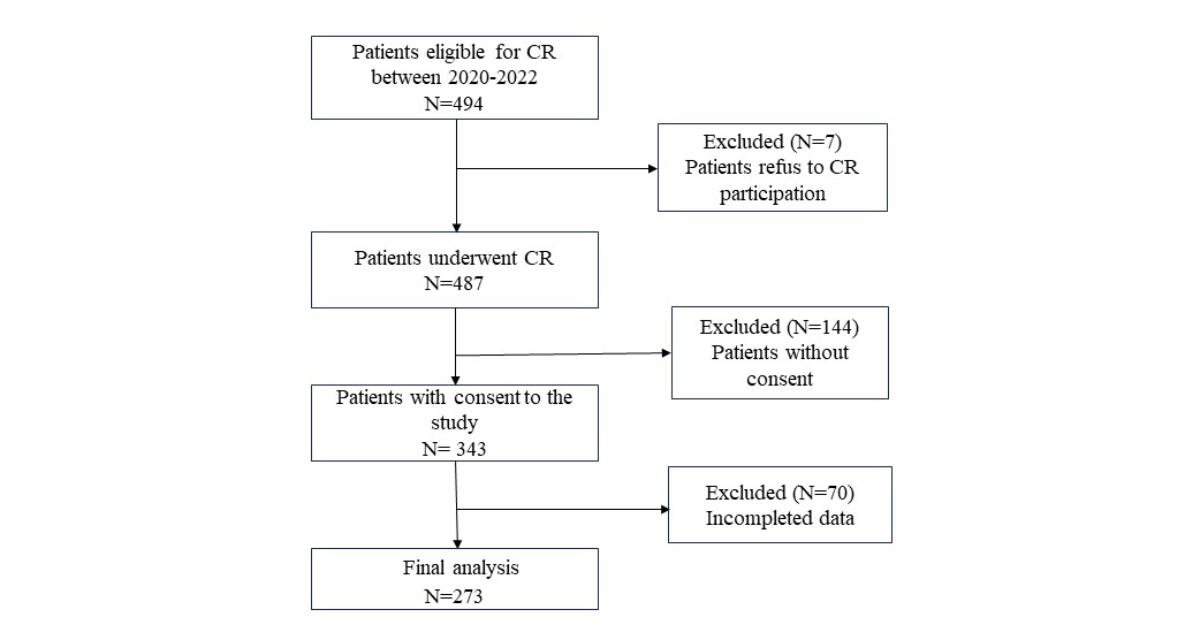
Figure 1Study flowchart.
DOI: https://doi.org/https://doi.org/10.57187/s.4160
Cardiovascular diseases are the most common cause of death and the third cause of hospitalisation in Switzerland [1]. A meta-analysis of 63 randomised controlled trials suggested that cardiac rehabilitation could significantly reduce cardiovascular mortality (relative risk: 0.74;95% confidence interval [CI]: 0.64–0.86) and hospital admissions (relative risk: 0.82;95% CI: 0.70–0.96) and improve quality of life (QoL) [2].
Functional capacity reflects an individual’s tolerance to perform activities under aerobic metabolism like walking, exercising or maintaining a body position [3]. It can be assessed by various measurements including the 6-minute walk test (6MWT), estimated metabolic equivalent of task (eMET), maximal short-term exercise capacity and maximal quadriceps isometric strength. Patients with cardiac diseases often demonstrate impaired functional capacity that could lead to a reduction in social or daily activities [4]. Improvements in functional capacity indicators, such as the 6-minute walk test and eMET, have been demonstrated in patients undergoing exercise-based cardiac rehabilitation programmes [5, 6], but few studies have reported the latter two tests (maximal short-term exercise capacity and quadriceps isometric strength) after completion of a cardiac rehabilitation programme. A change in these parameters after a cardiac rehabilitation programme should be evaluated.
In addition to objective measurements, patient-reported outcome measures (PROMs) including quality of life, depression, anxiety and level of physical activity are outcomes of interest because they are associated with mortality rate, hospitalisation and healthcare expenditures in patients with cardiac diseases [7–9]. According to a meta-analysis of 12 randomised controlled trials, the mean values for depression and anxiety significantly decreased (−0.34 points) in individuals with cardiovascular diseases after completing cardiac rehabilitation [10]. Physical activity also improved on discharge from a cardiac rehabilitation programme [11]. However, it remains unclear whether these improvements are maintained over time.
Factors associated with quality of life in patients who underwent cardiac rehabilitation were age, sex, number of comorbidities, psychological distress and physical activity [12–14]. Previous studies have also showed a significant association of functional capacity indicators, including eMET [15] and peak oxygen uptake [16], with quality of life. However, these studies were based on cross-sectional designs [15, 16], and did not assess changes in variables over time. A follow-up study could assess the changes in these parameters across different time points and provide a comprehensive predictive model.
According to a 2019 report by the European Association of Preventive Cardiology, cardiac rehabilitation was available in 90% (40/44) of European countries, albeit with regional variations [17]. On average, cardiac rehabilitation programmes had a multidisciplinary team of 6.5 staff members and offered 8.5 of 10 core components over a duration of 24.8 hours. Participation in either inpatient or outpatient cardiac rehabilitation yielded comparable results in terms of cardiac mortality and morbidity, functional capacity and physical activity [18]. In Switzerland, the cardiac rehabilitation programme follows the guidelines proposed by the Swiss Working Group for Cardiovascular Prevention, Rehabilitation and Sports Cardiology (SCPRS) [19]. A 2023 Swiss report from 82 registered centres of 133,060 participants showed that cardiac rehabilitation programmes could improve functional capacity, quality of life and smoking cessation rates [20]. However, there are some shortcomings concerning this registry database. Most data represent means or medians of each centre, rather than individual data. Additionally, the use of various questionnaires in registry databases could lead to data heterogeneity. Analysing individual data from medical records might overcome these shortcomings.
To this end, we aimed to assess changes in functional capacity (6-minute walk test, eMET, maximal short-term exercise capacity, quadriceps isometric strength) upon discharge and in PROMs (depression, anxiety, quality of life, level of physical activity) at 6-month follow-up among outpatients who had completed cardiac rehabilitation in a prospective study. Additionally, we evaluated factors associated with changes in quality of life using a multi-level mixed-effects generalised linear model adjusted for age, sex and time points.
This was a prospective study of outpatients who had completed a cardiac rehabilitation programme in a tertiary care rehabilitation clinic from October 2020 to October 2022. People with various cardiac diseases after acute hospitalisation at the Centre Hospitalier du Valais Romand (CHVR) were screened for eligibility for the cardiac rehabilitation programme at the nearby tertiary care rehabilitation centre.
Inclusion criteria were: age 18 to 75 years; heart diseases including acute coronary syndromes with or without percutaneous transluminal coronary angioplasty, heart surgery (mitral valve, aortic valve, intervention on large vessels), chronic coronary artery disease, primary prevention of cardiovascular disease and cardiac insufficiency. All patients were able to understand and sign an informed consent form.
Exclusion criteria were: under legal custody, unstable or life-threatening non-cardiovascular conditions including active infection, uncontrolled diabetes or end-stage cancer, unstable angina, uncontrolled malignant ventricular arrhythmias, overt cardiac insufficiency not controlled by medication, unoperated severe aortic valve stenosis, lung disease with severe hypoxia, ancillary conditions that are adversely affected by physical activity or that prohibit physical activity, substantial locomotor disability or physical dependence and insufficient potential for independence and reintegration and finally severe psychopathy or drug addiction with uncontrolled overt addiction. Moreover, we also excluded patients who had not performed functional tests at entry or discharge.
We collected baseline data (age, sex, diagnoses, smoking status at entry) at admission. Our primary outcomes were functional capacity including the 6-minute walk test [21], maximal short-term exercise capacity [22], eMET [23] and maximal quadriceps isometric strength [24] at entry and discharge; and PROMs including the Hospital Anxiety and Depression Scale (HADS), heart-related quality of life (HeartQuL), Baecke questionnaire; at entry, discharge and 6 months later.
The eMET was calculated by using the exercise stress test on the treadmill (h/p cosmos, Nussdorf – Traunstein, Germany) according to the Bruce protocol [23]. The protocol comprises 7 exercise stages of three minutes each. At each stage, the speed and gradient of the treadmill are increased to increase work output. For example, stage 1 of the Bruce protocol is performed at 2.7 km per hour (kph) with a 10% incline, stage 2 at 4 kph and 12%, stage 3 at 5.5 kph and 14%, etc. Heart rate and respiratory rate are constantly assessed; blood pressure and electrocardiogram (ECG) are taken at rest, after each stage and during recovery for at least 5 minutes or until return to baseline. The test stops if the individual shows signs or symptoms of impaired blood flow to the heart, irregular heart rhythm, fatigue, shortness of breath, wheezing, leg cramps or chest discomfort. The following Bruce protocol-specific equation accounts for handrail use: eMETs = (2.587 × TT + 6.004)/3.5, where TT is exercise time in minutes [3].
The 6-minute walk test [21] is a reliable and validated submaximal exercise test for patients with cardiac disease. Participants were instructed to walk as fast and as far as they could do for 6 minutes on a 120-metre walking track. The distance walked was recorded in metres.
The maximal short-term exercise capacity [25] is determined using an ergometer steep ramp test (SRT) (Ergoline GmbH, Ergoline, Germany). After a warm-up of 2 minutes of unloaded cycling, the resistance was progressively increased (25 W/10 s). Patients were instructed to cycle until exhaustion with a pedal frequency of 60–80 rotations per minute (rpm). The test was stopped when the pedal frequency dropped under 60 rpm. The steep ramp test is a practicable, reliable and validated test for the assessment of the training dose [25].
The maximal quadriceps isometric strength [24] was measured with an isometric measurement device (Easytorque, Fa. Tonus, Zemmer, Germany) with the individual in a sitting position. The knee angle was set to 80° to measure knee flexion and 90° for knee extension. The thighs were fixed with pads and the calves were pressed isometrically against the pads, thus against the force transducers. The individual had to build up strength for 5 s and hold it for 5 s more. Both sides were tested alternately. Three isometric measurements were taken for each side, and the maximum value achieved was retained. The correlation between measurements with a fixed handheld dynamometer and the isokinetic dynamometer method were statistically significant [26].
The HADS [27] was used to assess the level of depression and anxiety. The HADS includes 7 items related to symptoms of anxiety and 7 to symptoms of depression. Scores range from 0 to 21, with higher scores indicating greater symptom severity. A score ≥8 indicates possible or probable clinically relevant anxiety and/or depression [28].
The heart-related quality of life [29, 30] questionnaire is a 14-item self-assessment questionnaire used to measure health-related quality of life. The scale includes a 10-item physical subscale (Cronbach’s alpha: 0.91) and a 4-item emotional subscale (Cronbach’s alpha: 0.87) [31]. Items are rated on a 4-point Likert scale (range 0–3), with higher scores indicating higher quality of life. Scores for each subscale are calculated as the mean of items. The heart-related quality of life questionnaire has been validated in the EuroAspire IV Health Survey in 7449 stable coronary patients [31].
The Baecke questionnaire [32] contains 16 questions distributed across 3 domains: physical activity at work (items 1–8), physical activity in sports (items 9–12) and leisure-time physical activity excluding sports (items 13–16). Each item is scored on a Likert scale ranging from 1 to 5 and a specific formula provides a score between 1 and 5 for each assessed domain.
The work domain score is calculated by summing the responses in the domain (for item 2, the value used is the response subtracted from 6) and then dividing by 8. The sports domain score is computed by summing the values and dividing by 4. To calculate the leisure domain score, the summed values (for item 13, the value used is the response subtracted from 6) are divided by 4. For each domain, the final score ranges from 1 to 5, with a higher score indicating a higher level of physical activity [32].
The cardiac rehabilitation programme is a multidisciplinary approach developed according to the SCPRS guidelines [19]. The cardiac rehabilitation team consisted of different healthcare professionals (cardiologists, angiologists, physiotherapists, sports instructors, nurses, psychiatrists, psychologists, dieticians, biologists). The programme lasts 10 weeks, with 3 half-days of treatment per week. It consists of exercise (aerobic and resistance training), psychiatric intervention (stress management) and therapeutic education (cardiac physiology and pathology, medications, cardiovascular risk factors, diet). The exercise training includes nearly 70 hours of gym and water exercises, outdoor walking and relaxation sessions. There are five groups of different intensity levels that are adapted to the specific needs of the person, their state of health and evolution. The training is carried out with a maximum of 13 people; each session lasts 40 minutes. There is one excursion of 1.5 hour per week. Therapeutic education is provided in an interactive way to enable people to adopt habits that are sustainable and favourable to health.
This is an exploratory study, and we did not calculate the sample size beforehand. Categorical variables (sex, cardiac diagnoses, intervention, smoking status at entry) are presented with counts (%). Normal distribution was checked using the Shapiro-Wilk tests. Continuous variables including age, functional capacity tests and PROMs were not normally distributed and are presented as median and interquartile range (IQR, the 25th to 75th percentile).
We used Wilcoxon signed-rank tests to compare functional capacity (6-minute walk test, eMET, maximal short-term exercise capacity, quadriceps isometric strength) between discharge and entry level; and Kruskal-Wallis tests to compare the PROMs between three time points (entry, discharge, 6 months), followed by Dunn’s post-hoc tests with Bonferroni corrections for multiple comparisons.
The frequencies of missing data were as follow: functional tests (quadriceps isometric strength, eMET: 18%): HADS: 22%, heart-related quality of life: 29%, Baecke: 30%. We used complete case analysis to address missing data.
We used multilevel mixed-effects generalised linear models to assess factors associated with physical and emotional domains of heart-related quality of life. The two models included age, sex, time point, smoking status at entry, functional capacity, level of depression and anxiety, physical activity as fixed effects and subjects as random intercept. The significance level for all tests was 0.05. This model allows regression analyses on dependent variables that are non-normally distributed for longitudinal data [33]. We applied a logarithmic link (to transform outcomes into normally distributed variables) and a gaussian function in the models, using the meglm command in STATA 18.0 for Windows (Stata Corp., College Station, TX, USA). For interpretation, the β coefficient was backtransformed and presented as expβ. The coefficients in the model estimate the average change of response variable for every 1-unit increase in a covariate.
All participants provided written consent. The study protocol was approved by the local ethics committee (Commission cantonale d’éthique de la recherche sur l’être humain CER-VD Lausanne, Project-ID 2020-02155). The investigation conforms to the principles outlined in the Declaration of Helsinki [34].
Among 494 participants screened for eligibility for the cardiac rehabilitation programme during the study period, 7 patients refused to participate and 144 did not give consent for the study. Another 70 patients who did not perform functional tests at entry or discharge were also excluded.
A total of 273 participants were included in the final analysis. Figure 1 presents the flowchart of the study. The median time from acute hospitalisation to cardiac rehabilitation participation was 1.4 months (IQR: 1.1–2.0). The median age was 63 years (range: 57–69), 81% of participants were men and 32% were smokers. About two-thirds of the participants (76%) had a diagnosis of acute coronary syndrome with or without percutaneous coronary intervention (ACS ± PCI) (table 1).
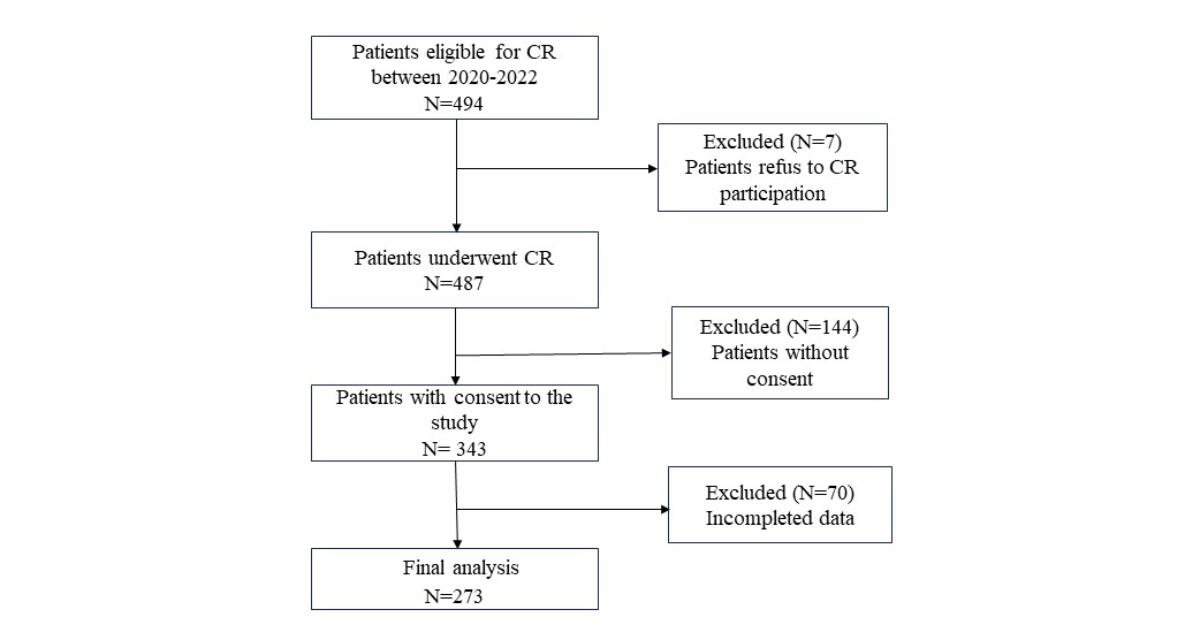
Figure 1Study flowchart.
Table 1Baseline characteristics of participants (n = 273).
| Variables | Total (n = 273) | |
| Age in years, median (IQR) | 63 (57–69) | |
| Sex, n (%) | Male | 222 (81%) |
| Female | 51 (19%) | |
| Cardiac intervention, n (%) | Acute coronary syndrome ± PCI | 207 (76%) |
| Heart valve surgery | 31 (11%) | |
| Heart insufficiency | 13 (5%) | |
| Intervention on large vessels | 5 (2%) | |
| Other | 17 (6%) | |
| Smoking at entry, n (%) | Yes | 84 (32%) |
IQR: interquartile range; PCI: percutaneous coronary intervention.
At discharge after the cardiac rehabilitation programme, median changes for the 6-minute walk test were significant (+60 m, 95% confidence interval [CI]: 50–65; p <0.001); similarly for the maximal short-term exercise capacity (+50 W, 95% CI: 50–50; p <0.001), eMET (+0.9, 95% CI: 0.7–1.1; p <0.001), maximal left quadriceps isometric strength (+3 Nm, 95% CI: 2–4; p <0.001) and maximal right quadriceps isometric strength (+4 Nm, 95% CI: 2.4–4.7; p <0.001) (table 2). Figure 2 shows the changes in functional capacity from entry to discharge.
Table 2Functional capacity at entry and discharge from the cardiac rehabilitation programme.
| n | Entry, median (IQR) | Discharge, median (IQR) | Change, median (95% CI) | p-value* | |
| 6-minute walk test (m) | 273 | 560 (500–610) | 630 (570–680) | 60 (50–65) | <0.001 |
| Maximal short-term exercise capacity (W) | 273 | 225 (150–275) | 275 (200–325) | 50 (50–50) | <0.001 |
| Maximal left quadriceps isometric strength (Nm) | 223 | 43 (34–53) | 48 (38–57) | 3 (2–4) | <0.001 |
| Maximal right quadriceps isometric strength (Nm) | 223 | 44 (34–55.5) | 50 (40–58) | 4 (2.4–4.7) | <0.001 |
| eMET | 223 | 8.4 (6.5–10.6) | 10.1 (7.2–11.4) | 0.9 (0.7–1.1) | <0.001 |
CI: confidence interval; eMET: estimated metabolic equivalent of task; IQR: interquartile range.
* Wilcoxon signed-rank tests.
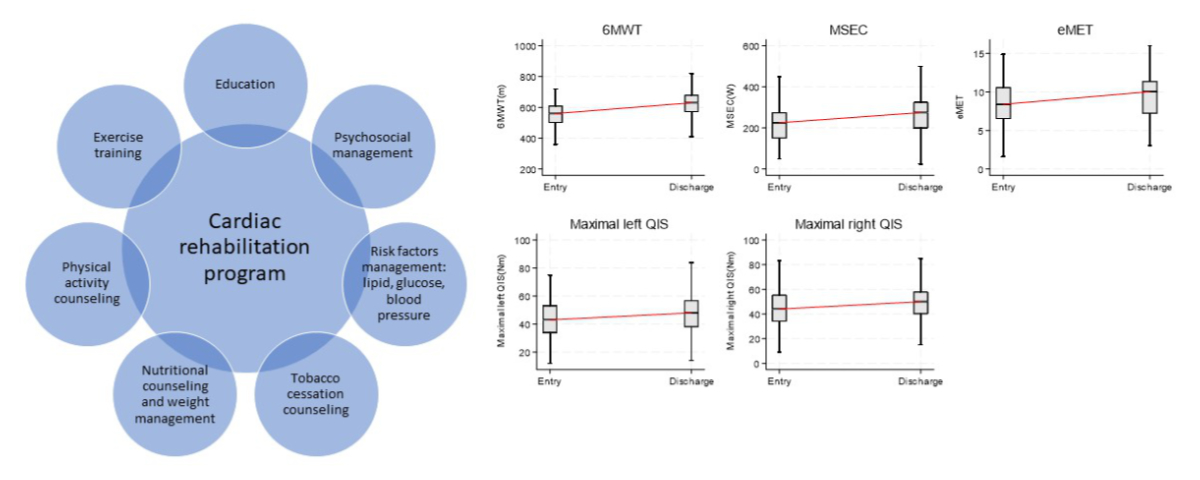
Figure 2Changes in functional capacity from entry to discharge in outpatients with various cardiac diseases. Wilcoxon signed-rank tests between entry and discharge: p-value <0.001 for all functional tests. 6MWT: 6-minute walk test; eMET: estimated metabolic equivalent of task; MSEC: maximal short-term exercise capacity; QIS: quadriceps isometric strength.
The median scores of depression significantly decreased from entry to discharge (from 5 to 4 points, p <0.001) and from entry to 6 months (5 to 4.5 points, p <0.001). The median anxiety scores significantly decreased from entry to discharge (5 to 4 points, p <0.001) and from entry to 6 months (5 to 4 points, p <0.001) (table 3). Differences in median scores of anxiety and depression were not statistically significant between discharge and 6 months.
Table 3Patient-reported outcome measures of depression and anxiety, quality of life and physical activity during the 6-month follow-up.
| Patient-reported outcome measure (PROM) | n | Entry | Discharge | 6-month time point | Kruskal-Wallis tests for 3 groups | |
| Median (IQR) | Median (IQR) | Median (IQR) | p-value | |||
| HADS | Depression | 212 | 5 (3–9) | 4 (2–7) | 4.5 (3–7) | <0.001 |
| Anxiety | 212 | 5 (4–7) | 4 (2–6) | 4 (3– 7) | <0.001 | |
| Heart-related quality of life | Physical | 195 | 19 (15–24) | 24 (20–27) | 25 (19–27) | <0.001 |
| Emotional | 195 | 9 (7–11) | 11 (9–12) | 11 (9–12) | <0.001 | |
| Baecke | Work | 192 | 2.4 (1–3.4) | 2.6 (1.5–3.4) | 2.1 (1–3.4) | 0.05 |
| Sport | 192 | 2.5 (2–3.3) | 2.8 (2–3.3) | 2.8 (2–3.3) | 0.14 | |
| Leisure | 192 | 3.0 (2.3–3.3) | 3.0 (2.7–3.7) | 3.2 (2.7–3.7) | 0.007 | |
HADS: Hospital Anxiety and Depression Scale; IQR: interquartile range.
The median score for the physical domain of quality of life significantly increased from entry to discharge (19 to 24 points, p <0.001) and from entry to 6 months (19 to 25 points, p <0.001). The median score of the emotional domain of quality of life significantly increased from entry to discharge (9 to 11 points, p <0.001) and from entry to 6 months (9 to 11 points, p <0.001) (table 3). Differences in median scores of the physical or emotional domain of quality of life were not statistically significant between discharge and 6 months.
Median scores for work and sports subscales (Baecke) scores did not significantly differ over the 6-month follow-up. The median score for leisure-time physical activity remained unchanged from entry to discharge (3 points) but slightly improved at 6 months (3.0 to 3.2 points, p = 0.007) as compared to the baseline level (table 3). Differences in median scores of leisure-time physical activity were not statistically significant between discharge and 6 months.
Figure 3 shows the changes in PROMs at three time points: entry, discharge and 6 months.
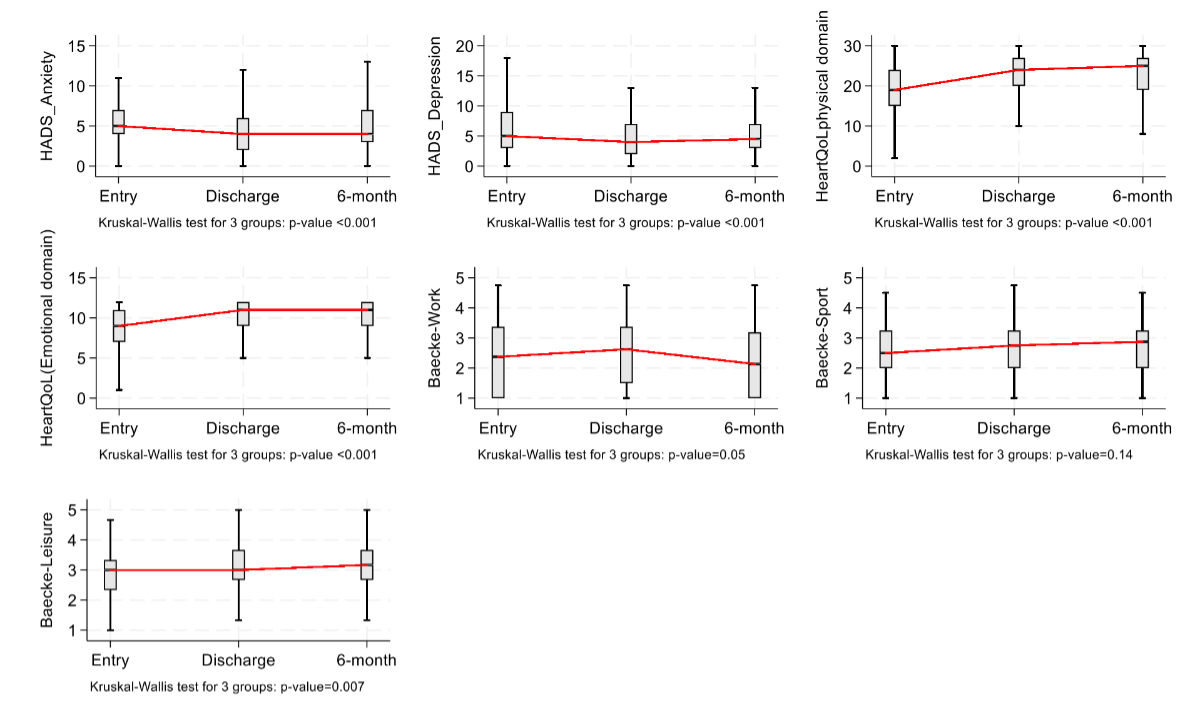
Figure 3Patient-reported outcome measures (PROMs) of depression and anxiety, quality of life and physical activity during the 6-month follow-up. HADS: Hospital Anxiety and Depression Scale; HeartQoL: heart-related quality of life.
The changes in functional capacity and PROMs according to cardiac condition (ACS ± PCI versus others) are presented in appendix tables S1 and S2.
Linear mixed models showed the physical domain of quality of life was associated with 6-minute walk test (coefficient: 1.001, 95% CI: 1.00–1.001) and scores of anxiety (coefficient: 0.97, 95% CI: 0.96–0.99) (table 4). The emotional domain was associated with the depression scores (coefficient: 0.95, 95% CI: 0.94–0.97) and anxiety (coefficient: 0.98, 95% CI: 0.97–0.99) after being adjusted for age, sex and time point (table 4).
Table 4Results of the generalised mixed models regarding the association between different factors with heart-related quality of life (HeartQoL) dimensions. Case-complete analysis was applied for missing data. The coefficients in the model estimate the average change of the response variable for every 1-unit increase in a covariate.
| Physical domain (n = 192) | Emotional domain (n = 192) | |||||||
| expβ | p-value | 95% CI | expβ | p-value | 95% CI | |||
| Age | 1.00 | 0.30 | 1.00 | 1.01 | 1.00 | 0.52 | 1.00 | 1.00 |
| Sex | 0.97 | 0.67 | 0.86 | 1.10 | 1.06 | 0.23 | 0.97 | 1.16 |
| Smoking status | 1.06 | 0.20 | 0.97 | 1.15 | 0.99 | 0.67 | 0.93 | 1.05 |
| 6-minute walk test | 1.001 | 0.02 | 1.00 | 1.001 | 1.00 | 0.29 | 1.00 | 1.00 |
| Maximal short-term exercise capacity | 1.00 | 0.59 | 1.00 | 1.00 | 1.00 | 0.39 | 1.00 | 1.00 |
| eMETs | 1.01 | 0.13 | 1.00 | 1.01 | 1.00 | 0.68 | 0.99 | 1.01 |
| Quadriceps isometric strength left | 1.00 | 0.63 | 1.00 | 1.01 | 1.00 | 0.94 | 1.00 | 1.00 |
| Quadriceps isometric strength right | 1.00 | 0.94 | 1.00 | 1.00 | 1.00 | 0.45 | 1.00 | 1.00 |
| Depression (HADS) (range: 0–21) | 1.00 | 0.50 | 0.98 | 1.01 | 0.95 | <0.001 | 0.94 | 0.97 |
| Anxiety (HADS) (range: 0–21) | 0.97 | 0.004 | 0.96 | 0.99 | 0.98 | 0.002 | 0.97 | 0.99 |
| Baecke work (range: 1–5) | 0.98 | 0.27 | 0.95 | 1.02 | 1.01 | 0.67 | 0.98 | 1.03 |
| Baecke sport (range: 1–5) | 1.01 | 0.69 | 0.96 | 1.06 | 0.99 | 0.65 | 0.96 | 1.03 |
| Baecke leisure time (range: 1–5) | 1.05 | 0.05 | 1.00 | 1.11 | 1.01 | 0.74 | 0.97 | 1.04 |
| Time point | 1.07 | 0.05 | 1.00 | 1.15 | 1.05 | 0.12 | 0.99 | 1.10 |
CI: confidence interval; eMET: estimated metabolic equivalent of task; HADS: Hospital Anxiety and Depression Scale.
Our cardiac patients exhibited a significant improvement in functional capacity (6-minute walk test, estimated metabolic equivalent of task [eMET], maximal short-term exercise capacity, maximal quadriceps isometric strength) upon discharge after a 10-week cardiac rehabilitation programme, alongside improvements in quality of life, symptoms of depression and anxiety and the level of leisure-time physical activity from entry to 6-month follow-up. These results align with existing evidence, underscoring the benefits of a cardiac rehabilitation programme regarding the outcomes of interest [35, 36]. Moreover, the 6-minute walk test and the levels of depression or anxiety have been found to associate significantly with quality of life.
Our results showed a gain of 60 m in the median scores of 6-minute walk test, comparable to the results of a systematic review of 15 studies [5]. The Minimal Clinically Important Difference (MCID) of the 6-minute walk test distance was established at 25 m after a cardiac rehabilitation programme for patients with coronary artery disease [37]. Therefore, the improvement in the 6-minute walk test after cardiac rehabilitation in our study is clinically meaningful. Similarly, the median scores of eMET increased by 0.9 points from entry to discharge in our study, which exceeds the proposed 0.5-MET improvement of the Canadian Cardiovascular Society [38]. To the best of our knowledge, the MCID for the maximal short-term exercise capacity in cardiac rehabilitation patients has not been proposed. However, for adults with chronic musculoskeletal pain, its threshold was established at 25–55 W [39]. We found an increase of 50 W in the median scores of maximal short-term exercise capacity at discharge, which falls within this range.
The median scores of maximal quadriceps isometric strength also showed improvement after cardiac rehabilitation, with an increase between 3 and 4 Nm (7% to 9% from baseline). The MCID for the maximum quadriceps isometric strength (+5.7 Nm) has been described in patients with chronic obstructive pulmonary disease [40]. The quadriceps strength is known to be a predictor of walking performance, exercise capacity [41] and cardiovascular mortality in patients with coronary artery disease [42]. Accordingly, each 10% increase in body weight-adjusted maximal quadriceps isometric strength is associated with reductions of 23% and 34% in the risk of all-cause and cardiovascular mortality, respectively. The observed gains in walking and exercise performance (clinical significance) together with muscle strength could lead to increased independent mobility and more favourable outcomes in our patients. Previous studies showed that every 10 m increase in 6-minute walk test is associated with a 4% reduction in mortality [43], and each 1-MET increase is associated with a 19% lower cardiovascular mortality risk among patients with cardiovascular diseases [44].
The PROMs were also improved from entry to discharge and from entry to the 6-month follow-up. The median depression and anxiety scores decreased significantly during follow-up (between −0.5 and −1 point from entry) but lower than the proposed MCID of 1.7 points [45]. These results can be expected because the participants have a low Hospital Anxiety and Depression Scale (HADS) score at baseline. In addition to psychological improvement, leisure-time physical activity increased and remained elevated at 6 months. A previous meta-analysis of 40 randomised controlled trials showed moderate evidence of increased physical activity after cardiac rehabilitation participation compared with controls [11]. Changes in scores for the work and sport physical activity were not statistically significant during follow-up, probably because our participants were too old (median age of 63 years) to return to work. The median scores of quality of life improved from entry to 6 months after discharge, with a greater difference in the physical domain (+6 points) than in the emotional domain (+2 points). These results are consistent with a previous literature review demonstrating improved quality of life after cardiac rehabilitation in patients with coronary heart disease [8, 46]. There is some evidence that the positive effects of cardiac rehabilitation on physical activity might decrease at longer follow-up [47]. Therefore, ongoing encouragement of a healthy lifestyle and sustained physical activity beyond the initial period of cardiac rehabilitation is necessary.
Factors associated with the heart-related quality of life were the 6-minute walk test and the levels of depression and anxiety. Our findings confirm the results of previous studies that demonstrated functional capacity and psychological distress as predictors of quality of life [14–16]. The association coefficients of some predictors were weak or moderate, for example, the 6-minute walk test (coefficient: 1.001) or symptoms of anxiety (coefficient: 0.97) or depression (coefficient: 0.95). Therefore, there may have been other potential factors influencing heart-related quality of life (such as comorbidities, quality of sleep, social background, etc.) that warrant examination in future studies.
The rate of participation in our cardiac rehabilitation programme was very high (99%). The interval between the acute hospitalisation and rehabilitation phase was also short (1.4 months). In the literature, the overall participation rate in cardiac rehabilitation programmes by patients with acute myocardial infarction is low (34%) [48]. Inadequate referral or geographic variation by hospital referral might be barriers to participation in a cardiac rehabilitation programme [49]. A high rate of participation in our study might be explained by the geographic convenience, the effectiveness of the liaison between the hospital and rehabilitation centres and information on the cardiac rehabilitation programme. Another study showed that cardiac rehabilitation participation rates were associated with insurance status [50]. All Swiss residents are covered under a mandatory universal basic health insurance that includes outpatient and inpatient treatments in a fee-for-service system [51]. The health insurer’s basic insurance pays for in- or outpatient rehabilitation programmes.
Women accounted for 19% of the studied population. Previous studies conducted in the Netherlands, in Italy and in Taiwan also noted a low percentage of women (28%, 27% and 23%, respectively) in cardiac rehabilitation [52–54]. Many reasons for low participation in cardiac rehabilitation by women have been described including lack of insurance or information, transportation issues, long distance, lack of support, comorbidities, older age and obesity [55]. Future studies aiming to increase the participation of women in cardiac rehabilitation programme are needed.
This study has several limitations. It was conducted at a single clinic which might induce population bias. For instance, most participants were men (81%), with a median age of 63 years which limits the generalisability of the results to other populations. There was also a fraction of missing data from the self-reported questionnaires, despite a second reminder to participants to return their responses. The missing data might potentially lead to attrition bias. Data on functional capacity at 6 months are unavailable, so we are unable to determine its progression over time. Another limitation is the absence of a randomised control group which means the improvement of outcomes may have been influenced by the natural course of recovery.
The strength of our study lies in the use of both objective and patient-reported measures to assess outcomes. The functional measurements (6-minute walk test, maximal short-term exercise capacity, eMET, quadriceps isometric strength) were performed using standardised procedures and validated instruments to minimise the measurement bias. PROMs (psychosocial aspect and physical activity) were assessed at different time points. Additionally, we used multilevel mixed-effects generalised linear models to assess the predictors of HeartQol, adjusting for age, sex and time points. This approach enhances statistical power and provides a basis for predictive modelling.
Functional capacity measures including the 6-minute walk test, maximal short-term exercise capacity, eMET and muscle strength increased significantly at discharge from cardiac rehabilitation. Improvements in the 6-minute walk test and eMET were considered clinically meaningful. The level of depression and anxiety, quality of life and leisure-time activity showed significant improvement from entry to discharge and from entry to 6 months. The 6-minute walk test, and the symptoms of depression or anxiety were found to be significantly associated with quality of life. A cardiac rehabilitation programme could be proposed to eligible cardiac patients to improve their outcomes.
The database was registered on Mendeley Data. Analytical codes will be made available on request.
We would like to thank the whole cardiac rehabilitation team (CRR and CHVR) for their support in data collection.
This study received no funding.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Maladies cardiovasculaires. Office fédéral de la statistique. Available on: https://www.bfs.admin.ch/bfs/fr/home/statistiques/sante/etat-sante/maladies/cardiovasculaires.html
2. Anderson L, Oldridge N, Thompson DR, Zwisler AD, Rees K, Martin N, et al. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease: Cochrane Systematic Review and Meta-Analysis. J Am Coll Cardiol. 2016 Jan;67(1):1–12.
3. Arena R, Myers J, Williams MA, Gulati M, Kligfield P, Balady GJ, et al.; American Heart Association Committee on Exercise, Rehabilitation, and Prevention of the Council on Clinical Cardiology; American Heart Association Council on Cardiovascular Nursing. Assessment of functional capacity in clinical and research settings: a scientific statement from the American Heart Association Committee on Exercise, Rehabilitation, and Prevention of the Council on Clinical Cardiology and the Council on Cardiovascular Nursing. Circulation. 2007 Jul;116(3):329–43. doi: https://doi.org/10.1161/CIRCULATIONAHA.106.184461
4. Piepoli MF, Spoletini I, Rosano G. Monitoring functional capacity in heart failure. Eur Heart J Suppl. 2019 Dec;21 Suppl M:M9–12.
5. Bellet RN, Adams L, Morris NR. The 6-minute walk test in outpatient cardiac rehabilitation: validity, reliability and responsiveness—a systematic review. Physiotherapy. 2012 Dec;98(4):277–86.
6. Keteyian SJ, Kerrigan DJ, Lewis B, Ehrman JK, Brawner CA. Exercise training workloads in cardiac rehabilitation are associated with clinical outcomes in patients with heart failure. Am Heart J. 2018 Oct;204:76–82.
7. Phyo AZ, Freak-Poli R, Craig H, Gasevic D, Stocks NP, Gonzalez-Chica DA, et al. Quality of life and mortality in the general population: a systematic review and meta-analysis. BMC Public Health. 2020 Nov;20(1):1596.
8. Shepherd CW, While AE. Cardiac rehabilitation and quality of life: a systematic review. Int J Nurs Stud. 2012 Jun;49(6):755–71.
9. Annapureddy A, Valero-Elizondo J, Khera R, Grandhi GR, Spatz ES, Dreyer RP, et al. Association Between Financial Burden, Quality of Life, and Mental Health Among Those With Atherosclerotic Cardiovascular Disease in the United States. Circ Cardiovasc Qual Outcomes. 2018 Nov;11(11):e005180.
10. Reavell J, Hopkinson M, Clarkesmith D, Lane DA. Effectiveness of Cognitive Behavioral Therapy for Depression and Anxiety in Patients With Cardiovascular Disease: A Systematic Review and Meta-Analysis. Psychosom Med. 2018 Oct;80(8):742–53. doi: https://doi.org/10.1097/PSY.0000000000000626
11. Dibben GO, Dalal HM, Taylor RS, Doherty P, Tang LH, Hillsdon M. Cardiac rehabilitation and physical activity: systematic review and meta-analysis. Heart. 2018 Sep;104(17):1394–402.
12. Hurdus B, Munyombwe T, Dondo TB, Aktaa S, Oliver G, Hall M, et al. Association of cardiac rehabilitation and health-related quality of life following acute myocardial infarction. Heart. 2020 Nov;106(22):1726–31.
13. Jamieson M, Wilcox S, Webster W, Blackhurst D, Valois RF, Durstine JL. Factors influencing health-related quality of life in cardiac rehabilitation patients. Prog Cardiovasc Nurs. 2002;17(3):124-31, 54. https://doi.org/
14. Kažukauskienė N, Burkauskas J, Macijauskienė J, Mickuvienė N, Brožaitienė J. Stressful Life Events Are Associated With Health-Related Quality of Life During Cardiac Rehabilitation and at 2-yr Follow-up in Patients With Heart Failure. J Cardiopulm Rehabil Prev. 2019 Mar;39(2):E5–8. doi: https://doi.org/10.1097/HCR.0000000000000385
15. Staniute M, Bunevicius A, Brozaitiene J, Bunevicius R. Relationship of health-related quality of life with fatigue and exercise capacity in patients with coronary artery disease. Eur J Cardiovasc Nurs. 2014 Aug;13(4):338–44.
16. Strong PC, Lee SH, Chou YC, Wu MJ, Hung SY, Chou CL. Relationship between quality of life and aerobic capacity of patients entering phase II cardiac rehabilitation after coronary artery bypass graft surgery. J Chin Med Assoc. 2012 Mar;75(3):121–6.
17. Abreu A, Pesah E, Supervia M, Turk-Adawi K, Bjarnason-Wehrens B, Lopez-Jimenez F, et al. Cardiac rehabilitation availability and delivery in Europe: How does it differ by region and compare with other high-income countries?: Endorsed by the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2019 Jul;26(11):1131–46.
18. Steinacker JM, Liu Y, Muche R, Koenig W, Hahmann H, Imhof A, et al. Long term effects of comprehensive cardiac rehabilitation in an inpatient and outpatient setting. Swiss Med Wkly. 2011 Jan;141(102):w13141.
19. SCPRS – Directives de la qualité. Available at: https://www.scprs.ch/public/stateoftheart/stateoftheart_francais.html
20. Tessitore E, Schmid JP, Hermann M, Schmied C, Wilhelm M, Meyer P; Working Group for Cardiovascular Prevention, Rehabilitation and Sports Cardiology (SCPRS). Cardiovascular Rehabilitation Delivery and Outcomes in Switzerland in More Than a Hundred Thousand Patients Over the Last Decade. J Cardiopulm Rehabil Prev. 2023 Jul;43(4):305–7. doi: https://doi.org/10.1097/HCR.0000000000000776
21. American Thoracic Society American Thoracic Society guidelines for oxygen based on 6-minute walk. 2002. https://www.atsjournals.org/doi/full/10.1164/rccm.202009-3608ST
22. Meyer P, Gayda M, Juneau M, Nigam A. High-intensity aerobic interval exercise in chronic heart failure. Curr Heart Fail Rep. 2013 Jun;10(2):130–8.
23. Fletcher GF, Ades PA, Kligfield P, Arena R, Balady GJ, Bittner VA, et al.; American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Nutrition, Physical Activity and Metabolism, Council on Cardiovascular and Stroke Nursing, and Council on Epidemiology and Prevention. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. 2013 Aug;128(8):873–934.
24. O’Shea SD, Taylor NF, Paratz JD. Measuring muscle strength for people with chronic obstructive pulmonary disease: retest reliability of hand-held dynamometry. Arch Phys Med Rehabil. 2007 Jan;88(1):32–6.
25. De Backer IC, Schep G, Hoogeveen A, Vreugdenhil G, Kester AD, van Breda E. Exercise testing and training in a cancer rehabilitation program: the advantage of the steep ramp test. Arch Phys Med Rehabil. 2007 May;88(5):610–6.
26. Kim WK, Kim DK, Seo KM, Kang SH. Reliability and validity of isometric knee extensor strength test with hand-held dynamometer depending on its fixation: a pilot study. Ann Rehabil Med. 2014 Feb;38(1):84–93.
27. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983 Jun;67(6):361–70.
28. Herrmann C. International experiences with the Hospital Anxiety and Depression Scale—a review of validation data and clinical results. J Psychosom Res. 1997 Jan;42(1):17–41. doi: https://doi.org/10.1016/S0022-3999(96)00216-4
29. Oldridge N, Höfer S, McGee H, Conroy R, Doyle F, Saner H; for the HeartQoL Project Investigators. The HeartQoL: part I. Development of a new core health-related quality of life questionnaire for patients with ischemic heart disease. Eur J Prev Cardiol. 2014 Jan;21(1):90–7.
30. Oldridge N, Höfer S, McGee H, Conroy R, Doyle F, Saner H; for the HeartQoL Project Investigators. The HeartQoL: part II. Validation of a new core health-related quality of life questionnaire for patients with ischemic heart disease. Eur J Prev Cardiol. 2014 Jan;21(1):98–106.
31. De Smedt D, Clays E, Höfer S, Oldridge N, Kotseva K, Maggioni AP, et al.; EUROASPIRE Investigators. Validity and reliability of the HeartQoL questionnaire in a large sample of stable coronary patients: The EUROASPIRE IV Study of the European Society of Cardiology. Eur J Prev Cardiol. 2016 May;23(7):714–21.
32. Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982 Nov;36(5):936–42.
33. Salinas Ruíz J, Montesinos López OA, Hernández Ramírez G, Crossa Hiriart J. Generalized Linear Mixed Models for Non-normal Responses. Generalized Linear Mixed Models with Applications in Agriculture and Biology. Cham: Springer International Publishing; 2023. pp. 113–27.
34. Rickham PP. HUMAN EXPERIMENTATION. CODE OF ETHICS OF WORLD MEDICAL ASSOCIATION. DECLARATION OF HELSINKI. BMJ. 1964 Jul;2(5402):177.
35. Fan Y, Yu M, Li J, Zhang H, Liu Q, Zhao L, et al. Efficacy and Safety of Resistance Training for Coronary Heart Disease Rehabilitation: A Systematic Review of Randomized Controlled Trials. Front Cardiovasc Med. 2021 Nov;8:754794.
36. Lin X, Zhang X, Guo J, Roberts CK, McKenzie S, Wu WC, et al. Effects of Exercise Training on Cardiorespiratory Fitness and Biomarkers of Cardiometabolic Health: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Am Heart Assoc. 2015 Jun;4(7):e002014. doi: https://doi.org/10.1161/JAHA.115.002014
37. Gremeaux V, Troisgros O, Benaïm S, Hannequin A, Laurent Y, Casillas JM, et al. Determining the minimal clinically important difference for the six-minute walk test and the 200-meter fast-walk test during cardiac rehabilitation program in coronary artery disease patients after acute coronary syndrome. Arch Phys Med Rehabil. 2011 Apr;92(4):611–9.
38. Grace SL, Poirier P, Norris CM, Oakes GH, Somanader DS, Suskin N; Canadian Association of Cardiac Rehabilitation. Pan-Canadian development of cardiac rehabilitation and secondary prevention quality indicators. Can J Cardiol. 2014 Aug;30(8):945–8.
39. Benaim C, Blaser S, Léger B, Vuistiner P, Luthi F. “Minimal clinically important difference” estimates of 6 commonly-used performance tests in patients with chronic musculoskeletal pain completing a work-related multidisciplinary rehabilitation program. BMC Musculoskelet Disord. 2019 Jan;20(1):16.
40. Oliveira A, Rebelo P, Paixão C, Jácome C, Cruz J, Martins V, et al. Minimal Clinically Important Difference for Quadriceps Muscle Strength in People with COPD following Pulmonary Rehabilitation. COPD. 2021 Feb;18(1):35–44.
41. Kamiya K, Mezzani A, Hotta K, Shimizu R, Kamekawa D, Noda C, et al. Quadriceps isometric strength as a predictor of exercise capacity in coronary artery disease patients. Eur J Prev Cardiol. 2014 Oct;21(10):1285–91.
42. Kamiya K, Masuda T, Tanaka S, Hamazaki N, Matsue Y, Mezzani A, et al. Quadriceps Strength as a Predictor of Mortality in Coronary Artery Disease. Am J Med. 2015 Nov;128(11):1212–9.
43. Shawon MS, Hsu B, Chard R, Nicholson IA, Elias VL, Nicola LK, et al. Six-minute walk test distance at time of hospital discharge is strongly and independently associated with all-cause mortality following cardiac surgery. Sci Rep. 2024 Jan;14(1):2493.
44. Ezzatvar Y, Izquierdo M, Núñez J, Calatayud J, Ramírez-Vélez R, García-Hermoso A. Cardiorespiratory fitness measured with cardiopulmonary exercise testing and mortality in patients with cardiovascular disease: A systematic review and meta-analysis. J Sport Health Sci. 2021 Dec;10(6):609–19.
45. Lemay KR, Tulloch HE, Pipe AL, Reed JL. Establishing the Minimal Clinically Important Difference for the Hospital Anxiety and Depression Scale in Patients With Cardiovascular Disease. J Cardiopulm Rehabil Prev. 2019 Nov;39(6):E6–11. doi: https://doi.org/10.1097/HCR.0000000000000379
46. Lourens EC, Baker RA, Krieg BM. Quality of life following cardiac rehabilitation in cardiac surgery patients. J Cardiothorac Surg. 2022 May;17(1):137.
47. Meiring RM, Tanimukai K, Bradnam L. The Effect of Exercise-Based Cardiac Rehabilitation on Objectively Measured Physical Activity and Sedentary Behavior: A Systematic Review and Meta-analysis. J Prim Care Community Health. 2020;11:2150132720935290.
48. Wang L, Liu J, Fang H, Wang X. Factors associated with participation in cardiac rehabilitation in patients with acute myocardial infarction: A systematic review and meta-analysis. Clin Cardiol. 2023 Nov;46(11):1450–7.
49. Ritchey MD, Maresh S, McNeely J, Shaffer T, Jackson SL, Keteyian SJ, et al. Tracking Cardiac Rehabilitation Participation and Completion Among Medicare Beneficiaries to Inform the Efforts of a National Initiative. Circ Cardiovasc Qual Outcomes. 2020 Jan;13(1):e005902. doi: https://doi.org/10.1161/CIRCOUTCOMES.119.005902
50. Gallagher R, Neubeck L, Du H, Astley C, Berry NM, Hill MN, et al. Facilitating or getting in the way? The effect of clinicians’ knowledge, values and beliefs on referral and participation. Eur J Prev Cardiol. 2016 Jul;23(11):1141–50.
51. Biller-Andorno N, Zeltner T. Individual Responsibility and Community Solidarity—The Swiss Health Care System. N Engl J Med. 2015 Dec;373(23):2193–7.
52. Lin WC, Ho CH, Tung LC, Ho CC, Chou W, Wang CH. Differences Between Women and Men in Phase I Cardiac Rehabilitation After Acute Myocardial Infarction: A Nationwide Population-Based Analysis. Medicine (Baltimore). 2016 Jan;95(3):e2494. doi: https://doi.org/10.1097/MD.0000000000002494
53. Eijsvogels TMH, Maessen MFH, Bakker EA, Meindersma EP, van Gorp N, Pijnenburg N, et al. Association of Cardiac Rehabilitation With All-Cause Mortality Among Patients With Cardiovascular Disease in the Netherlands. JAMA Network Open. 2020;3(7):e2011686-e. https://doi.org/
54. De Feo S, Tramarin R, Ambrosetti M, Riccio C, Temporelli PL, Favretto G, et al. Gender differences in cardiac rehabilitation programs from the Italian survey on cardiac rehabilitation (ISYDE-2008). Int J Cardiol. 2012 Oct;160(2):133–9.
55. Supervía M, Medina-Inojosa JR, Yeung C, Lopez-Jimenez F, Squires RW, Pérez-Terzic CM, et al. Cardiac Rehabilitation for Women: A Systematic Review of Barriers and Solutions. Mayo Clin Proc. 2017 Mar;92(4):565–77.
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.4160.