Revision of a nationwide competency framework for undergraduate medical education
in Switzerland: PROFILES 2
DOI: https://doi.org/https://doi.org/10.57187/s.4389
Christoph Berendonka*,
Tuija Eeva Elisabeth Waldvogelb*,
Raphaël Bonvinc,
Christian Schirlod,
Jörg Goldhahnb,
Frank Zimmermanne,
Mathieu
Nendazf
a Institute for Medical Education,
University of Bern, Bern, Switzerland
b Department of Health Science and
Technologies, Swiss Federal Institute of Technology (ETH), Zurich, Switzerland
c Department of Community Health, University
of Fribourg, Fribourg, Switzerland
d Faculty of Health Sciences and Medicine,
University of Lucerne, Lucerne, Switzerland
e Faculty of Medicine at University of
Basel, University of Basel, Basel, Switzerland
f Department of Medicine, Faculty of
Medicine, University of Geneva, Geneva, Switzerland
* These authors contributed equally to this
manuscript
Summary
For more than 20 years, Switzerland has had
a national binding set of learning objectives to guide medical education at
universities. The learning expectations, compiled in the Principal Relevant Objectives and Framework for Integrative Learning
and Education in Switzerland (PROFILES), were revised in 2023. The purpose
of this article is to describe the revision process and highlight the changes
and updates in PROFILES 2. The new document consists of three interrelated and
interdependent chapters: the Competencies and Roles (CRs), the Entrustable
Professional Activities (EPAs) and the Situations as Starting Points
(SSPs). The CRs are based on the CanMEDS roles, which describe the personal
attributes and competencies of the graduate. EPAs define what activities the
graduate is expected to perform on the first day of residency. SSPs represent
situations in which the professional activities are expected to be performed. In
terms of content, three new areas of focus have been added: planetary health;
diversity, equity and inclusion (DEI); and digitalisation. The revised PROFILES
reflects current best practice in medical education and will help to ensure
that the needs of future generations of doctors and society are met.
Abbreviations
- EPAs
-
Entrustable Professional Activities
- PROFILES
-
Principal Relevant Objectives and Framework for Integrative Learning
and Education in Switzerland
- SCLO
-
Swiss Catalogue of Learning
Objectives for Undergraduate Medical Training
- SMIFK/CIMS
-
Joint Commission of the Swiss
Medical Schools
- SSP
-
Situations as Starting Points
Introduction
In 2000, the Joint Commission of the Swiss
Medical Schools (SMIFK/CIMS) decided to develop a national catalogue of
learning objectives in response to various changes in educational policy
(accreditation, bilateral negotiations between Switzerland and the EU). This
first Swiss Catalogue of Learning Objectives for Undergraduate Medical Training
(SCLO) was published two years later [1, 2].
The SCLO marked an important advance in medical education, because for the
first time the content and aims of medical training were widely discussed. Criticism
arose however, as the document was essentially a long list of “discipline-related
objectives” (a list of diagnoses and factual knowledge) and “problems
as starting points” (a symptom, sign or test result of a patient with which the
physician may be confronted). The SCLO did not adequately address social,
attitudinal and ethical issues [3].
This feedback was taken into account when
the catalogue was revised. In the second edition of the SCLO, published in 2008
[3], a specific chapter on General Objectives
based on the CanMEDS 2005 Framework [4] was
integrated into the document. The CanMEDS framework was originally developed by
the Royal College of Physicians and Surgeons of Canada with the goal to
“identify the core competencies generic to all specialists to meet the needs of
society” [5]. With the integration of
CanMEDS, the general objectives of the different roles of a physician became
tangible. This was a first step towards a reference document based on competences,
defined as a set of cognitive learning objectives, skills, attitudes and
values.
In light of developments in medicine and
medical education, the SMIFK/CIMS decided to undertake a complete revision of
the SCLO in the mid-2010s [6]. The
guiding principle in revising the document was to adopt the notion of competency-based
education and to promote an integrative approach to medicine. In 2017 the Principal
Relevant Objectives and Framework for Integrative Learning and Education in
Switzerland (PROFILES) document was published [6]. PROFILES provided a generic description of
outcome-based
competencies that cover the field of medicine without focusing on specific disciplines.
Consequently, the “discipline-related objectives” were dropped and
a chapter was added presenting a set of Entrustable Professional Activities
(EPAs) reflecting the main medical tasks that a physician must be able to
perform autonomously on the first day of residency [7]. PROFILES also provided an
important reference for the
development and orientation of existing curricula, and was especially relevant for
the newly created medical degree programmes (Universities of Fribourg, Lucerne
and St Gallen, and the Swiss Federal Institute of Technology Zurich [ETH]). At
ETH, the new bachelor’s degree in medicine was built from scratch by using
PROFILES for curriculum development by mapping PROFILES items to each new
module to guide the definition of its content [8,
9]. It also served as a reference for the Federal Licensing Examination that
every graduate must pass to begin postgraduate training. The content of the
federal examination in human medicine is determined by PROFILES. This national
examination is held simultaneously and identically in the respective
universities. The examination consists of two parts: a written examination with
240 multiple-choice questions and a practical clinical skills examination with
12 Objective Structured Clinical Examination (OSCE) stations. In this sense,
PROFILES supports the link between undergraduate and postgraduate medical education
in Switzerland.
Now that PROFILES has been in use for
several years, the SMIFK/CIMS has decided to review and update the document to
reflect social and global developments in medical education and to adapt its
three chapters to best support its ongoing widespread implementation. This
article describes the approach and methods used to review and revise PROFILES. It
aims to make the process as transparent as possible and to serve as a reference
for stakeholders that are planning to undertake a similar exercise.
Process
A working group, composed of experts from
multiple medical education fields: clinicians, deans, medical education
experts, faculty staff and student representatives, was mandated by the
SMIFK/CIMS in 2021 to carry out the review. Details on the WG members can be
found in the appendix in table S1. The review was structured in the following
phases: inquiry, analysis and validation.
Inquiry of needs
In November 2021, a targeted needs
assessment was initiated. The invitation to submit proposals for changes to
PROFILES was sent to the deaneries of all Swiss faculties of medicine, the
university hospitals, the Institute for Medical Education (Institut für Medizinische
Lehre, IML), the Association of Swiss Assistant and Senior
Physicians (Verband Schweizerischer Assistenz-
und Oberärztinnen und -ärzte VSAO), the Swiss Medical Students’ Association (SWIMSA),
the Joint Commission of the Swiss Medical Schools (SMIFK/CIMS), the Swiss Institute
for Postgraduate and Continuous Education (SIWF), the
Swiss Medical Association (Foederatio Medicorum Helveticorum, FMH), the Federal Office
of Public Health and the Swiss Armed Forces.
Analysis of needs
As a first step, each member of the working
group individually assessed each proposed change and decided whether to support
or reject the proposal. In a second step, iterative rounds of revision and
review took place in hybrid meetings of the entire working group. A nominal group
technique for reflection on the formal structure and content was used for these
meetings [10]. During this process,
literature was consulted to relate the proposed innovations to international
trends. After three meetings, consensus was reached and no further revisions
were requested by the group members.
Validation of goals and objectives
A two-strategy approach was adopted to
validate the proposed changes to the PROFILES document. Regular reports and
discussions were held at SMIFK/CIMS meetings on the ongoing revision process. SMIFK/CIMS
members already include deans and vice-deans from all faculties and training
centres, but in addition, feedback on the preliminary draft of PROFILES 2 was specifically
sought from the deaneries of all faculties of medicine in Switzerland. The
revised and updated document was well received, and no significant requests
were made to change or add to the document. Based
on this feedback and the discussions at the SMIFK/CIMS meetings, the document
was finalised and presented at a SMIFK/CIMS meeting in June 2023, where it was
unanimously adopted.
Outcomes
In total, 128 proposals were submitted by the
contacted stakeholders. Most of the proposals were submitted by the medical
faculties and the associated university hospitals (92%), followed by the
student association (6%) and other stakeholders (2%). The proposals fell into
three categories: implementation of main innovations; structural adaptations
affecting the understanding of the three PROFILES chapters and their
interrelation; and editorial adaptations concerning rewording or elimination of
duplicates of clinical issues in EPAs or SSPs.
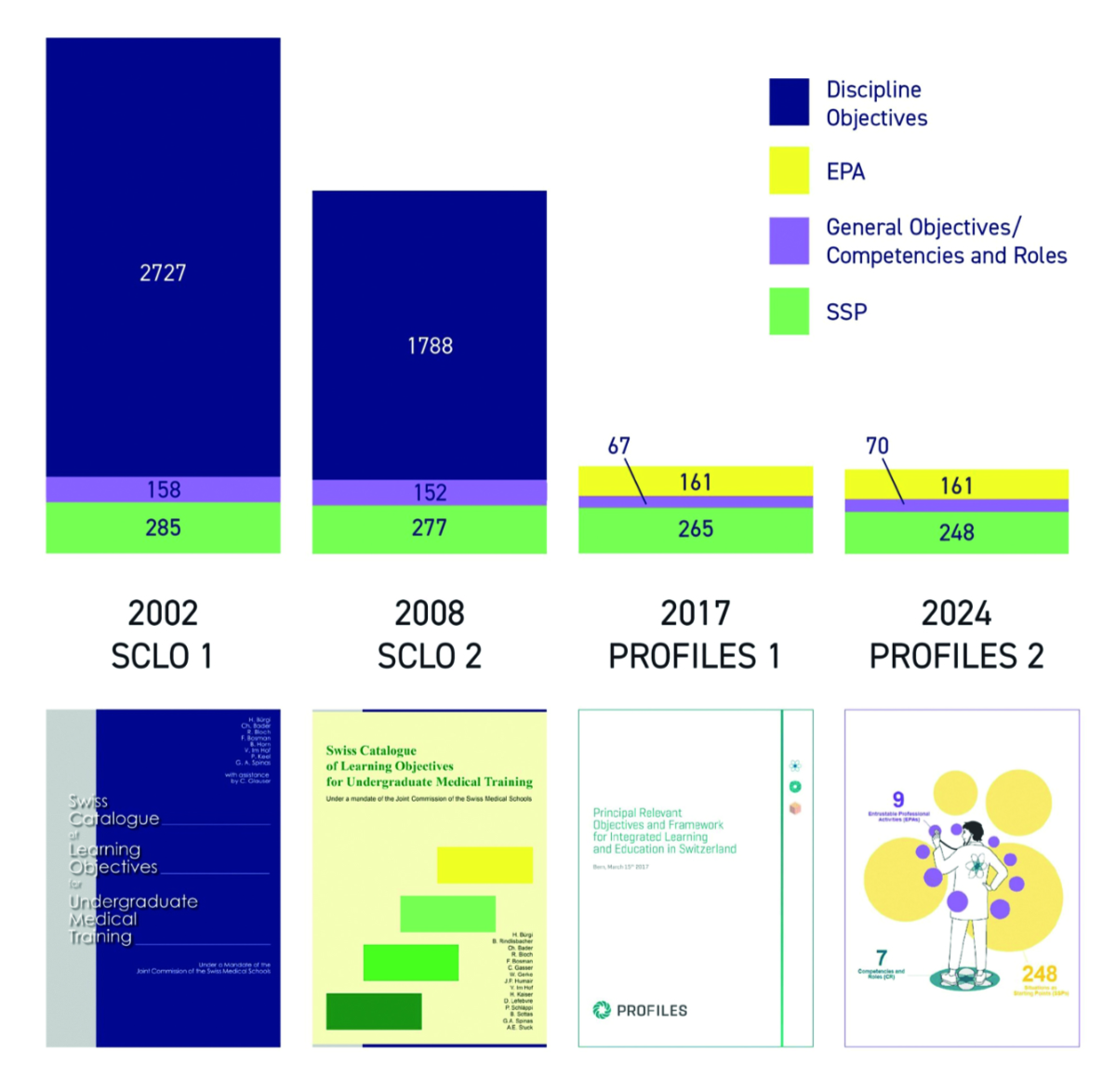
An overview of the evolution of the
national learning objectives catalogue in Switzerland from SCLO 1 to PROFILES 2
is presented in figure 1, which
delineates the number of items related to the corresponding chapter.
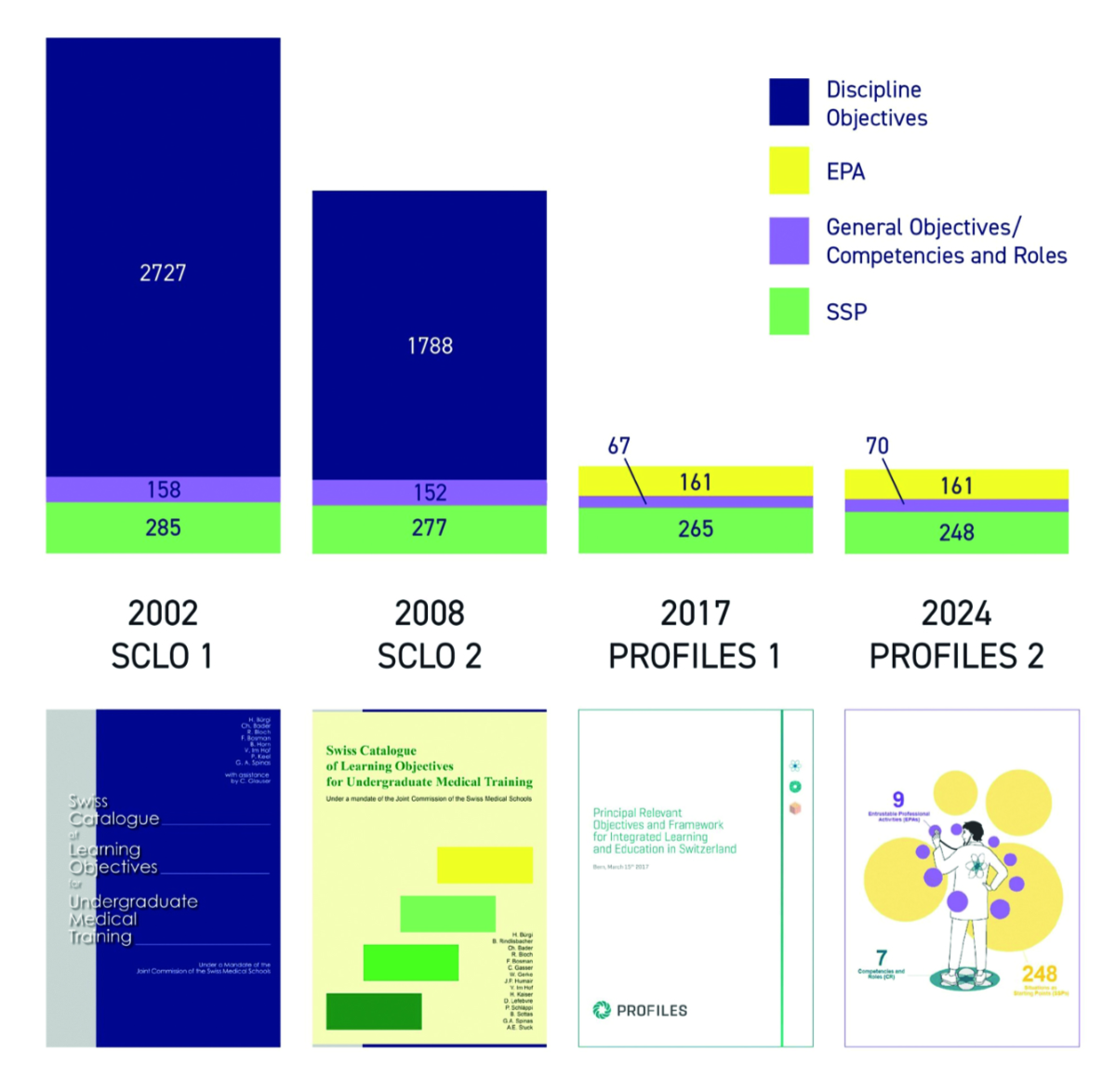
Figure 1Evolution of the learning expectations (in terms of number of items related to discipline-related
objectives, Entrustable Professional Activities [EPAs], General
Objectives/Competencies and Roles, and Situations as Starting Point [SSP] from
the first national catalogue SCLO 1 in 2002 to PROFILES 2 in 2024).
Main innovations
Approximately one third of proposals related
to content changes, focusing on three topics: planetary health; diversity,
equity and inclusion (DEI); and digitalisation.
The importance of these three themes is well supported by international
literature on medical education and is, in terms of content, the most
significant development of the PROFILES 2 document.
Planetary health
Based on the concept of planetary
boundaries [11], which was first defined
in 2009, and the comprehension that human health depends on the environmental
state, the concept of planetary health was defined [12]. The concept of planetary
health looks at the material,
biological, social and cultural aspects of public health and accepts that human
health and the state of the environment are irreversibly intertwined [13]. There is
overwhelming scientific evidence
on the adverse effects of environmental changes on human health. Examples are
numerous: heat waves increase the number of cardiovascular diseases [14], air pollution
leads to respiratory
diseases [15], while the loss of
biodiversity leads to increasing prevalences of allergies and chronic
inflammatory diseases [16, 17].
Additionally, the human health sector itself has an impact on the environment:
in OECD countries, China and India, the healthcare sector accounts for 5% of
the national carbon footprint of these countries [18]. The “AMEE Consensus Statement
2021 on planetary health and education for
sustainable healthcare” highlights the importance of preparing health professionals
to
address the upcoming challenges through medical education [19].
Diversity, equity and inclusion
The necessity of implementing diversity,
equity and inclusion in medical education arose in response to the increasing visibility
and awareness given to diversity in patients and students. Counteracting
discrimination and striving for equity is also documented in the Swiss Federal
Constitution (Art. 8) and Swiss Criminal Code (Art. 261) [25, 26]. By
implementing diversity, equity and inclusion in medical curricula, the quality
of healthcare (by inclusion of marginalised and vulnerable populations) can be
improved and the comfort and success of students from underrepresented groups
at faculties of medicine can be enhanced [20].
Most frequently, diversity, equity and inclusion is discussed in medical
education concerning the following dimensions: age, gender, ethnicity, physical
impairment, sexual orientation and religion [21].
The need for such standards is evident in the numerous publications concerning
insufficient healthcare for minorities such as transgender [22–25], for patients from
diverse cultural
backgrounds [26] or the inclusion of
students with disabilities into medical training [27]. An evaluation of sex- and gender-specific
medicine in German
curricula showed that the implementation of diversity, equity and inclusion in
medical curricula varies greatly between medical faculties [28]. To address this heterogeneity,
it is
recommended that aspects of the diversity, equity and inclusion should be
included in documents that guide undergraduate medical education [21].
Digitalisation
The importance of implementing digital
skills into medical education is evident when looking at the speed at which new
technologies are developed and introduced into clinical practice and the
healthcare system. Applications of digital technology in medicine are diverse,
ranging from AI-based cancer detection [39–41], to the use of AI in
computational psychiatry [43]. An overview of the digital competencies in
medical education in Switzerland from 2020 revealed that digital competencies
are very heterogeneously taught at the different faculties [29]. Traditionally, new
content is only
integrated into a medical curriculum when it becomes part of the generally
accepted body of knowledge [30, 31].
However, for digital competencies this procedure would be fatal as future
developments have to be anticipated in order to help shape the future of (digitalisation
in) medicine [30].
Elements of planetary health, diversity,
equity and inclusion and digitisation were mentioned in PROFILES 1, but the
revision has given them increased weight and visibility. Tables S2, S3 and S4 in the
appendix illustrate the evolution of items
from PROFILES 1 to PROFILES 2.
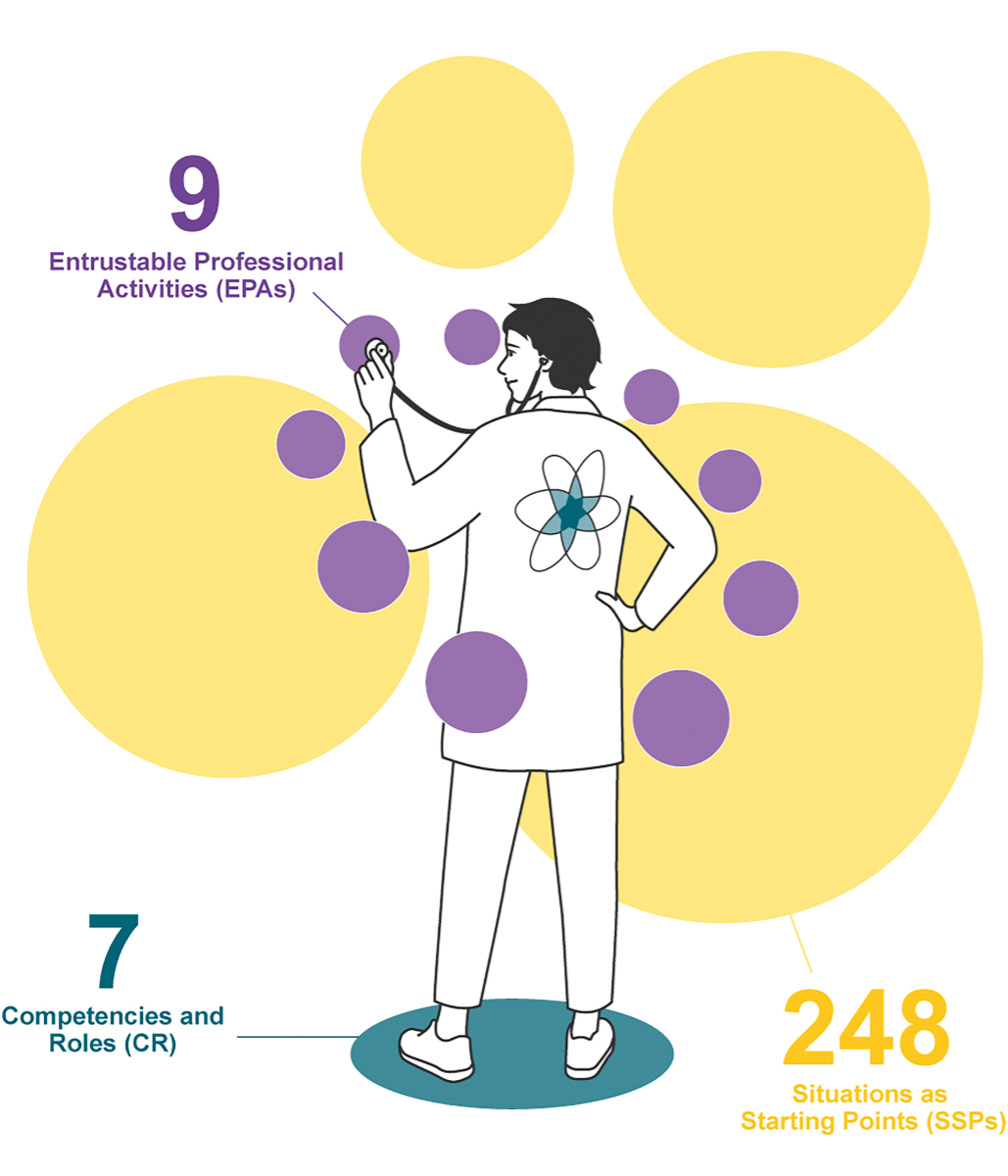
Structural adaptations
First, Competencies and Roles
replaced the term General Objectives to reflect the competency-based
approach. Second, based on the experience of implementing PROFILES 1 and the
feedback received, it has become clear that many users struggled with how to
distinguish and use the three PROFILES chapters. Thus, great care has been
taken to ensure that the reader of the new document realises that the three
main chapters of PROFILES cover three inseparable dimensions of medical
practice: Competencies and Roles (CR) represent the personal attributes
and competencies of the graduate, Entrustable Professional Activities
(EPAs) describe what the graduate is expected to perform (by using the
competencies), and Situations as Starting Points for Learning (SSPs) list
the situations in which these professional activities are expected to be
performed. An illustration has been made to highlight the complex relationship
between the three chapters (see figure 2).
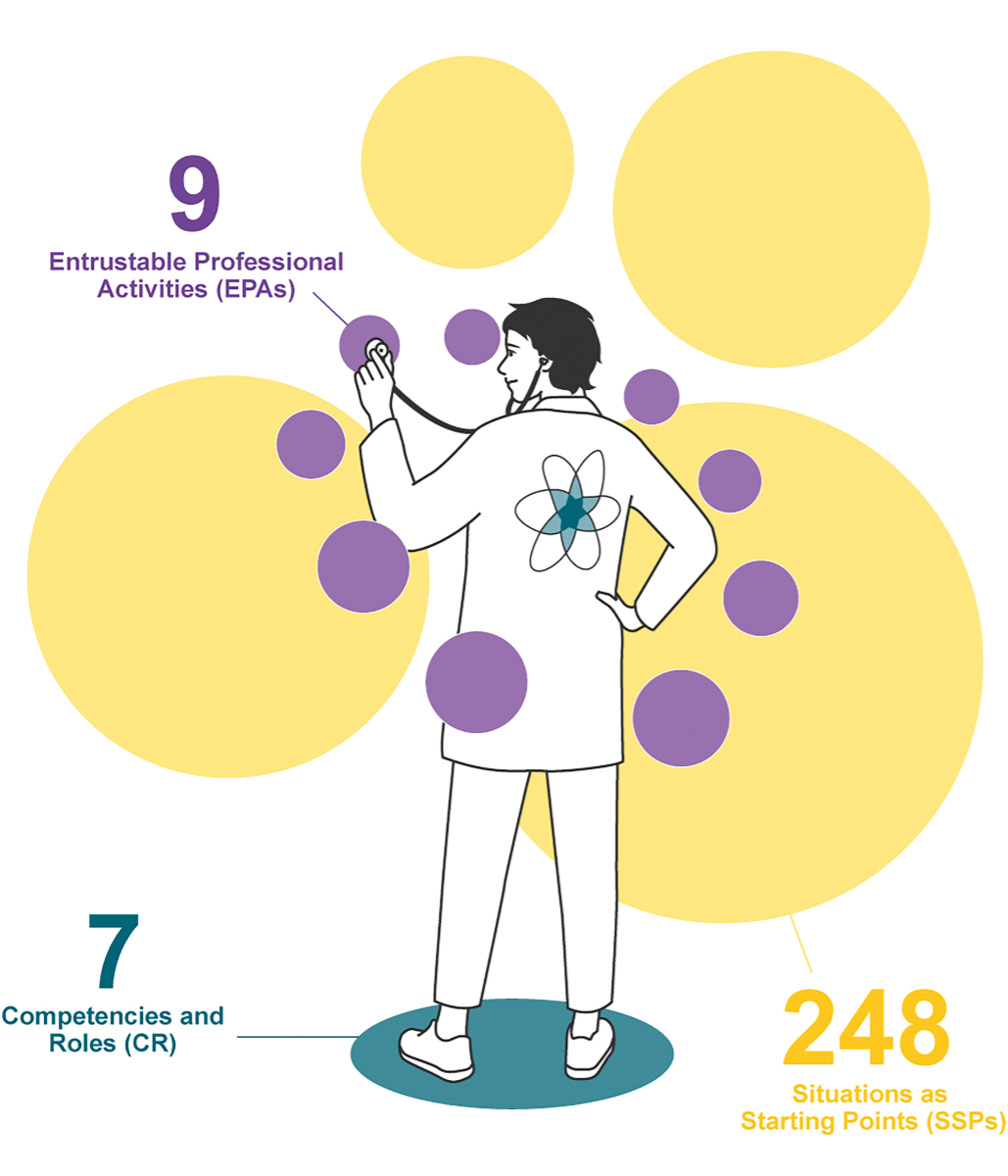
Figure 2Illustration showing the interplay
between the three chapters of the PROFILES document: Competencies and Roles
(CR), Entrustable Professional Activities (EPAs) and Situations as Starting Points
(SSPs).
Editorial adaptations
Around half of the proposals concerned the
specification of the detailed wording or the removal of duplicates in the EPA
and SSP chapters. In the SSP chapter, the number of items decreased from 265 to
248 (see figure 1). In this category, the
clinical expertise of the working group was of great importance to find the
right formulations while keeping the level of complexity in line with the
level of expertise the medical students should reach by the end of
their studies for the federal licensing exam.
Outlook
The basic structure of the PROFILES
document, with its competency-based approach to undergraduate medical
education, has not been adapted and thus proven its worth. In this sense, the
updated PROFILES 2 document does not represent a revolution, but rather an
evolution. Retaining the tripartite structure (SSP originating from SCLO 1, CanMEDS
roles from SCLO 2 and EPA from
PROFILES 1), the current version provides continuity with
the previous edition but integrates the global trends that will shape
healthcare in the future. PROFILES 2 comes into force for the 2025/26 semester
and the document will be the basis for the Federal Licensing Examination 2028.
The process of implementing PROFILES 2 by
translating the expectations into teaching and assessment in different medical
schools has only just begun. For successful implementation, it is particularly
important to align the competence-based outcome parameter described in PROFILES
2 with the curriculum design and the assessment system [32]. Equally important to
success is a well-qualified teaching
staff who place their teaching within a global vision of the concepts that
underpin PROFILES 2. If the full potential of competency-based education is to
be implemented, it is essential that the development of this approach in both
undergraduate and postgraduate medical education is coordinated and that there
is a seamless and coherent transition between the two stages of education [6, 33].
For future revisions, the needs assessment
might be supported by technical tools that facilitate reporting by all
stakeholders, as has already been done in Germany for the revision of the NKLM
catalogue (equivalent to PROFILES) [34, 35].
In the present revision, the involvement of patient representatives or other
civil representation was left at the faculties’ discretion, so this occurred
inhomogenously. In a forthcoming revision of this document, it seems even more
important to consider the systematic involvement of representatives of civil
society [36]. The CanMEDS project has
pioneered this approach by advocating a competence framework that takes into
account societal needs. Such an approach would be in line with the WHO’s call
to strengthen public accountability in health systems and policy setting [37].
Acknowledgments
We would like to thank the working group
and all the participating stakeholders for their contributions and feedback. Special
thanks go to John Griffin for his diligent editing of the manuscript.
Prof. Mathieu Nendaz
Faculty of
Medicine
Centre Médical Universitaire
Rue Michel Servet 1
CH-1211 Genève 4
Mathieu.Nendaz[at]unige.ch
References
1. Bürgi H, et al. Swiss Catalogue of Learning Objectives for Undergraduate Medical Training.
Joint Commission of the Swiss Medical Schools; 2002.
2. Bloch R, Bürgi H. The Swiss catalogue of learning objectives. Med Teach. 2002 Mar;24(2):144–50.
doi: https://doi.org/10.1080/01421590220120759
3. Bürgi H, et al. Swiss Catalogue of Learning Objectives for Undergraduate Medical Training.
Joint Commission of the Swiss Medical Schools; 2008.
4. Frank JR, Snell LS, Sherbino J. The CanMEDS 2015 Physician Competency Framework. 2015.
5. CanMEDS history. Available from: https://www.royalcollege.ca/en/canmeds/about-canmeds/history-canmeds.html
6. Michaud PA, Jucker-Kupper P; the Profiles Working Group. The “Profiles” document:
a modern revision of the objectives of undergraduate medical studies in Switzerland.
Swiss Med Wkly. 2016 Feb;146(0506):w14270. doi: https://doi.org/10.4414/smw.2016.14270
7. Ten Cate O, Schumacher DJ. Entrustable professional activities versus competencies
and skills: exploring why different concepts are often conflated. Adv Health Sci Educ
Theory Pract. 2022 May;27(2):491–9. doi: https://doi.org/10.1007/s10459-022-10098-7
8. Goldhahn J, Brack U, Ahlers O. Implementation of a new competency based learning objectives
catalogue into a new integrated medical curriculum – building from the scratch. Ottawa
Conference. Abu Dhabi, United Arab Emirates; 2018.
9. Goldhahn J, et al. Online Kartierung gegen die Schweizer „PROFILES“ – ein gemeinsames
Projekt der Eidgenössischen Technischen Hochschule Zürich (ETH) und des LOOOP-Projektes.
Gemeinsame Jahrestagung der Gesellschaft für Medizinische Ausbildung (GMA) und des
Arbeitskreises zur Weiterentwicklung der Lehre in der Zahnmedizin (AKWLZ). Münster:
German Medical Science GMS Publishing House; 2017.
10. Harvey N, Holmes CA. Nominal group technique: an effective method for obtaining group
consensus. Int J Nurs Pract. 2012 Apr;18(2):188–94. doi: https://doi.org/10.1111/j.1440-172X.2012.02017.x
11. Rockström J, Steffen W, Noone K, Persson A, Chapin FS 3rd, Lambin EF, et al. A safe
operating space for humanity. Nature. 2009 Sep;461(7263):472–5. doi: https://doi.org/10.1038/461472a
12. Myers SS. Planetary health: protecting human health on a rapidly changing planet.
Lancet. 2017 Dec;390(10114):2860–8. doi: https://doi.org/10.1016/S0140-6736(17)32846-5
13. Whitmee S, Haines A, Beyrer C, Boltz F, Capon AG, de Souza Dias BF, et al. Safeguarding
human health in the Anthropocene epoch: report of The Rockefeller Foundation-Lancet
Commission on planetary health. Lancet. 2015 Nov;386(10007):1973–2028. doi: https://doi.org/10.1016/S0140-6736(15)60901-1
14. Ragettli MS, Vicedo-Cabrera AM, Flückiger B, Röösli M. Impact of the warm summer 2015
on emergency hospital admissions in Switzerland. Environ Health. 2019 Aug;18(1):66.
doi: https://doi.org/10.1186/s12940-019-0507-1
15. Perera FP. Multiple Threats to Child Health from Fossil Fuel Combustion: Impacts of
Air Pollution and Climate Change. Environ Health Perspect. 2017 Feb;125(2):141–8.
doi: https://doi.org/10.1289/EHP299
16. Sandifer PA, Sutton-Grier AE, Ward BP. Exploring connections among nature, biodiversity,
ecosystem services, and human health and well-being: opportunities to enhance health
and biodiversity conservation. Ecosyst Serv. 2015;12:1–15. doi: https://doi.org/10.1016/j.ecoser.2014.12.007
17. Schmeller DS, Courchamp F, Killeen G. Biodiversity loss, emerging pathogens and human
health risks. Biodivers Conserv. 2020;29(11-12):3095–102. doi: https://doi.org/10.1007/s10531-020-02021-6
18. Pichler PP, Jaccard IS, Weisz U, Weisz H. International comparison of health care
carbon footprints. Environ Res Lett. 2019;14(6):064004. 10.1088/1748-9326/ab19e1
19. Shaw E, Walpole S, McLean M, Alvarez-Nieto C, Barna S, Bazin K, et al. AMEE Consensus
Statement: planetary health and education for sustainable healthcare. Med Teach. 2021 Mar;43(3):272–86.
doi: https://doi.org/10.1080/0142159X.2020.1860207
20. LeBlanc C, Sonnenberg LK, King S, Busari J. Medical education leadership: from diversity
to inclusivity. GMS J Med Educ. 2020 Mar;37(2):Doc18.
21. Ludwig S, Gruber C, Ehlers JP, Ramspott S; Diversity in Medical Education. Diversity
in Medical Education. GMS J Med Educ. 2020 Mar;37(2):Doc27.
22. Streed CG Jr, Navarra M, Klein J. Advancing undergraduate medical education regarding
the care of transgender and gender Diverse persons and communities. Perspect Med Educ.
2022 Dec;11(6):306–8. doi: https://doi.org/10.1007/s40037-022-00732-w
23. Safer JD, Coleman E, Feldman J, Garofalo R, Hembree W, Radix A, et al. Barriers to
healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016 Apr;23(2):168–71.
doi: https://doi.org/10.1097/MED.0000000000000227
24. Reisner SL, Vetters R, Leclerc M, Zaslow S, Wolfrum S, Shumer D, et al. Mental health
of transgender youth in care at an adolescent urban community health center: a matched
retrospective cohort study. J Adolesc Health. 2015 Mar;56(3):274–9. doi: https://doi.org/10.1016/j.jadohealth.2014.10.264
25. Safer JD, Pearce EN. A simple curriculum content change increased medical student
comfort with transgender medicine. Endocr Pract. 2013;19(4):633–7. doi: https://doi.org/10.4158/EP13014.OR
26. Petrov L. Weiterentwicklung der Wirtschaftslichkeitskontrolle nach KVG. Zürcher Studien
zum öffentlichen Recht. Volume 296. Zürich, Genf: Schulthess Verlag; 2024.
27. Fitzpatrick S, Barrett D. Disability inclusion in Medical Education: towards a quality
improvement approach. Med Educ. 2023 Jan;57(1):17–20. doi: https://doi.org/10.1111/medu.14952
28. Ludwig S, et al. Geschlechtsspezifische Medizin in der Lehre: noch in den Kinderschuhen.
Dtsch Arztebl. 2016;113:A-2364.
29. Hautz SC, Hoffmann M, Exadaktylos AK, Hautz WE, Sauter TC. Digital competencies in
medical education in Switzerland: an overview of the current situation. GMS J Med
Educ. 2020 Nov;37(6):Doc62.
30. Buhmann J, Felix J, Gächter T, Kowatsch T, Lehmann R, von Lutterotti N, et al. Digitalisierung
der Medizin: Konsequenzen für die Ausbildung. Schweiz Arzteztg. 2018;99(42):1441–4.
Available from: https://www.alexandria.unisg.ch/server/api/core/bitstreams/3c0b5958-d15b-416e-88c9-dfc9ada11a27/content
31. Rampton V, Mittelman M, Goldhahn J. Implications of artificial intelligence for medical
education. Lancet Digit Health. 2020 Mar;2(3):e111–2. doi: https://doi.org/10.1016/S2589-7500(20)30023-6
32. Sohrmann M, Berendonk C, Nendaz M, Bonvin R; Swiss Working Group For Profiles Implementation.
Nationwide introduction of a new competency framework for undergraduate medical curricula:
a collaborative approach. Swiss Med Wkly. 2020 Apr;150(1516):w20201. doi: https://doi.org/10.57187/smw.2020.20201
33. Maeder MB, et al. Kompetenzbasierte ärztliche Weiterbildung in der Schweiz unter besonderer
Berücksichtigung von EPAs. Ein Konzeptpapier des SIWF; 2021.
34. LOOOP – das nicht-kommerzielle Forschungsnetzwerk für Curriculumsentwicklung und Curriculum-Mapping.
2024 [cited 11.03.2025]. Available from: https://looop.charite.de/
35. Fakultätentag M. Nationaler Kompetenzbasierter Lernzielkatalog Medizin (NKLM) Version
2.0. 2024 [cited 18.04.2024]. Available from: https://nklm.de/zend/menu
36. Frank J. A history of CanMEDS - chapter from Royal College of Physicians of Canada
75th Anniversary history. 2004.
37. World Health Organisation. Strategic alliances: the role of civil society in health.
Geneva: World Health Organization; 2001. Available from: https://iris.who.int/bitstream/handle/10665/279937/CSI-2001-DP1-eng.pdf?sequence=1
Appendix
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.4389.