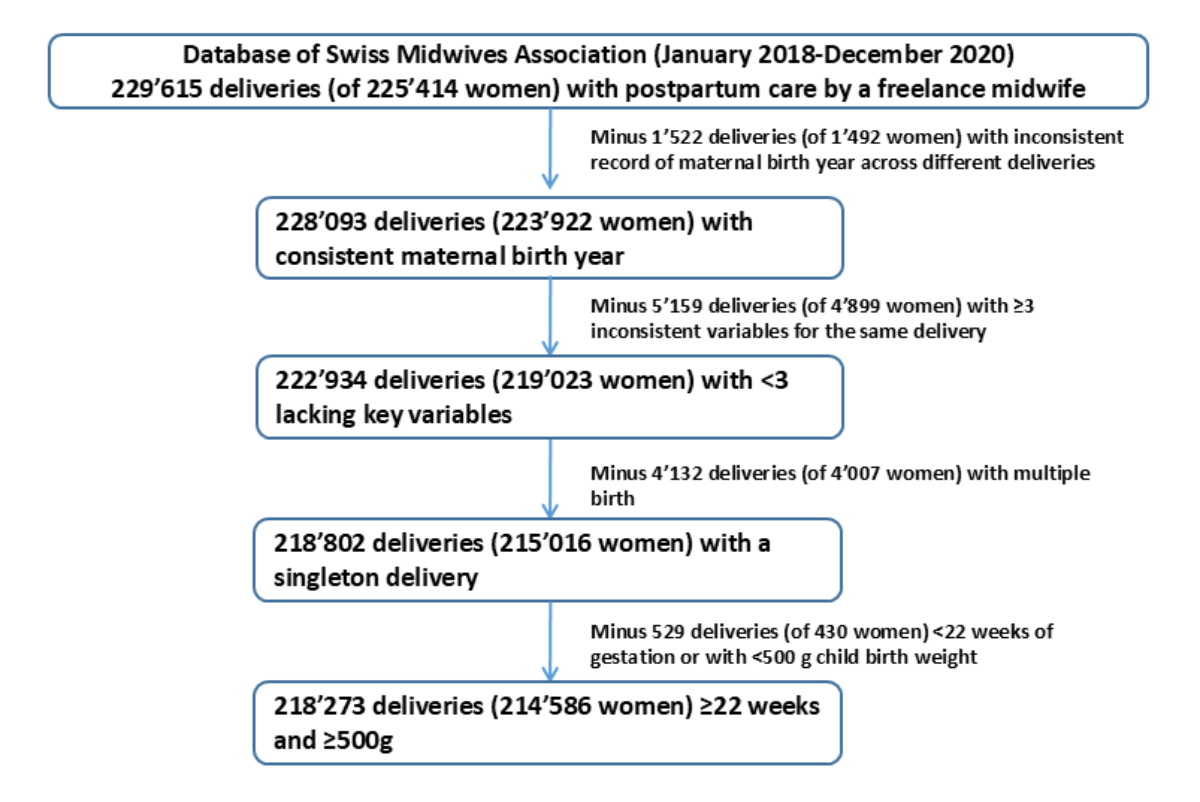
Figure 1Flowchart of the study population.
DOI: https://doi.org/https://doi.org/10.57187/s.4319
Proportions of preterm birth and other perinatal outcomes during coronavirus disease of 2019 (COVID-19)-related restrictions (referred to as lockdowns) varied widely across countries. A nationwide Danish study reported 90% fewer extremely preterm births (gestational week [GW] ≤28) during the local lockdown between 12 March and 14 April 2020, when compared to the average proportion of extremely preterm births during the same time period in the previous five years [1]. Consequently, an abundance of methodologically heterogeneous studies from different countries reported anything from a strongly reduced [2–7] to an unchanged [8–10] up to an increased risk of preterm births [11]. In January 2023, the large International Perinatal Outcomes in the Pandemic (iPOP) study, which collected harmonised data from 26 countries (52 million births) between 2015 and 2020, was published [12]. Primary analyses included standardised population-based data from 18 countries and yielded a statistically significant 3–4% decrease in preterm births during the first three months of lockdown in high- and middle-income countries. However, this result was not confirmed in a subset of 486,357 included births from Switzerland (BEVNAT) [12] nor in an observational study using data from the birth registry of the Swiss Federal Statistical Office (FSO) as well as from the Swiss Neonatal Network and Follow-Up Group (SwissNeoNet) [13]. Potential mechanisms behind observed changes in the proportion of preterm births during COVID-19-related lockdowns are a reduction in infections, air pollution, or physical stress. However, a reduction in preterm births might signal a reduction in the quality of obstetric care of high-risk women [12].
Other perinatal endpoints, such as Caesarean (C)-sections or neonatal Apgar scores, have not been investigated in Switzerland. A single-centre observational study at the maternity ward of a large hospital in Zurich, Switzerland, reported a decrease in the proportion of C-sections from 38% to 30% (similarly for planned and unplanned C-sections) during the first wave of the COVID-19 pandemic (1 March to 31 May 2020) when compared to the same time period in the two previous years [14]. However, studies based on single centres are prone to channelling bias. Studies evaluating the association between lockdowns in Switzerland and neonatal Apgar scores have not been conducted to date. Moreover, potential regional differences in birth outcomes during lockdowns have not been investigated, although different regions in Switzerland were differently affected during the first wave of COVID-19. We aimed to investigate the association between the first COVID-19-related lockdown in Switzerland (16 March to 10 May 2020, appendix table S1 [15–17]) and the proportion of different maternal and neonatal birth outcomes (preterm births, C-sections and Apgar scores <7 at 5 minutes) overall and within different regions of Switzerland using the nationwide statistics of outpatient midwifery services in Switzerland.
We conducted an observational study using anonymised data from the statistics of outpatient midwifery services in Switzerland. This data source was established in 2005 and has since been continuously developed. The statistics of outpatient midwifery services in Switzerland include information on all outpatient visits by a midwife in association with pregnancy, birth, and postpartum care of women in Switzerland [18]. The quality and completeness of the records has improved markedly since 2018, when it became mandatory for midwives to bill their provided services electronically. Data entered in the billing system are directly fed into the database, and there are several quality control measures in place during data entry (standardised variable format, feedback questions if values are outside the reference range) and processing (quality control checks and correction or deletion of implausible values). In 2020, 85,914 live births were registered in Switzerland and 83,715 women (>93%) were cared for by midwives during outpatient postpartum care. Mandatory health insurance covers between 10 and 16 outpatient postpartum visits by a midwife [18–21].
The statistics of outpatient midwifery services in Switzerland encompass anonymised information on demographics of the women, pregnancy- and birth-related records (gravidity, parity, multiple birth status, birth mode, birth place [hospital, birth centre, home]), child-related records (birth date, gestational week at birth, birthweight, Apgar scores), as well as number of visits, date of visit, type of visit (related to pregnancy, birth, or postpartum), frequently occurring healthcare problems during the postpartum period (e.g. breastfeeding problems, depression, exhaustion of the mother, hyperbilirubinaemia of the newborn), and indications for (possible) hospital (re)admission of mother or child.
We included all births between 2018 and 2020 to women with at least one postpartum-related outpatient visit by a midwife. We excluded births of women whose birth year was inconsistently recorded or if ≥3 key variables (i.e. birth mode, birth year of the mother, gravidity, parity, multiple birth status, gestational age at birth, birthweight of the child, birth place, or all three Apgar scores i.e. at 1, 5 and 10 minutes]) were lacking. We also excluded multiple births and miscarriages (births at gestational week <22 or birthweight <500 g). Midwives in Switzerland can choose between six different electronic billing systems; one of these does not reliably capture Apgar scores so we excluded all births billed via this system for analyses of Apgar scores (n = 15,631).
We evaluated three outcomes of interest: (1) Preterm birth: defined as a birth occurring <37 weeks of gestation and further subdivided into extremely preterm birth (<28 weeks of gestation), very preterm birth (28–31 weeks of gestation) or moderate/late preterm birth (32–36 weeks of gestation). The terms birth and post-term birth were defined, respectively, as births at 37–41 and ≥42 weeks of gestation [22]. We also stratified preterm births into births via C-section and vaginal births. (2) C-section birth: overall and stratified into planned vs unplanned C-section, or unknown. (3) Moderately reduced or low Apgar score at 5 minutes: defined as an Apgar score <7. In an additional analysis, we further evaluated Apgar scores <7 at 10 minutes as well as low Apgar scores (<5) at 5 and 10 minutes separately. Apgar scores were introduced in the 1950s as a standardised way to evaluate infants shortly after birth. The score ranges from 0 to 10 and evaluates the newborn on five criteria each scored from 0 to 2: appearance (skin colour), pulse, grimace (reflexes / response to stimulus), activity (muscle tone) and respiration. In Switzerland, tests are given to the newborn at 1, 5, and 10 minutes after birth. Generally, Apgar scores 7–10 are considered normal, with scores <5 indicating that a newborn requires resuscitation. However, the ability of Apgar scores to predict clinical outcomes is limited and in clinical practice decisions about resuscitation are made before any Apgar test is given [23].
We applied standard descriptive methods to document demographics and characteristics of the study population, stratified by year of birth, and compared these to the corresponding statistics of the Swiss Federal Office of Statistics. We also plotted proportions of all outcomes of interest per calendar week over time, separately for the years 2018, 2019, and 2020.
We conducted a logistic regression analysis to quantify changes in the proportion of outcomes (complete case analyses) in association with the lockdown in Switzerland [24]. For this, we included data between the start of January 2018 and the end of the lockdown period in 2020. The lockdown period was defined as the 8-week period between 16 March and 10 May 2020 (table S1 displays restrictions in Switzerland). The logistic regression models included an indicator variable for the time of the lockdown along with calendar day as a numerical trend variable, birth month and residential region of the mother (German-, French-, or Italian-speaking part of Switzerland, or unknown/international) as categorical variables.
To adjust for potential clustering due to mothers with more than one delivery in the observation period, the maternal identifier was treated as a cluster variable and robust variance estimates were used. Estimated effects of the lockdown are reported as odds ratios (ORs) with 95% confidence intervals (CIs). To address the uncertainty of a potential lag between the implementation of the lockdown and the studied outcomes, and the fact that the strict lockdown in Switzerland lasted only eight weeks (table S1 [16]), we ran two additional models extending and shortening the lockdown period to 6 and 10 weeks from 16 March 2020 for the three primary endpoints. We conducted sensitivity analyses by region of residence of the mother, i.e. Italian-speaking (Ticino), French-speaking, or German-speaking part of Switzerland. Because the German-speaking part of Switzerland is the largest part of the country, we also subdivided it into subregions (Northwest, Central, and Eastern Switzerland, as well as the cantons of Zurich and Bern). We further evaluated individual cantons with large university hospitals wherever sample size allowed; this was the case for Zurich, Bern, Geneva and Vaud (the latter two were also the cantons which, besides Ticino, were most heavily affected by the first COVID-19 wave in spring 2020). The cantons of Basel City and Lucerne have university hospitals but the sample size was too small for individual analysis [25]. We also conducted a sensitivity analysis only including women with a recorded inpatient birth. We further conducted two sensitivity analyses for the outcome “moderate/low Apgar score at 5 minutes”, in which we excluded (1) all births <37 weeks of gestation because preterm birth and moderate/low Apgar score are likely collinear and (2) all births in 2018, as Apgar scores were recorded less reliably in these two subsamples. All analyses were conducted using SAS statistical software (version 9.4; SAS Institute, Cary, NC, USA).
Our final study population included 218,273 singleton births to 214,586 women between 2018 and 2020 (flowchart in figure 1).
Figure 1Flowchart of the study population.
The largest proportion of women were aged 31–35 years when they gave birth (39.9%), and half of all births were a first-time birth (49.6%). Of all singleton newborns with recorded information on gestational age at birth (92.8%), 5.3% were born preterm (4.5% moderate/late preterm). In total, 30.2% of infants were born via C-section. Between 2018 and 2020, slightly more infants were born in the summer and autumn (51.5% between June and November) than in winter and spring (48.5%, table 1).
Table 1Characteristics of women who received postpartum care by a midwife in Switzerland (2018–2020).
| 2018 | 2019 | 2020 | Total | ||
| Number of births | 75,909 | 70,770 | 71,594 | 218,273 | |
| Number of women | 75,738 | 70,583 | 71,422 | 214,586* | |
| Maternal age at birth, n (%) | ≤20 years | 562 (0.7) | 449 (0.6) | 411 (0.6) | 1422 (0.7) |
| 21–25 years | 5355 (7.1) | 4890 (6.9) | 4676 (6.5) | 14,921 (6.8) | |
| 26–30 years | 19,573 (25.8) | 18,069 (25.5) | 18,629 (26.0) | 56,271 (25.8) | |
| 31–35 years | 29,711 (39.1) | 28,335 (40.0) | 28,884 (40.3) | 86,930 (39.8) | |
| 36–40 years | 16,774 (22.1) | 15,739 (22.2) | 15,882 (22.2) | 48,395 (22.2) | |
| 41–45 years | 3220 (4.2) | 2948 (4.2) | 2872 (4.0) | 9040 (4.1) | |
| ≥46 years | 249 (0.3) | 251 (0.4) | 228 (0.3) | 728 (0.3) | |
| Unknown | 465 (0.6) | 89 (0.1) | 12 (0.0) | 566 (0.3) | |
| Gestational age at birth, n (%) | Extremely preterm (<28 weeks) | 198 (0.3) | 212 (0.4) | 217 (0.3) | 627 (0.3) |
| Very preterm (28–31 weeks) | 303 (0.4) | 251 (0.4) | 265 (0.4) | 819 (0.4) | |
| Moderate/late preterm (32–36 weeks) | 3611 (4.8) | 2807 (4.0) | 2788 (3.9) | 9206 (4.2) | |
| Term (37–41 weeks) | 70,445 (92.8) | 58,840 (83.1) | 61,245 (85.5) | 190,530 (87.3) | |
| Post-term (≥42 weeks) | 477 (0.6) | 424 (0.6) | 440 (0.6) | 1341 (0.6) | |
| Unknown** | 875 (1.1) | 8236 (11.6) | 6639 (9.3) | 15,750 (7.2) | |
| Apgar score at 5 minutes***, median (IQR) | 9 (9–10) | 9 (9–10) | 9 (9–10) | 9 (9–10) | |
| Apgar score at 5 minutes***, n (%) | Apgar <7 | 1319 (1.8) | 1142 (1.8) | 1426 (2.2) | 3887 (1.9) |
| Apgar ≥7 | 60,251 (80.3) | 57,326 (91.6) | 58,926 (90.7) | 176,503 (87.1) | |
| Missing | 13,513 (18.0) | 4095 (6.6) | 4644 (7.2) | 22,252(11.0) | |
| Birth mode, n (%) | Vaginal | 52,367 (69.0) | 48,826 (69.0) | 48,964 (68.4) | 150,157 (68.8) |
| Caesarean section planned | 11,729 (15.5) | 11,021 (15.6) | 11,325 (15.8) | 34,075 (15.6) | |
| Caesarean section unplanned | 10,928 (14.4) | 9889 (14.0) | 10,098 (14.1) | 30,915 (14.2) | |
| Unknown | 885 (1.2) | 1034 (1.5) | 1207 (1.7) | 3126 (1.4) | |
| Parity, n (%) | 1 | 38,005 (50.1) | 34,986 (49.4) | 35,238 (49.2) | 108,229 (49.6) |
| ≥2 | 37,683 (49.6) | 35,701 (50.5) | 36,280 (50.7) | 109,664 (50.2) | |
| Unknown | 221 (0.3) | 83 (0.1) | 76 (0.1) | 380 (0.2) | |
| Place of birth#, n (%) | Hospital | – | 58,544 (82.7) | 61,743 (86.2) | 120,287 (84.5) (84.5) |
| Home | – | 792 (1.1) | 947 (1.3) | 1739 (1.2) | |
| Birth house | – | 1861 (2.6) | 1788 (2.5) | 3649 (2.6) | |
| Other | – | 367 (0.5) | 408 (0.6) | 775 (0.5) | |
| Missing | – | 9206 (13.0) | 6708 (9.4) | 15,914 (11.2) | |
| Place of birth during lockdown##, n (%) | Hospital | – | 6704 (84.3) | 6877 (85.5) | 13,581 (84.9) |
| Home | – | 89 (1.1) | 140 (1.7) | 229 (1.4) | |
| Birth house | – | 208 (2.6) | 222 (2.8) | 430 (2.7) | |
| Other | – | 36 (0.5) | 48 (0.6) | 84 (0.5) | |
| Missing | – | 915 (11.5) | 756 (9.4) | 1671 (10.5) | |
| Season at birth, n (%) | Winter (Dec/Jan/Feb) | 19,253 (25.4) | 16,881 (23.9) | 16,451 (23.0) | 52,585 (24.1) |
| Spring (Mar/Apr/May) | 17,052 (22.5) | 17,879 (25.3) | 18,299 (25.6) | 53,230 (24.4) | |
| Summer (Jun/Jul/Aug) | 19,212 (25.3) | 18,742 (26.5) | 19,047 (26.6) | 57,001 (26.1) | |
| Autumn (Sept/Oct/Nov) | 20,392 (26.9) | 17,268 (24.4) | 17,797 (24.9) | 55,457 (25.4) | |
* Some women gave birth multiple times during the 3-year study period, which is why the total number of individual women does not equal the sum of individual women of the three individual calendar years.
** Changes in the proportion of missing values between calendar years are due to changes in the billing software. The main provider made gestational age a non-compulsory variable after 2018.
*** 15,631 births excluded because they were billed via a billing system that does not reliably record Apgar scores.
# Place of birth was not well captured in 2018.
## Between 17 March 2019/2020 and 26 April 2019/2020.
Our study population was comparable to data of the Swiss Federal Statistical Office regarding the average age of women giving birth and the percentage of preterm births in different subgroups (appendix table S2). The percentage of neonates who were born prematurely between 2018 and 2020 was lower in the statistics of outpatient midwifery services in Switzerland than in the data of the Swiss Federal Statistical Office, which is likely explained by the fact that our study population excluded multiple births, whereas multiples were included in the Federal Statistical Office dataset.
Results of the logistic regression analyses are shown in figures 2A–2D and in appendix table S3. The lockdown in Switzerland was associated with a slight but not statistically significant increase in the proportion of preterm births during the 8-week lockdown period in Switzerland (OR: 1.09, 95% CI: 0.96–1.23), which became larger and statistically significant when the lockdown period was extended to 10 weeks (OR: 1.12, 95% CI: 1.01–1.25). After stratification by region, we observed a statistically significantly increased OR for preterm birth of 2.05 (95% CI: 1.10–3.85) during the lockdown period in the canton of Ticino, but not in any other region/canton of Switzerland (figure 2B, table S3). Figures 3–5 and appendix figure S1 graphically display the weekly proportion of the primary endpoints over time in 2018, 2019, and 2020.
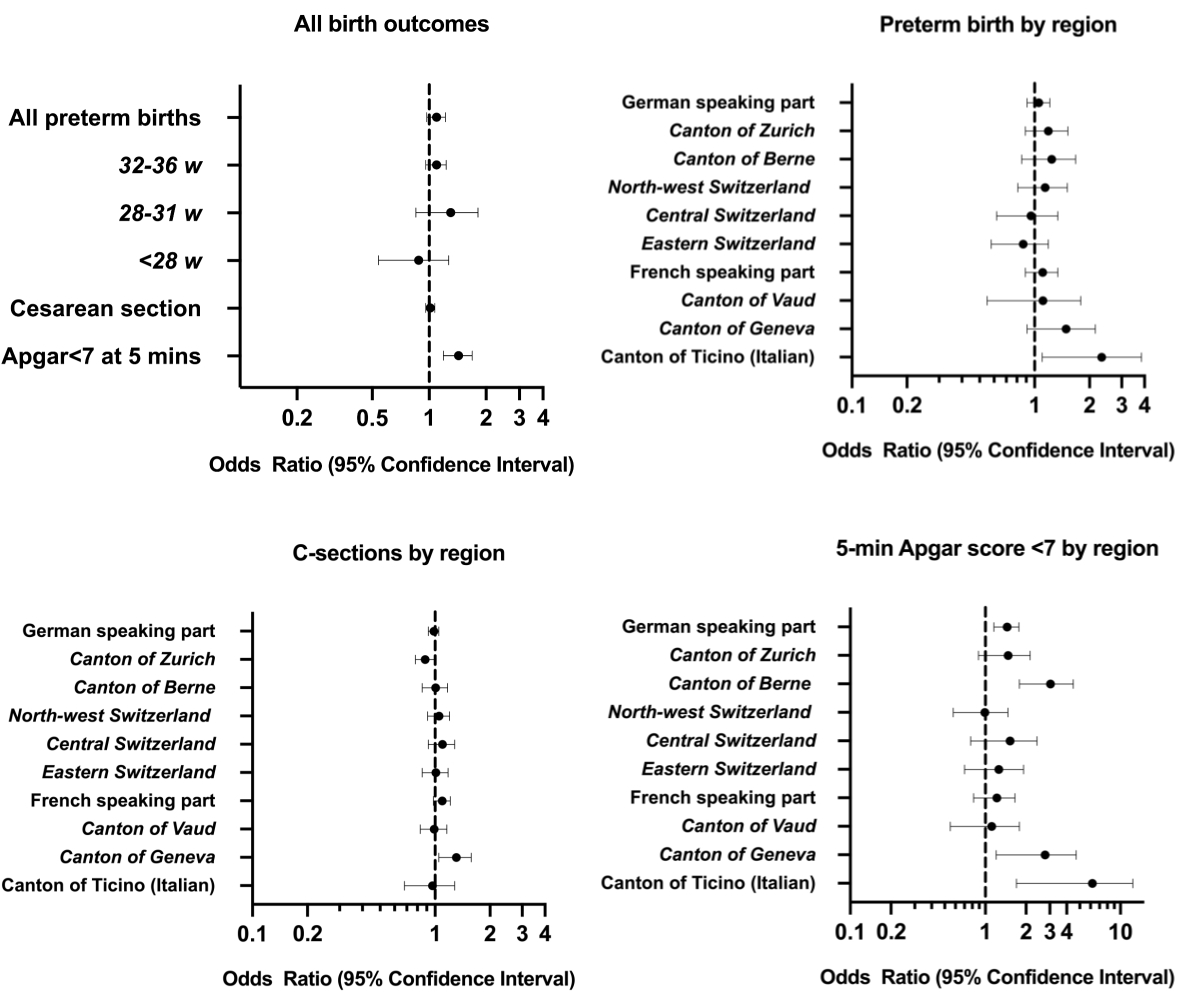
Figure 2(A) Odds ratios for the risk of adverse birth outcomes during the first COVID-19-related lockdown in 2020 in Switzerland. (B) Odds ratios for the risk of preterm birth during the first COVID-19-related lockdown in 2020 stratified by region. (C) Odds ratios for the risk of a Caesarean section (C-section) during the first COVID-19-related lockdown in 2020 stratified by region. (D) Odds ratios for the risk of an Apgar score <7 at 5 minutes of age during the first COVID-19-related lockdown in 2020 stratified by region.
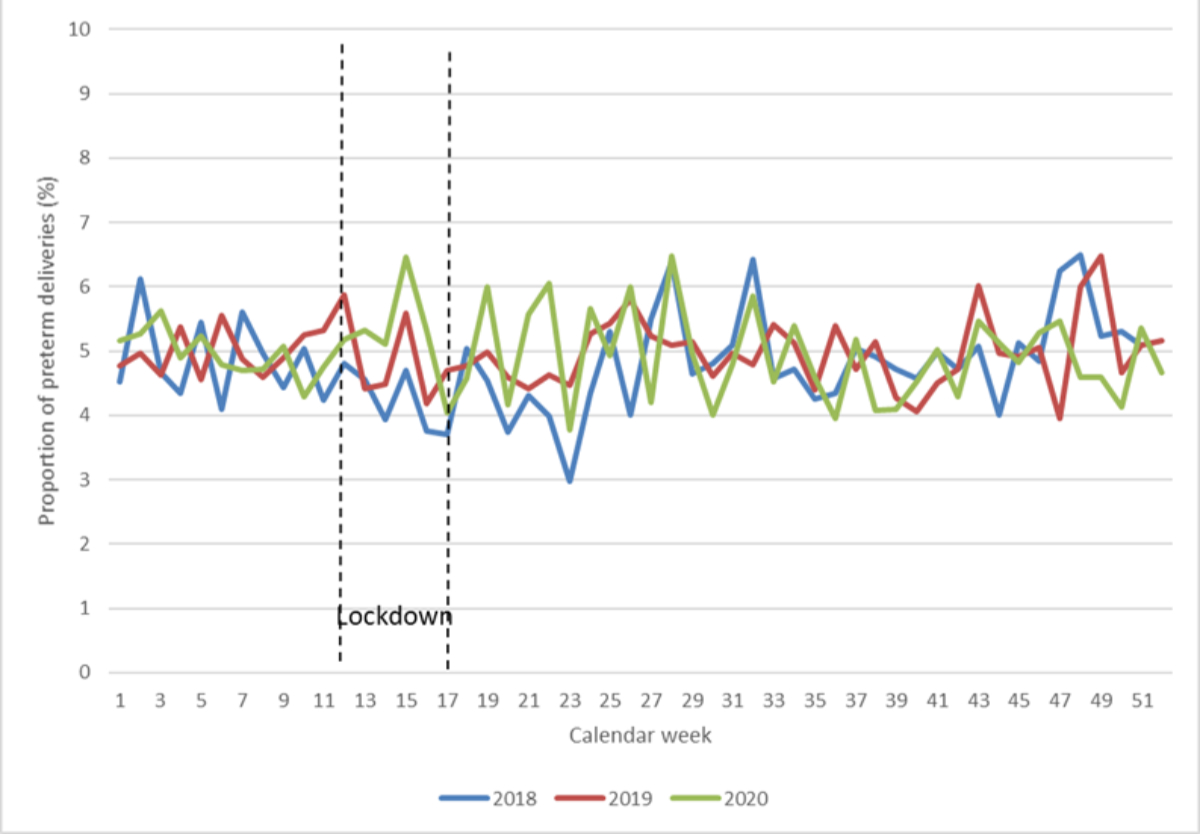
Figure 3Weekly proportion of preterm births between 2018 and 2020 in Switzerland.
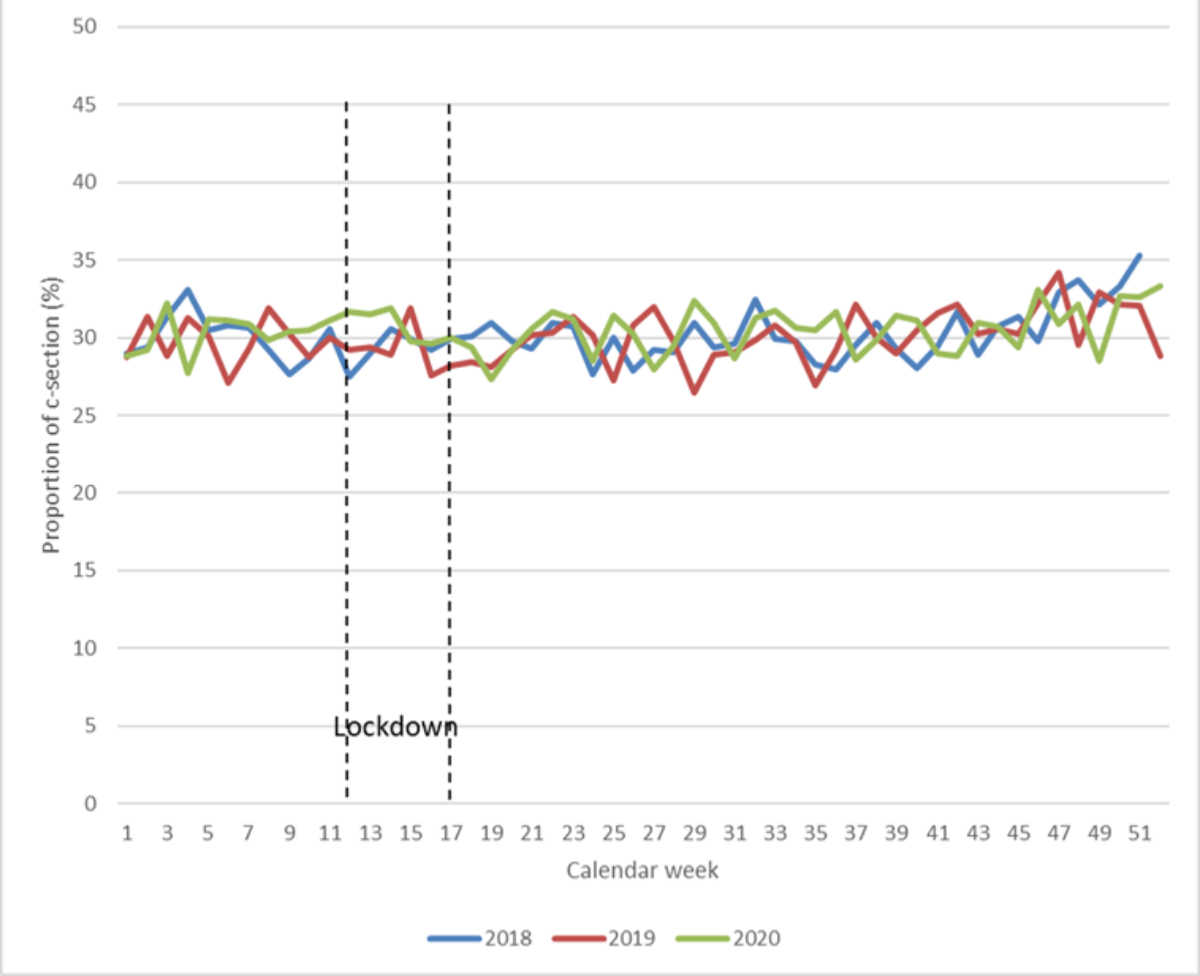
Figure 4Weekly proportion of Caesarean sections (C-sections) between 2018 and 2020 in Switzerland.
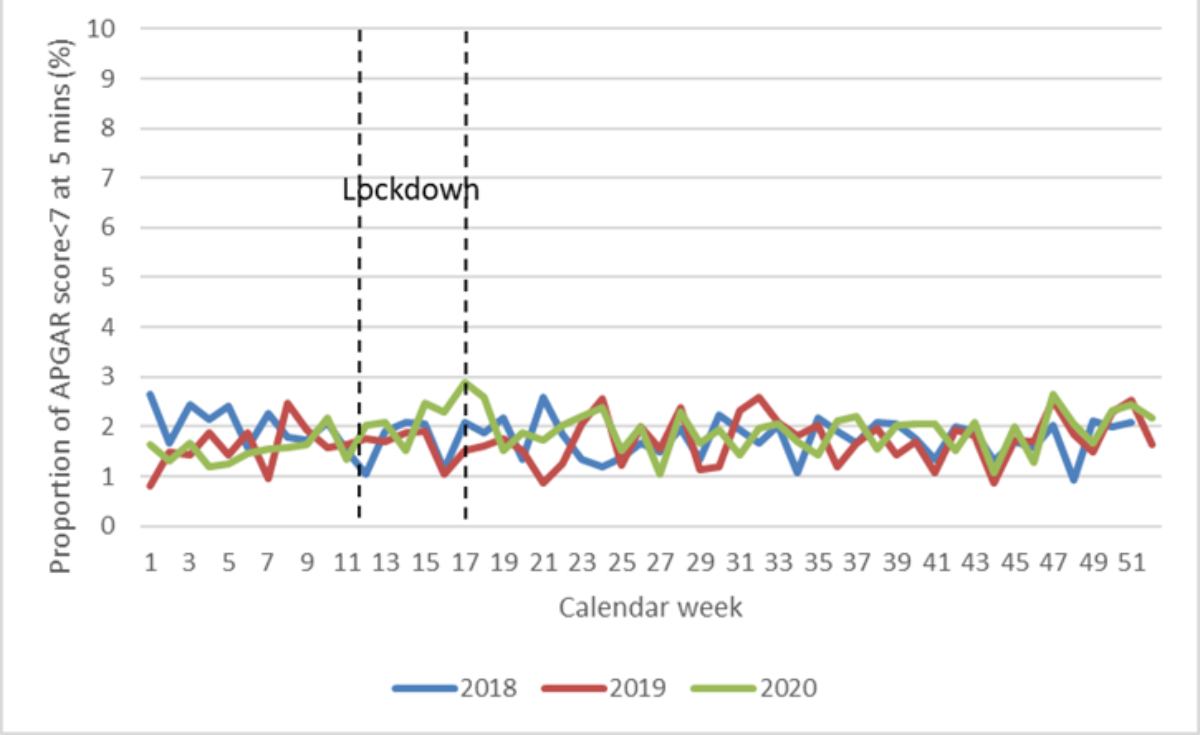
Figure 5Weekly proportion of newborns with a moderate/low Apgar score (<7) at 5 minutes between 2018 and 2020 in Switzerland.
We did not observe an association between the lockdown period and the proportion of C-sections overall and after stratification into planned and unplanned C-sections (figures 2A and 2C, figure 4, table S3). This was true for Switzerland overall and after stratification by region.
Figure 5 shows a slightly higher proportion of newborns with a moderately reduced or low Apgar score (<7) at 5 minutes of age during the lockdown (calendar weeks 12–17) compared to the same period in 2018/2019. Logistic regression analysis (figure 2A and table S3) revealed a statistically significantly increased risk of an Apgar score <7 at 5 minutes during the lockdown period (OR: 1.41, 95% CI: 1.19–1.69). These results were robust to a shortening and lengthening of the lockdown period to 6 and 10 weeks, as well as in two sensitivity analyses (table S3), in which we excluded (1) preterm infants born <37 weeks of gestation and (2) all births in 2018. The corresponding association was stronger for Apgar scores at 10 minutes of age (OR: 1.94, 95% CI: 1.46–2.59, table S3 and appendix figure S2). Furthermore, proportions of newborns with a low Apgar score (<5) at 5 minutes and 10 minutes of age during the lockdown period were also increased, resulting in ORs of 1.58 (95% CI: 1.17–2.15) and 1.89 (95% CI: 1.24–2.86, table S3).
During the lockdown period, the risk of a 5-minute Apgar score <7 was strongly increased in the canton of Ticino with an OR of 4.60 (95% CI: 1.70–12.34), but the sample size was small (figure 2D, table S3). In the German-speaking part of Switzerland, we observed an OR of 1.43 (95% CI: 1.16–1.77), which was driven by increased ORs in the canton of Bern (OR: 2.84, 95% CI: 1.79–4.48) whereas ORs were not meaningfully changed in other German-speaking parts of Switzerland. In the French-speaking part of Switzerland, an increased risk for a 5-minute Apgar score <7 was observed for the canton of Geneva (OR: 2.40, 95% CI: 1.20–4.70, table S3).
The proportion of missing Apgar scores did not differ between the lockdown period from 16 March 2020 to 10 May 2020 (15.8%) and the entire calendar year of 2020 (15.6%). Also, the monthly proportion of all women who received postpartum outpatient midwife care of all women who gave birth did not differ during the lockdown period compared to the baseline period in all of Switzerland or in Ticino specifically (data not shown).
This nationwide observational study included over 85% of all singleton births in Switzerland between 2018 and 2020. We did not observe a sizeable country-wide change in the incidence of adverse birth outcomes during the COVID-19-related lockdown between 16 March and 10 May 2020. However, in the canton of Ticino, we observed a 2-fold increase in the risk of preterm birth (<37 weeks) and a 4.6-fold increase in the proportion of newborns with an Apgar score <7 at 5 minutes during the lockdown period in 2020. The canton of Ticino borders northern Italy and had the highest number of COVID-19 infections during this time, but the increased risks are based on a small sample size [25]. Preterm births were not increased in other regions of Switzerland, whereas Apgar scores <7 were also more frequent in Bern (2.8-fold) and Geneva (2.4-fold). C-sections were not increased during the lockdown.
Preterm birth has been the most studied birth outcome in association with lockdowns in different countries, with varying results. Many studies reported a decreased risk of preterm birth during lockdowns, but they were based on non-representative data from selected hospitals and thus likely skewed, as high-risk births may have been unequally distributed across clinics [2–6, 9].
The international iPOP study evaluated harmonised data from 26 countries (52 million births) between 2015 and 2020. In total, 98.6% of all births originated from 18 population-based datasets from different countries/regions [12]. Results differed between population-based studies vs studies from single treatment centres or other non-population-based data sources. The iPOP study quantified a statistically significant 3–4% decrease in preterm births during the first three months of lockdown among representative data of high-income countries, including 486,357 births from Switzerland (BEVNAT). This reduced overall proportion of preterm births was driven by a large number of births (>20 million) from the US, whereas no association between preterm birth and the lockdown was observed in Switzerland and in most other high-income countries included [12]. Another large Scandinavian study also yielded no change in the proportion of preterm births during the initial COVID-19 lockdown in Denmark, Sweden, and Norway [26].
Our study confirmed the absence of a sizeable overall change in the risk of preterm birth in Switzerland during the first COVID-19 lockdown. However, we observed a doubling of the risk of preterm birth (<37 weeks) in the canton of Ticino, which borders northern Italy, where the number of COVID-19 infections was highest during the first wave of COVID-19 in 2020 [25]. It is possible that COVID-19 infections in pregnant women may account for some preterm births [27]. However, the number of pregnant women infected with COVID-19 during the early pandemic remains unknown, and COVID-19 infections are not captured in this dataset [28]. Moreover, a study from northern Italy reported a decreased risk of preterm birth during the first year of the COVID-19 pandemic [7]. Another possibility is that pregnant women may have been reluctant to seek medical care, and impending preterm births might have been attended to later than usual. It is also possible that other changes in the provision of healthcare during this time led to this increase. Third, a change in the proportion of preterm births may be related to an inverse change in the number of stillbirths, as medical interventions to induce birth early are often implemented when a woman is at risk of stillbirth. Stillbirths are not reliably captured in the Swiss statistics of independent midwives. The number of stillbirths in Switzerland was low, between 3.7 and 4.3 per 1000 births in 2018–2020 [29], and the iPOP study showed no statistically significant change in monthly stillbirths during the lockdown period in Switzerland [12]. However, we are unable to analyse any association between the lockdown and the proportion of stillbirths in Switzerland or in Ticino specifically. Finally, the increased proportion of preterm births in Ticino is based on a small number of women who gave birth during the lockdown in this canton (n = 217), and a chance finding cannot be ruled out. Further studies are needed to verify this result and to get to the bottom of the cause for this association.
The association between local lockdowns and the risks of maternal and neonatal birth outcomes might differ by country and even by region, depending on the stringency of the lockdown, the infectious burden of COVID-19, or other aspects pertinent to local healthcare systems. Compared to other countries, the nationwide lockdown, which started on 16 March in Switzerland, was rather “mild” (table S1) [17], and the number of infections remained relatively low during the first wave of COVID-19 [28]. Hospitals in most regions of the country never surpassed their capacity limits, and overall recorded fewer hospitalisations compared to previous years due to cancelled interventions [30]. However, the number of COVID-19 infections varied between different regions in Switzerland, with Ticino accounting for the proportionally highest number of COVID-19 infections and declaring a state of emergency with additional restrictions on 11 March 2020, before the rest of Switzerland [25, 31]. It is therefore important to evaluate potential public health impacts of lockdowns at a national or even regional level. Thus, our results are specific to Switzerland and may not be generalisable to other countries.
We did not observe a change in the proportion of planned or unplanned C-sections in Switzerland (approx. 1/3 births) overall or within the German-, French-, or Italian-speaking parts separately during the initial COVID-19 lockdown. We hypothesised that fear of high numbers of COVID-19 cases may have affected planning of elective C-sections, whereas an increase in birth complications could have increased secondary C-sections, but our results suggest that this was not the case. Our finding is in line with a nationwide study from England [32]. On the other hand, a study from Iceland reported a 32% decrease in planned C-sections during COVID-19 lockdowns [33], highlighting how differently healthcare systems reacted to lockdowns, and that in some countries elective C-sections were performed less frequently whereas in others this was not the case. A nationwide study from Iran even reported a 2% increase in the proportion of C-sections during the first wave of the COVID-19 pandemic compared to previous years [34]. A previous observational study at a large city hospital in Zurich reported an 8% reduction in planned and unplanned C-sections, which may have been due to channelling of pregnant women or by changes in the management of births at this hospital. The authors did report some relatively small changes in the demographic characteristics of pregnant women and a slight increase in the proportion of birth inductions (29.3% vs 26.9%) during the lockdown vs 2018/2019 [14]. Of note, great regional differences exist in the proportion of C-sections across Switzerland, with proportions between 13% and 53% at the municipality level [35].
Finally, we observed an increased proportion of moderately reduced/low Apgar scores (<7) at 5 minutes of age during the lockdown for the cantons of Ticino (4.6-fold), Geneva (2.4-fold) and Bern (2.8-fold), but no meaningful change for the rest of Switzerland. Interestingly, after Ticino, Geneva was the canton with the second highest infection numbers during the first wave of COVID-19 [28]. This regional distribution of changes in Apgar scores suggests that our results are not pure chance findings. Several mechanisms may explain these findings; it is possible that there might have been changes in the quality of neonatal healthcare right after birth in regions/healthcare facilities highly affected by COVID-19. Furthermore, it is possible that COVID-19 infections in pregnant women may have led to reduced Apgar scores. However, changes in staff or routines during the lockdown may have led to inconsistencies in the recording of lower Apgar scores in some cases. It is a known problem that Apgar scores are not an exact measure and are subject to large inter-rater variability and subjectivity. Moreover, despite their common use, their ability to predict clinical outcomes is limited [23]. Thus, these results have to be interpreted cautiously [36]. Moreover, the absolute excess number of newborns with moderately reduced or low Apgar scores during the lockdown vs 2018/2019 was small.
This study is based on a nationwide database. A prior validation study has shown that all outcomes of interest in this study are reliably captured in the database (table S2). Nevertheless, certain limitations need to be considered. First, we did not have information on COVID-19 infections, which are an individual risk factor for birth complications [12]. Second, we did not have information available on the actual birth facility or the attending midwife/physician, and we therefore cannot infer upon differences in risk by specific birth facilities. Third, we only had data between 2018 and 2020 available. Having more pre-pandemic years available would have made analyses more robust. Fourth, it is possible that women left the hospital earlier and that more women who would otherwise have remained hospitalised may have received postpartum outpatient midwife care instead. On the other hand, it is possible that women may have decided not to see a midwife in their home due to fear of infection. However, the monthly proportion of women with postpartum midwife care remained stable when comparing before vs during the lockdown in Switzerland overall and in Ticino specifically. Thus, our results are unlikely altered due to increased or decreased midwife care of women with preterm births or other complications during the lockdown period. However, the statistics of outpatient midwifery services may not cover some women with severe birth complications who remain hospitalised for an extended period of time, and thus our results may not be generalisable to these women. Fifth, other maternal outcomes, which would have been of interest, such as psychological or lactation problems during the postpartum period, are not reliably captured in the database. Finally, we did not evaluate the course of birth outcomes after the first lockdown. It is possible that the risk of certain birth outcomes changed during the second lockdown in late 2020, and future studies should evaluate these associations.
This observational study included over 85% of all births in Switzerland between 2018 and 2020. Our results suggest no change in the risk of preterm birth, C-section, or reduced Apgar scores at 5 minutes during the first COVID-19 lockdown in Switzerland in 2020. Increased risks of preterm birth during the lockdown were recorded in the canton of Ticino, which borders northern Italy, and was the region with the highest COVID-19 burden in Switzerland during that time. However, the absolute number of infants born in Ticino during this time was small and a chance finding cannot be ruled out.
The study data belong to the Swiss Federation of Midwives. Access and/or use is only possible under contractually agreed conditions.
We thank the Swiss Federation of Midwives for providing us with the anonymised statistics of outpatient midwifery services in Switzerland and the “Freiwillige Akademische Gesellschaft Basel (FAG)” for supporting our study with a research grant. We thank PD Dr Christian Schindler, senior statistician at the Swiss Tropical and Public Health Institute, for his support with development and interpretation of statistical models.
This work was financially supported by the “Freiwillige Akademische Gesellschaft Basel (FAG)”.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Hedermann G, Hedley PL, Bækvad-Hansen M, Hjalgrim H, Rostgaard K, Poorisrisak P, et al. Danish premature birth rates during the COVID-19 lockdown. Arch Dis Child Fetal Neonatal Ed. 2021 Jan;106(1):93–5. doi: https://doi.org/10.1136/archdischild-2020-319990
2. Been JV, Burgos Ochoa L, Bertens LC, Schoenmakers S, Steegers EA, Reiss IK. Impact of COVID-19 mitigation measures on the incidence of preterm birth: a national quasi-experimental study. Lancet Public Health. 2020 Nov;5(11):e604–11.
3. Matheson A, McGannon CJ, Malhotra A, Palmer KR, Stewart AE, Wallace EM, et al. Prematurity Rates During the Coronavirus Disease 2019 (COVID-19) Pandemic Lockdown in Melbourne, Australia. Obstet Gynecol. 2021 Mar;137(3):405–7. doi: https://doi.org/10.1097/AOG.0000000000004236
4. Einarsdóttir K, Swift EM, Zoega H. Changes in obstetric interventions and preterm birth during COVID-19: A nationwide study from Iceland. Acta Obstet Gynecol Scand. 2021 Oct;100(10):1924–30. doi: https://doi.org/10.1111/aogs.14231
5. Cuestas E, Gómez-Flores ME, Charras MD, Peyrano AJ, Montenegro C, Sosa-Boye I, et al. Association between COVID-19 mandatory lockdown and decreased incidence of preterm births and neonatal mortality. J Perinatol. 2021 Oct;41(10):2566–9.
6. Meyer R, Bart Y, Tsur A, Yinon Y, Friedrich L, Maixner N, et al. A marked decrease in preterm deliveries during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol. 2021 Feb;224(2):234–7. doi: https://doi.org/10.1016/j.ajog.2020.10.017
7. Rusconi F, Puglia M, Pacifici M, Brescianini S, Gagliardi L, Nannavecchia AM, et al.; AIE Perinatal Health Working Group. Pregnancy outcomes in Italy during COVID-19 pandemic: a population-based cohort study. BJOG. 2022 Oct;130(3):276–84. doi: https://doi.org/10.1111/1471-0528.17315
8. Pasternak B, Neovius M, Söderling J, Ahlberg M, Norman M, Ludvigsson JF, et al. Preterm Birth and Stillbirth During the COVID-19 Pandemic in Sweden: A Nationwide Cohort Study. Ann Intern Med. 2021 Jun;174(6):873–5. doi: https://doi.org/10.7326/M20-6367
9. De Curtis M, Villani L, Polo A. Increase of stillbirth and decrease of late preterm infants during the COVID-19 pandemic lockdown. Arch Dis Child Fetal Neonatol Ed. 2021 Jul;106(4):456. doi: https://doi.org/10.1136/archdischild-2020-320682.
10. Main EK, Chang SC, Carpenter AM, Wise PH, Stevenson DK, Shaw GM, et al. Singleton preterm birth rates for racial and ethnic groups during the coronavirus disease 2019 pandemic in California. Am J Obstet Gynecol. 2021 Feb;224(2):239–41. doi: https://doi.org/10.1016/j.ajog.2020.10.033
11. Briozzo L, Tomasso G, Viroga S, Nozar F, Bianchi A. Impact of mitigation measures against the COVID 19 pandemic on the perinatal results of the reference maternity hospital in Uruguay. J Matern Fetal Neonatal Med. 2022 Dec;35(25):5060–2. doi: https://doi.org/10.1080/14767058.2021.1874911
12. Calvert C, Brockway MM, Zoega H, Miller JE, Been JV, Amegah AK, et al. Changes in preterm birth and stillbirth during COVID-19 lockdowns in 26 countries. Nat Hum Behav. 2023 Apr;7(4):529–44. doi: https://doi.org/10.1038/s41562-023-01522-y
13. Adams M, Schulzke SM, Rogdo B, Meyer P, McDougall J, Stocker M, et al.; Swiss Neonatal Network. Impact of SARS-CoV-2 on incidence, treatment and outcome of very preterm born infants in Switzerland: a retrospective, population-based cohort study. Swiss Med Wkly. 2022 May;152(19–20):w30174. doi: https://doi.org/10.4414/SMW.2022.w30174
14. Cincera T, Conde N, von Felten S, Leeners B, von Orelli S. Did the first wave of the COVID-19 pandemic impact the cesarean delivery rate? A retrospective cohort study at a primary care center in Switzerland. J Perinat Med. 2022 Dec;51(5):614–22.
15. Swiss Federal Authorities. Die Bundesversammlung der Schweizerischen Eidgenossenschaft. SR 818.101. Federal Act of 28 September 2012 on Controlling Communicable Human Diseases (Epidemics Act, EpidA). Available from: https://www.fedlex.admin.ch/eli/cc/2015/297/en
16. Bundesamt für Gesundheit (BAG). BAG: Massnahmen und Verordnungen [Internet]. 2022 [cited 2023 Sep 5]. Available from: https://www.bag.admin.ch/bag/de/home/gesetze-und-bewilligungen/gesetzgebung/gesetzgebung-mensch-gesundheit/gesetzgebung-covid-19.html#-1876551640
17. Coronavirus: Bundesrat erklärt die «ausserordentliche Lage» und verschärft die Massnahmen [Internet]. 2020 [cited 2023 Aug 8]. Available from: https://www.bag.admin.ch/bag/en/home/das-bag/aktuell/medienmitteilungen.msg-id-78454.html
18. Statistik der Frei Praktizierenden Hebammen fpH [Internet]. 2018 [cited 2018 Aug 14]. Available from: http://www.hebamme.ch/de/heb/shv/stats.cfm
19. Grylka-Bäschlin S, Borner B. Ausführlicher Statistikbericht der frei praktizierenden Hebammen der Schweiz [Internet]. 2020 [cited 2023 Sep 5]. Available from: https://www.hebamme.ch/verbandsnews/statistikbericht-der-frei-praktizierenden-hebammen-der-schweiz-2020/
20. Grylka-Baeschlin S, Iglesias C, Erdin R, Pehlke-Milde J. Evaluation of a midwifery network to guarantee outpatient postpartum care: a mixed methods study. BMC Health Serv Res. 2020 Jun;20(1):565. doi: https://doi.org/10.1186/s12913-020-05359-3
21. Grylka-Bäschlin S, Borner B. Statistics of independent midwives in Switzerland [Internet]. [cited 2023 Oct 4]. Available from: https://www.zhaw.ch/en/health/health-research-and-development/midwifery/projects/statistics-of-independent-midwives-in-switzerland/
22. Bundesamt für Statistik BFS. Gesundheit der Neugeborenen [Internet]. [cited 2025 Apr 17]. Available from: https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/gesundheitszustand/gesundheit-neugeborenen.html
23. Michel A. Review of the Reliability and Validity of the Apgar Score. Adv Neonatal Care. 2022 Feb;22(1):28–34. doi: https://doi.org/10.1097/ANC.0000000000000859
24. Wing C, Simon K, Bello-Gomez RA. Designing Difference in Difference Studies: Best Practices for Public Health Policy Research. Annu Rev Public Health. 2018 Apr;39(1):453–69. doi: https://doi.org/10.1146/annurev-publhealth-040617-013507
25. Giachino M, Valera CB, Rodriguez Velásquez S, Dohrendorf-Wyss MA, Rozanova L, Flahault A. Understanding the dynamics of the covid-19 pandemic: A real-time analysis of switzerland’s first wave. Int J Environ Res Public Health. 2020 Nov;17(23):1–17. doi: https://doi.org/10.3390/ijerph17238825
26. Oakley LL, Örtqvist AK, Kinge J, Hansen AV, Petersen TG, Söderling J, et al. Preterm birth after the introduction of COVID-19 mitigation measures in Norway, Sweden, and Denmark: a registry-based difference-in-differences study. Am J Obstet Gynecol. 2022 Apr;226(4):550.e1–22.
27. Menter T, Mertz KD, Jiang S, Chen H, Monod C, Tzankov A, et al. Placental Pathology Findings during and after SARS-CoV-2 Infection: Features of Villitis and Malperfusion. Pathobiology. 2021;88(1):69–77. doi: https://doi.org/10.1159/000511324
28. Probst D. Corona-data.ch [Internet]. 2020. Available from: https://corona-data.ch/
29. Statistik B für. Säuglingssterblichkeit, Totgeburten [Internet]. 2023 [cited 2023 Sep 5]. Available from: https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/gesundheitszustand/sterblichkeit-todesursachen/saeuglings-totgeburten.html
30. Bähler C, Elmiger M, Signorell A. Helsana-Report: Corona. Auswirkungen der Corona-Pandemie auf die medizinsche Versorgung in der Schweiz [Internet]. 2021. Available from: https://reports.helsana.ch/wp-content/uploads/2021/09/Helsana-Report-Corona-Gesamtreport.pdf
31. Bergamin F, Mazidi S. Kompetenzabgrenzung zwischen Bund und Kantonen bei der Bekämpfung von Epidemien: Erste Einschätzungen unter besonderer Berücksichtigung der COVID-19-Verordnungen. Institut für Föderalismus. aus Sonderausgabe Newsletter IFF 2/2020. Vol. 41. Available from: https://www.unifr.ch/federalism/de/assets/public/files/Newsletter/IFF/Bergamin.Mazidi_Kompetenzabgrenzung%20zwischen%20Bund%20und%20Kantonen_COVID-19.pdf
32. Chmielewska B, Barratt I, Townsend R, Kalafat E, van der Meulen J, Gurol-Urganci I, et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Health. 2021 Jun;9(6):e759–72.
33. Einarsdóttir K, Swift EM, Zoega H. Changes in obstetric interventions and preterm birth during COVID-19: A nationwide study from Iceland. Acta Obstet Gynecol Scand. 2021 Oct;100(10):1924–30. doi: https://doi.org/10.1111/aogs.14231
34. Gharacheh M, Kalan ME, Khalili N, Ranjbar F. An increase in cesarean section rate during the first wave of COVID-19 pandemic in Iran. BMC Public Health. 2023 May;23(1):936. doi: https://doi.org/10.1186/s12889-023-15907-1
35. Bundesamt für Statistik BFS. Anzahl und Rate der Kaiserschnitte nach Kanton und Wohnregion [Internet]. [cited 2025 Apr 17]. Available from: https://www.bfs.admin.ch/bfs/fr/home/actualites/quoi-de-neuf.assetdetail.28625247.html
36. Livingston J. Interrater reliability of the Apgar score in term and premature infants. Appl Nurs Res. 1990 Nov;3(4):164–5. doi: https://doi.org/10.1016/S0897-1897(05)80139-9
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.4319.