct;40(10):2133–44. doi: https://doi.org/10.1007/s10554-024-03205-9
7. Ruperti-Repilado FJ, Affolter J, Bouchardy J, Gabriel H, Stämpfli SF, Engel R, et al. Young adults after arterial switch operation for transposition of the great arteries in Switzerland: a growing population. Swiss Med Wkly. 2022 Feb;152(708):w30114. doi: https://doi.org/10.4414/SMW.2022.w30114
8. Ruperti-Repilado FJ, Tobler D, Greutmann M, Bouchardy J, Ladouceur M, Dos-Subira L, et al.; EPOCH. Risk stratification of adults with congenital heart disease during the COVID-19 pandemic: insights from a multinational survey among European experts. Open Heart. 2021 Apr;8(1):e001455. doi: https://doi.org/10.1136/openhrt-2020-001455
9. Ducas RA, Mao T, Beauchesne L, Silversides C, Dore A, Ganame J, et al. Adult Congenital Heart Disease Care in Canada: Has Quality of Care Improved in the Last Decade? Can J Cardiol. 2024 Jan;40(1):138–47.
10. Mylotte D, Pilote L, Ionescu-Ittu R, Abrahamowicz M, Khairy P, Therrien J, et al. Specialized adult congenital heart disease care: the impact of policy on mortality. Circulation. 2014 May;129(18):1804–12. doi: https://doi.org/10.1161/CIRCULATIONAHA.113.005817