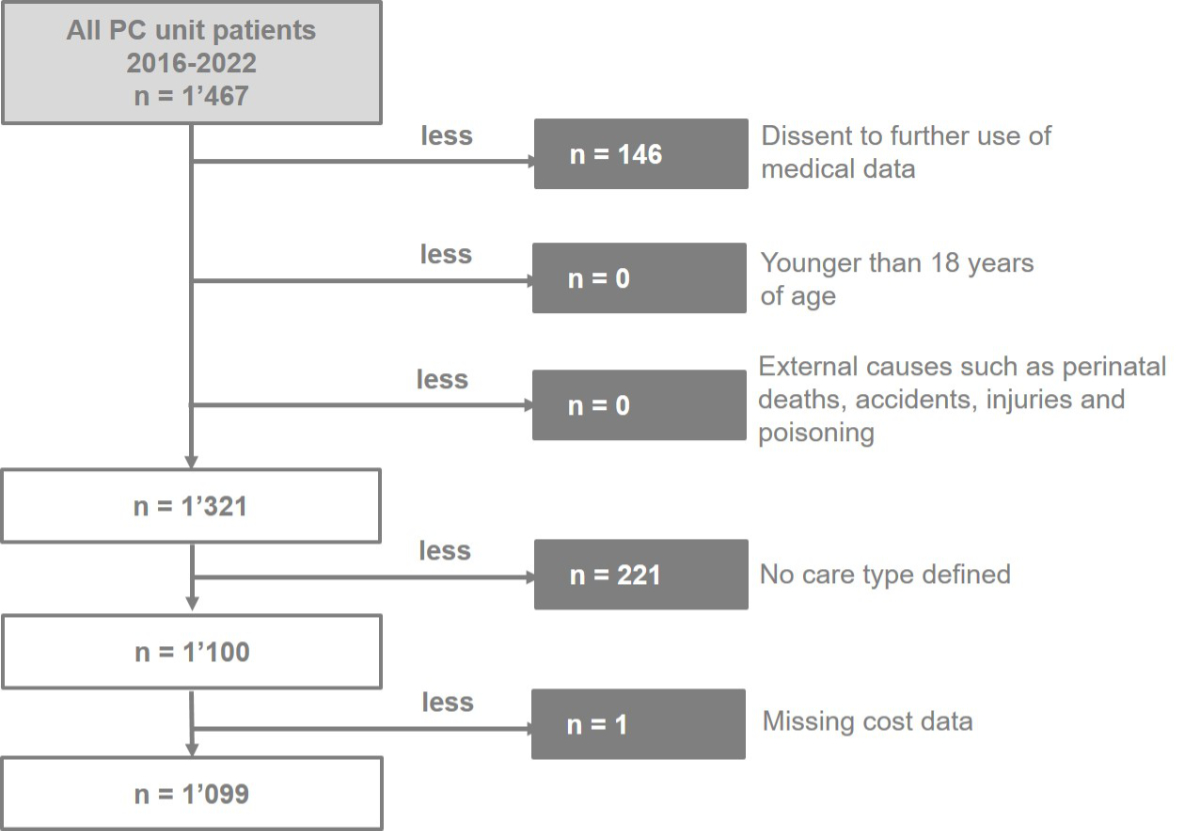
Figure 1Exclusion flowchart for the study population. PC: palliative care.
DOI: https://doi.org/https://doi.org/10.57187/s.4132
Although costs of inpatient palliative care are widely studied [1–14], heterogeneous patient needs in specialist inpatient palliative care continue to challenge health scientists. Patients receiving specialist palliative care are often grouped under a single umbrella, which means uniformly applying costs and related reimbursements across all patients hospitalised in specialist palliative care units. This is the current basis for reimbursement via diagnosis-related groups (DRG). However, patients with diverse clinical needs demonstrate different diagnostic and therapeutic intervention patterns and require an array of interprofessional competencies, leading to various cost clusters during hospitalisations. Emerging evidence suggests that categorising patients receiving palliative care into distinct groups provides more accurate reflections of incurred costs and resources, yet existing data remain limited [5, 15–17]. It is reasonable to assume that patient groups possibly and most likely differ in terms of generated costs.
To address the different sets of competencies required to meet patients’ clinical needs, we categorised patient care into four distinct groups [18]. These care types are derived from clinically defined care goals within a specialist palliative care unit in a Swiss university hospital and were introduced in 2012. Details on the care type framework are presented in the appendix (appendix tables S1 and S2). Our study investigates whether these different care types are associated with different hospital costs. We hypothesised that patients – classified into one of four care types based on their care goals – would differ significantly by costs and their respective cost categories, with care type 1 being the most expensive.
We performed a single-centre, retrospective, observational analysis using the following administrative data for specialist palliative care inpatients: patient characteristics and transfers; records regarding care activities; costs per unit; and medication databases. The study site, at a Swiss university hospital, encompassed a 10-bed acute palliative care unit, an ambulatory consultation service and an inhouse consultation service. The centre offers an interdisciplinary therapeutic approach (e.g. physiotherapy, nutrition counselling, social counselling, psychotherapy) and full access to diagnostic and therapeutic measures (e.g. CT, MRI, chemotherapy, radiotherapy).
Since 2012, administrative data of the specialist palliative care unit of the hospital has contained care type groups. In the first years after introduction of the care types, the quality of administrative data was poor. We therefore used administrative data for the period from 1 January 2016 to 31 December 2022. Patients were included in the study if they provided general consent for their health-related data to be used for research purposes; were aged 18 years or over; and had a minimum stay of one night in the specialist palliative care unit. Patients were excluded from the study population if they refused consent for their health-related data to be used for research purposes; if they died as a result of injury, poisoning or other consequences of external causes (e.g. self-harm, assault) and accidents (with transport vehicles or other), as classified in the ICD-10; if their death was a result of medical or surgical complications when the patient was otherwise healthy; if cost data or care type data were missing (figure 1). Patients in the specialist palliative care unit generally all receive a care type, however this does not account for external patients who did not qualify as patients in need of specialist palliative care. The care type was also missing if physicians sometimes had no time to make a care type evaluation because the patients stayed only shortly at the department. In August 2023, we received data originating from the municipal office regarding the survival status of the patients in our study population.
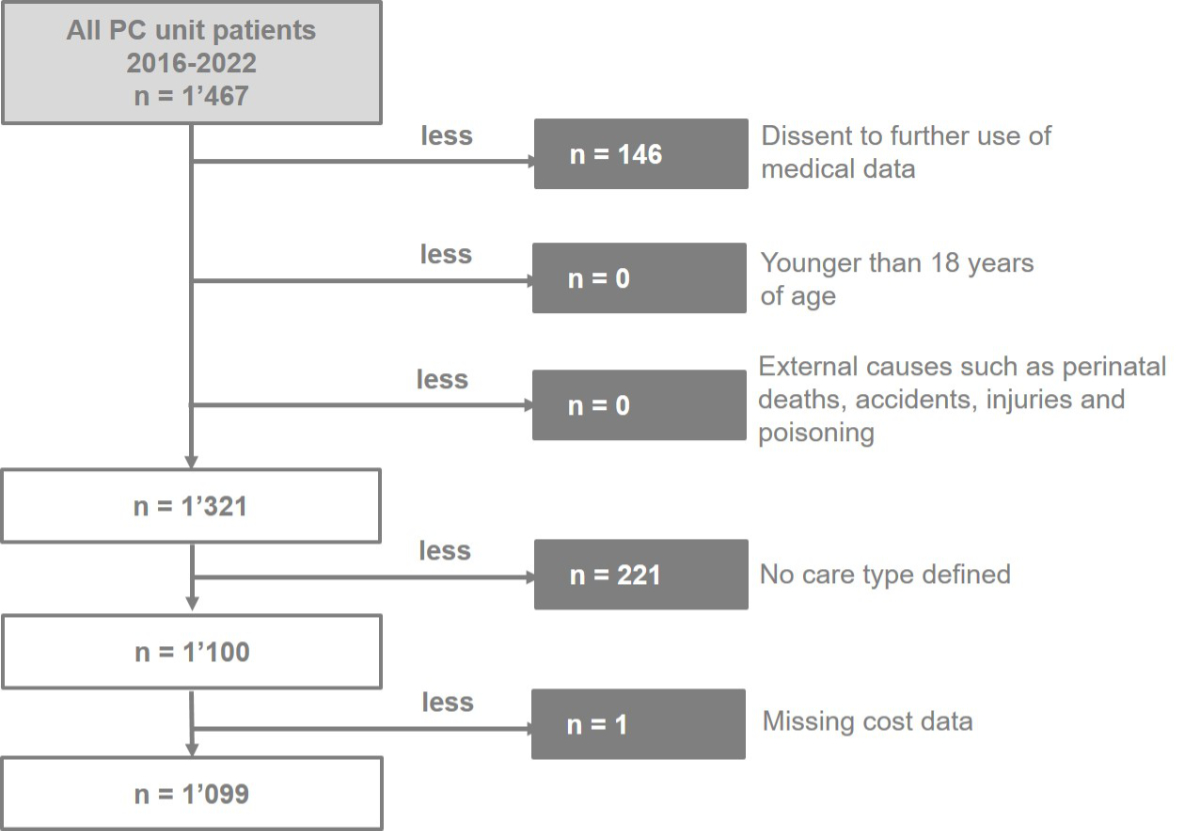
Figure 1Exclusion flowchart for the study population. PC: palliative care.
Specialist palliative care treatment goals vary widely, as patients admitted to a specialist palliative care unit show heterogeneity in main diagnosis, disease complexity, life expectancy, patient and family needs and preferences, and socioeconomic situation. Categorising treatment goals helps interprofessional specialist palliative care teams quickly gain an understanding of a patient’s current treatment goal. The care type framework emerged as a successful practical solution to streamline internal processes and procedures in clinical care and as a result was implemented in the study specialist palliative care unit in 2012. It delineates the most common patient treatment goals in specialist palliative care hospital settings based on clinical practice. In routine clinical care, care type classification serves as a compass for interprofessional specialist palliative care team members and helps to align medical treatment, nursing care, psychological care, social care and physiotherapy. The care type framework was developed in 2007 by two senior palliative care specialists at the Kantonalspital St Gallen. Care types were derived from interprofessional assessments and discussions with patients and their relatives.
The care type framework (figure 2 and appendix tables S1 and S2) addresses dynamic performance stages and clinical competencies.
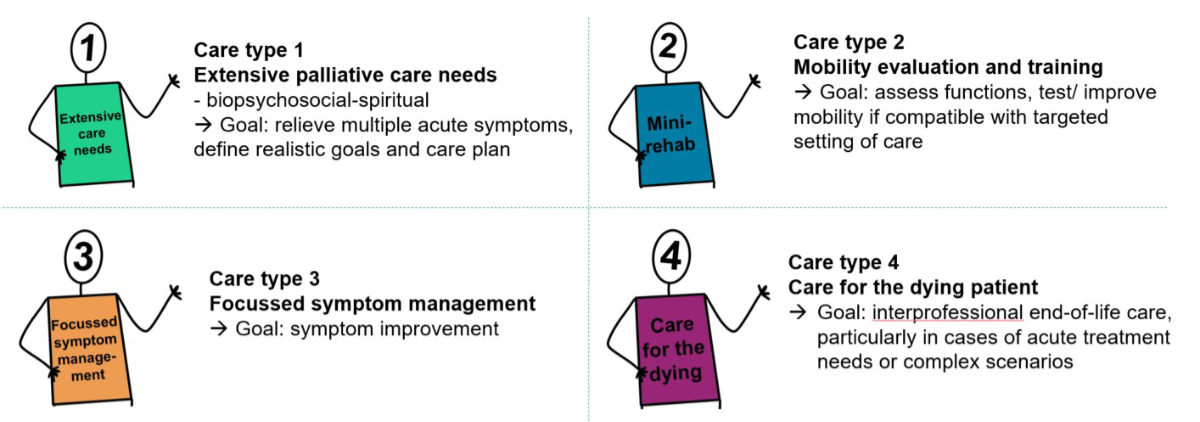
Figure 2The care type framework.
The standard procedure for assigning patients to care type groups is as follows: On the day of admission to the specialist palliative care unit, the treating specialist palliative care physicians and nurses assign patients to care type 1, 2, 3 or 4 unless the patients have already been recently assigned to a care type by specialist palliative care consultation teams on other units or during ambulatory specialist palliative care consultations. The interprofessional team of the specialist palliative care unit reviews patient care type correctness weekly and, if necessary, updates care types. If there is a discrepancy regarding which care type the patient belongs to, round-table discussions are held with the responsible interprofessional team and, whenever possible, with the patient and his/her relatives until an agreement is reached. However, the final decision is made by the treating physician and admitting nurse. We used the last reported care type during patient hospitalisation in our analyses. This was for reasons of simplicity and as the length of stay at the specialist palliative care per hospitalisation is known to be relatively short, we did not expect high fluctuations between care type groups.
We used administrative cost data recorded in hospital patient and financial systems by hospital staff. Since information at the smallest unit level was available – such as pills, minutes, and treatment units and exact dates – we exclusively incorporated costs into our dataset from the days patients were referred to specialist palliative care until discharge from the specialist palliative care unit, whether discharged alive or upon death. Our cost assessment was performed from the perspective of the healthcare provider, including direct costs paid by the healthcare provider. Costs reflect the actual unadjusted expenses the hospital incurred to provide the services. We included all expenses of the hospital and did not make any selection of care costs. All costs are reported in Swiss Francs (CHF).
Reflecting all hospital areas, we categorised cost data into seven different cost categories as follow [4]:
Public health insurance is mandatory for all residents of Switzerland. The mandatory basic standardised insurance package includes all necessary medical and pregnancy-related benefits, such as ambulatory and in-patient care, medications and medical aids, which are considered appropriate in terms of both medical necessity and cost. Additional benefits can be added to the basic insurance by purchasing voluntary, private or semi-private insurance, which allows for more provider and treatment options (such as complementary medicine and dental care) and includes perks like a private hospital room [19]. Hospitals are reimbursed for their services by health insurance, governmental financing and patient out-of-pocket payments.
We present continuous and categorical patient characteristics with median and quartiles (Q1, Q3) and frequencies. We compared care type groups using Kruskal-Wallis tests for continuous variables and chi-squared tests for categorical variables.
We present unadjusted cost data with median and quartiles (Q1, Q3) for each group and compared between care types using Kruskal-Wallis tests.
We hypothesise that the treatment goals that are categorised in care types drive hospital costs.
As we cannot exclude an influence of patient characteristics on the association between the different care types and costs, analyses were adjusted for patient characteristics using inverse probability of treatment weighting (IPTW), with weights generated using the propensity score method. Propensity scores were derived by a multinomial logistic regression with age, sex, marital status, insurance class, type of illness, location prior to specialist palliative care unit and case mix index as covariates. Levels of covariates with few entries were collapsed: marital status (as a binary variable, yes/no), type of illness (cancer, yes/no) and location prior to specialist palliative care (all hospital units). Table 1 shows the uncollapsed categories for marital status, insurance class, main diagnosis and location prior to specialist palliative care unit. For the two continuous variables age and case mix index, a flexible parameterisation was used. A multivariable fractional polynomial (MFP) model for best predicting the care type variable was selected automatically and used in the logistic regression to build the weights. This method preserves the continuous nature of the covariates in a regression model even if the relationships may be non-linear. The method by Stürmer et al. was used to trim the weights based on the 1st and 99th percentiles [20].
Table 1Baseline characteristics of patients with palliative care admitted to the specialist palliative care unit between 1 January 2016 and 31 December 2022.
| Overall (n = 1099) | Care type 1 (n = 484) | Care type 2 (n = 100) | Care type 3(n = 262) | Care type 4 (n = 253) | p-value | ||
| Age at admission (yrs) | Median [Q1–Q3] | 67 [57–75] | 66 [57–74] | 70 [59–76] | 66 [56–74] | 68 [59–75] | 0.21 |
| Sex – n (%) | 0.09 | ||||||
| Male | 643 (59%) | 295 (61%) | 58 (58%) | 136 (52%) | 154 (61%) | ||
| Female | 456 (41%) | 189 (39%) | 42 (42%) | 126 (48%) | 99 (39%) | ||
| Marital status – n (%) | 0.45 | ||||||
| Single | 153 (14%) | 77 (16%) | 10 (10%) | 37 (14%) | 29 (11%) | ||
| Married | 632 (58%) | 271 (56%) | 60 (60%) | 144 (55%) | 157 (62%) | ||
| Widowed | 18 (1.6%) | 6 (1.2%) | 1 (1%) | 7 (2.7%) | 4 (1.6%) | ||
| Divorced | 106 (10%) | 41 (8.5%) | 12 (12%) | 26 (10%) | 27 (11%) | ||
| Separated | 186 (17%) | 88 (18%) | 16 (16%) | 47 (18%) | 35 (14%) | ||
| Unknown | 4 (0.4%) | 1 (0.2%) | 1 (1%) | 1 (0.4%) | 1 (0.4%) | ||
| Insurance class – n (%) | 0.39 | ||||||
| Public | 847 (77%) | 371 (77%) | 76 (76%) | 209 (80%) | 191 (75%) | ||
| Semi-private | 208 (19%) | 90 (19%) | 21 (21%) | 41 (16%) | 56 (22%) | ||
| Private | 44 (4.0%) | 23 (4.8%) | 3 (3.0%) | 12 (4.6%) | 6 (2.4%) | ||
| Main diagnosis – n (%) | 0.04 | ||||||
| Cardiovascular diseases | 29 (2.6%) | 8 (1.7%) | 4 (4.0%) | 5 (1.9%) | 12 (4.7%) | ||
| Endocrine, nutritional and metabolic diseases | 3 (0.3%) | 1 (0.2%) | 0 (0%) | 0 (0%) | 2 (0.8%) | ||
| Gastrointestinal diseases | 5 (0.5%) | 1 (0.2%) | 0 (0%) | 0 (0%) | 4 (1.6%) | ||
| Infectious diseases | 7 (0.6%) | 4 (0.8%) | 0 (0%) | 0 (0%) | 3 (1.2%) | ||
| Malignant neoplasms | 989 (90%) | 441 (91%) | 86 (86%) | 241 (92%) | 221 (87%) | ||
| Neurological diseases | 32 (2.9%) | 14 (2.9%) | 6 (6.0%) | 7 (2.7%) | 5 (2.0%) | ||
| Other | 34 (3.1%) | 15 (3.1%) | 4 (4.0%) | 9 (3.4%) | 6 (2.4%) | ||
| Location of patient prior to specialist palliative care unit – n (%) | <0.001 | ||||||
| Emergency department | 280 (25%) | 130 (27%) | 26 (26%) | 42 (16%) | 82 (32%) | ||
| Home (directly to specialist palliative care unit) | 425 (39%) | 173 (36%) | 36 (36%) | 155 (59%) | 61 (24%) | ||
| Other hospital units | 394 (36%) | 181 (37%) | 38 (38%) | 65 (25%) | 110 (43%) | ||
| Survival status* (8 August 2023) – n (%) | <0.001 | ||||||
| Alive | 58 (5.3%) | 21 (4.3%) | 11 (11%) | 25 (10%) | 1 (0.4%) | ||
| Died after leaving hospital | 638 (58%) | 329 (68%) | 86 (86%) | 189 (72%) | 34 (13%) | ||
| Died at hospital | 403 (37%) | 134 (28%) | 3 (3.0%) | 48 (18%) | 218 (86%) | ||
| Case mix index** | Median [Q1–Q3] | 2.2 [1.4–3.6] | 2.3 [1.5–4.0] | 2.5 [1.5–4.2] | 1.8 [1.4–2.4] | 1.6 [1.3–3.2] | <0.001 |
| Length of stay in specialist palliative care unit (days) | Median [Q1–Q3] | 12 [7.0–16] | 13 [8.0–18] | 14 [9.0–17] | 12 [7.0–15] | 8.0 [3.0–13] | <0.001 |
* Survival status: denotes whether a patient is alive or deceased at a specific point in time (in our analysis the point in time is 8 August 2023).
** Case mix index: a measure of the type, complexity and severity of the patient group. Higher values indicate that a hospital has treated a greater number of complex, resource-intensive patients [23, 38].
Propensity score and treatment effect estimation were done in two steps. First, a logistic regression was carried out to compute the weights and the stabilised weights. Second, the generalised linear model with an assumed gamma distribution of errors and a logarithmic link function, adjusted by inverse probability weighting using stabilised weights, was estimated. We calculated potential outcome means and average treatment effects based on the weighted generalised linear regression [21].
On this basis, the total costs of the four care types were compared. The potential outcome means represent the theoretical means if all patients received the specific care type. As average treatment effects, mean ratios of the costs of different care types were calculated for all patients. Point estimates are accompanied by bias-corrected 95% bootstrap confidence intervals (95% CI). Due to the exploratory purpose of the analysis, p-values were not corrected for multiple testing. We performed sensitivity analyses of the adjusted costs, excluding patients found to have a relatively long survival in the main analysis. “Relatively long survival” was defined as not deceased during hospitalisation or within 31 weeks of the study end. The underlying notion was that these patients with a relatively long survival time may have been different in terms of disease severity and care needs. We performed all analyses using Stata 18 (Stata Corporation, College Station, Texas, USA).
Of 1099 included patients, 484 (44%) were assigned to care type 1; 100 (9%) care type 2; 262 (24%) care type 3; and 253 (23%) care type 4. We provide baseline patient characteristics in table 1. No missing data were identified in the included patient sample. Results showed clear differences between care type groups in the main diagnosis (p = 0.04); location of patient before referral to the specialist palliative care unit (p <0.001); survival status (p <0.001); case mix (p <0.001); and length of stay on specialist palliative care unit (p <0.001).
Our analyses of changes in care type during one hospitalisation showed 4.5% patients (n = 50) with one care type change – most often from care type 1 to care type 3 (2%; n = 23) – and no patients with two or more care type changes. All patients initially with care type 4 had no change in their care type. Two patients changed from care type 3 to care type 4 for all analysed years.
Overall unadjusted median costs per patient were CHF 20,253 (interquartile range [IQR] 12,327–30,104). Analyses showed a clear difference between care type groups for overall costs (p <0.001) and for all cost categories (p <0.001). Median overall unadjusted costs per patient were CHF 23,999 for care type 1; CHF 21,598 for care type 2; CHF 17,946 for care type 3; and CHF 14,997 for care type 4 (appendix table S3). In all care type groups, nursing costs were the biggest cost category. Overall unadjusted costs show a decrease in costs from care type 1 to 2 to 3 to 4.
After adjustment for patient characteristics, care type groups showed clearly different overall costs (figure 3). Adjusted potential overall mean costs were lowest for care type 4 and different (–15%) from the most expensive care type 1 (p = 0.009).
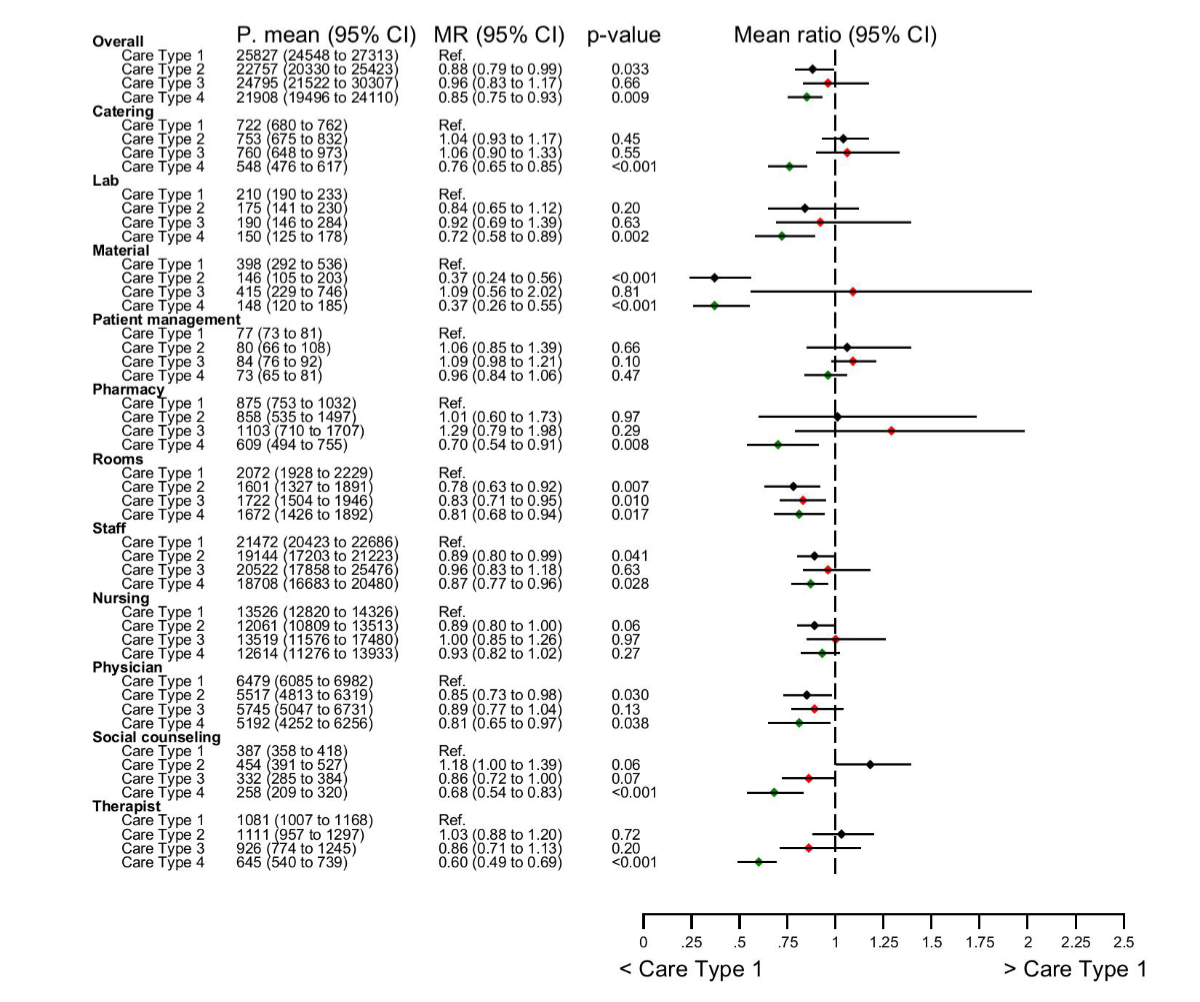
Figure 3Adjusted overall potential mean hospital costs by care type and cost category using propensity score model (average treatment effect total): Treatment effects show the ratio of the potential means (MR) of overall hospital costs of specialist palliative care (sPC) in CHF between patients with care type 2, 3 and 4 compared to patients with care type 1 (ref.), adjusted for age, sex, marital status, insurance class, type of illness, location prior to specialist palliative care unit and case mix index. A potential mean of care type refers to a theoretical mean if all patients received a given, specific care type.A treatment ratio <1 indicates a decrease in the potential mean of cost compared to care type 1 and a treatment ratio >1 indicates an increase in cost compared to care type 1. MR: Mean ratio; PM: potential outcome mean; Ref: reference care type.
In the analyses of adjusted cost categories, care type 4 showed 24% lower catering costs (p <0.001); 28% lower laboratory costs (p = 0.002), 63% lower materials costs (p <0.001), 32% lower social counselling costs (p <0.001), 40% lower therapist costs (p <0.001) when compared with care type 1. Care type 2 showed 63% lower materials costs (p <0.001) than care type 1.
Unadjusted median costs per day per patient were CHF 1815 (IQR 1562–2198). Unadjusted median costs per day per care type were: CHF 1824 for care type 1; CHF 1685 for care type 2; CHF 1721 for care type 3; and CHF 1924 for care type 4 (appendix table S4). Unadjusted differences by cost category are also shown in appendix table S4. Overall unadjusted median nursing costs per day accounted for 54% of daily hospital costs. For all care types, unadjusted median nursing costs were the biggest cost category and materials and patient management costs were the smallest.
Using the generalised linear model, care type groups showed clearly different potential daily mean costs (figure 4). Adjusted potential overall mean costs per day for care type 2 were clearly lower (11%) than for care type 1 (p <0.001). Adjusted overall mean costs per day for care type 4 were the highest of all care types (+21%) compared to care type 1 (p = 0.12), which was driven by nursing and physician costs. Adjusted daily catering (p <0.001), social counselling (p <0.001) and therapy (p <0.001) costs were lowest for care type 4.
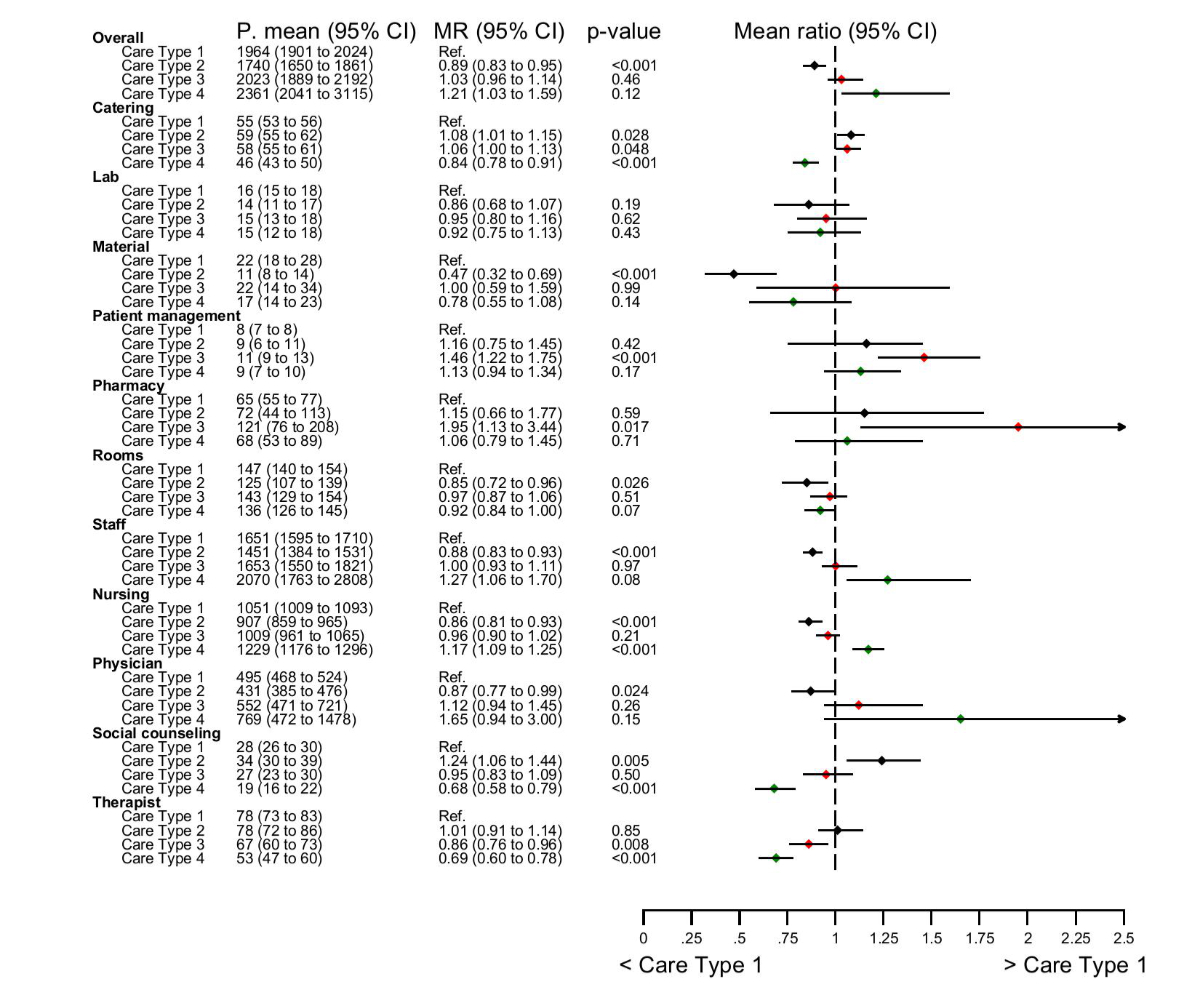
Figure 4Adjusted potential mean hospital costs per day by care type and cost category using propensity score model (average treatment effect per day): Treatment effects show the ratio of the potential means (MR) of daily hospital costs of specialist palliative care (sPC) in CHF between patients with care type 2, 3 and 4 compared to patients with care type 1 (ref.), adjusted for age, sex, marital status, insurance class, type of illness, location prior to specialist palliative care unit and case mix index. A potential mean of care type refers to the theoretical means if all patients received a given, specific care type. A treatment ratio <1 indicates a decrease of the potential mean of cost compared to care type 1 and a treatment ratio >1 indicates an increase in cost compared to care type 1. MR: Mean ratio; PM: potential outcome mean; Ref: reference care type.
Lowest adjusted mean staff costs per day appeared in care type 2. Care type 2 also showed the lowest adjusted costs per day in material and rooms. Daily pharmacy adjusted mean costs were lowest for care type 1 and highest for care type 3.
Results from adjusted overall and daily costs remained similar when we excluded patients who were alive after 31 weeks after the last patients discharged on 31 December 2022 (tables S5 and S6 in the appendix).
The care type framework for specialist palliative care evolved from two clinical needs: defining treatment goals specific to inpatient specialist palliative care and redirecting necessary interprofessional competencies in a usually very short time period. To our knowledge, no other system or framework exists for such a purpose. While the main purpose of the framework is to address a medical necessity, a valuable additional benefit is that it can also serve as a factor in cost analysis. This study showed the framework’s potential to predict various cost clusters in this usually very heterogeneous patient population.
Already in 1998 in Australia, efforts to complete the diagnosis-related group (DRG) system involved integrating treatment goals to adequately describe costs for different care situations. Lee et al. [22] could show that costs of subacute care, like palliative care, are not adequately described by the existing case mix classifications [23]. In a following study [15, 24], they integrated five phases of care (stable, unstable, deteriorating, terminal and bereavement) to describe the actual situations of patients, including their family members and caregivers. They found that the phase of care, the functional status, age and severity of symptoms were good predictors of costs in Australian palliative care, better than the patient’s underlying diagnosis [24, 25]. The findings of the Australian Palliative Care Outcomes Collaboration (PCOC) [26] have influenced subsequent studies in other countries, which have investigated patient-related costs and contributing factors [2, 5, 12, 16, 17, 27]. For example, a German study by Becker et al. [5] identified that the phase of illness, Karnofsky performance score and type of discharge are key factors driving palliative care costs. A Brazilian study found that the place of death had the greatest impact on the cost per day, with deaths in hospitals and hospice care increasing the average cost per day by 1.56 and 1.83, respectively [12]. These international findings collectively enhance our understanding of resource needs and associated costs in palliative care.
Despite the absence of an internationally standardised procedure, the assessment process for grouping palliative care patients remains intricate and time-consuming. For economic evaluations that utilise various cost categories aligned with different care goals and needs, the care type framework presents a promising option because it originates from a clear clinical purpose of patient-orientated goal-directed care. This potential led us to select it for our retrospective analysis. The care type framework offers the prospect of quickly and easily categorising patients.
The results of our comprehensive analysis provide a detailed breakdown of individual cost categories, revealing why some palliative care patients have higher expenses than others. Our study not only differentiates between the daily and overall costs of palliative care patients but also distinguishes the costs among different palliative care patient groups.
Patients categorised as care type 4 displayed the lowest overall costs per stay, whereas care type 1 patients had the highest overall costs mainly because of high-intensity care over a longer period (length of stay: 13 days vs 8 days). Our initial hypothesis was that patients classified as care type 1 – characterised by extensive care needs – would incur the highest costs from complex care requirements. However, we only confirmed our initial hypothesis for overall costs. In fact patients classified as care type 4 (care for dying patients) showed the highest daily costs driven by staff costs – especially nursing – that patients in the dying phase generate mainly through increased communication with them and their relatives [1, 2, 12, 14]. The significant impact of length of stay on costs was also evident in other studies [4, 8, 17, 28–30]. Our findings emphasise the necessity for more personalised approaches to managing inpatient specialist palliative care. For example, considering other facilities – with lower operating costs and similarly high quality of care – is a worthwhile option to explore. We also conclude that care for a dying person at a university hospital palliative care unit can be very demanding necessitating a very broad range of competencies, a situation not reflected in the DRG-based reimbursement system.
Costs – overall and daily – mostly comprised staff costs, which was also shown in other studies [2, 4, 31]. Some studies focused on family caregiving costs for home-based palliative care with similar results [32, 33]. Given the palliative care emphasis on interpersonal relationships and care, we recognise concordance with the essence of palliative care in high staff costs (especially nursing costs) across all care types. The highest costs for social work were associated with care type 2. Patients with care type 2 typically seek to improve their mobility and are often unable to return to their familiar living environments without additional aids.
Other cost categories, such as catering costs, were the lowest for care type 4, which can be explained by the general condition of dying patients, who often have anorexia [34]. Care type 1 patients correspond most to “usual medical care” with high overall costs for diagnostic and pharmacological interventions. This also explains the highest room costs per day for care type 1 patient with extensive palliative care needs.
Our study analysed a large database – with a detailed dataset – over seven years. Notably, we directly derived the costs we analysed from the hospital database; thus, we minimised potential biases in our study data since no insurance data or tariff data were included, resulting in a more accurate reflection of real costs. However, we acknowledge some important limitations of our study. Admittedly, it is uncommon for an economic evaluation to use an unpublished, unevaluated clinical framework. However, we implemented our care type framework in clinical practice more than ten years ago. Although the care type framework remains untested in other hospital settings, team members reported experiencing the framework as easy to use and helpful for organising interprofessional care. Expanding the framework to other hospitals could validate its generalisability. Second, we derived data from only one university hospital in a retrospective, observational manner. From a statistical standpoint, while propensity score weighting was employed to adjust for the impact of patient characteristics, its ability to account for unmeasured variables is limited. Third, we only accounted for a restricted set of confounding factors. Nonetheless, we made efforts to ensure a robust comparison between care types using all available data at the time of hospital admission. Furthermore, we were unable to analyse the specific tasks of the staff. For example, we suspect that the high care costs of care type 4 are associated with increased communication with relatives; therefore, expanding care for relatives may have meant slower handling of patient daily personal care. For other studies, staff costs were also unspecified by task, instead reporting personnel costs, staff costs or caregiving costs [2, 32, 33] as the biggest cost components. Yen et al. reported nurses spent most of their time communicating with patients [35].
We recommend that future studies investigate the balance between patient needs for care type 4 and the level of care specialisation in a specialist palliative care unit. Future studies may examine frameworks to better match care needs with various levels and intensity of care competencies, with the aim of allocating highly qualified healthcare personnel as efficiently as possible to avoid staff shortages, and reduce costs. Additionally, specialist palliative care in home-like environments may align more closely with patient wishes than in-hospital specialist palliative care. For example, 72% of people in Switzerland prefer dying at home [36, 37], with similar figures in other countries [38].
Incorporating care type classifications in other hospitals and thus, in future studies, could validate its generalisability and enhance cost projections and facilitate the development of cost-effective care models. It can also raise awareness among stakeholders in the healthcare system of the importance of high-quality post-hospital facilities such as hospices, nursing homes or any other long-term care facilities. These classifications might also improve reimbursement systems, by more accurately representing the distinct nature of specialist palliative care compared to curative disciplines. This is particularly crucial for the DRG system, which primarily considers length of stay for reimbursement but often overlooks the intensity and complexity of interprofessional care. From a clinical perspective, the care type classification can act as a guiding framework for interprofessional specialist palliative care team members, enhancing internal processes and coordination.
There is clear evidence of differences between patients in specialist palliative care units in terms of overall and detailed hospitalisation costs. Length of stay and staff costs, especially nursing costs, appear important drivers of hospital costs for specialist palliative care and differ between care types defined on the basis of treatment goals. Care types provide an important yet – until now – missing explanatory framework for differences in hospital costs of specialist palliative care.
The data are not publicly available due to restrictions e.g. their containing information that could compromise the privacy of research participants. The deidentified data, study protocol, and analytic code that support the findings of this study are available on reasonable requests for meta-analysis. Investigators who propose use of the data should have non-commercial research goals and need approval by an independent review committee. Requests are best proposed beginning March 2026 and ending May 2027 to the provided email from the corresponding author [MH].
We thank the anonymous reviewers, patients for sharing their data and Dr Kristin Marie Bivens for scientific editing.
This work was supported by the Swiss Cancer Research foundation (KFS-6062-02-2024) and Swiss National Science Foundation (SNSF) (grant numbers 10531G_212822). Grant providers had no influence on designing the study; collecting, analysing and interpreting data; writing the report; and deciding to submit the article for publication.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1.Kato K, Fukuda H. Comparative economic evaluation of home-based and hospital-based palliative care for terminal cancer patients. Geriatr Gerontol Int. 2017 Nov;17(11):2247–54. doi: https://doi.org/10.1111/ggi.12977
2.Mosoiu D, Dumitrescu M, Connor SR. Developing a costing framework for palliative care services. J Pain Symptom Manage. 2014 Oct;48(4):719–29. doi: https://doi.org/10.1016/j.jpainsymman.2013.11.017
3.Smith S, Brick A, O’Hara S, Normand C. Evidence on the cost and cost-effectiveness of palliative care: a literature review. Palliat Med. 2014 Feb;28(2):130–50. doi: https://doi.org/10.1177/0269216313493466
4. Hagemann M, Zambrano SC, Bütikofer L, Bergmann A, Voigt K, Eychmüller S. Which Cost Components Influence the Cost of Palliative Care in the Last Hospitalization? A Retrospective Analysis of Palliative Care Versus Usual Care at a Swiss University Hospital. Journal of Pain and Symptom Management. 1. Januar 2020;59(1):20-29.e9.
5.Becker C, Leidl R, Schildmann E, Hodiamont F, Bausewein C. A pilot study on patient-related costs and factors associated with the cost of specialist palliative care in the hospital: first steps towards a patient classification system in Germany. Cost Eff Resour Alloc. 2018 Oct;16(1):35. doi: https://doi.org/10.1186/s12962-018-0154-3
6.Freytag A, Meissner F, Krause M, Lehmann T, Jansky MK, Marschall U, et al. [A regional comparison of outcomes quality and costs of general and specialized palliative care in Germany: a claims data analysis]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2023 Oct;66(10):1135–45. doi: https://doi.org/10.1007/s00103-023-03746-9
7.Chanthong P, Punlee K, Kowkachaporn P, Intharakosum A, Nuanming P. Comparison of direct medical care costs between patients receiving care in a designated palliative care unit and the usual care units. Asia Pac J Clin Oncol. 2023 Aug;19(4):493–8. doi: https://doi.org/10.1111/ajco.13882
8.Perdikouri K, Katharaki M, Kydonaki K, Grammatopoulou E, Baltopoulos G, Katsoulas T. Cost and reimbursement analysis of end-of-life cancer inpatients. The case of the Greek public healthcare sector. J Cancer Policy. 2023 Mar;35:100408. doi: https://doi.org/10.1016/j.jcpo.2023.100408
9.Simoens S, Kutten B, Keirse E, Berghe PV, Beguin C, Desmedt M, et al. Costs of terminal patients who receive palliative care or usual care in different hospital wards. J Palliat Med. 2010 Nov;13(11):1365–9. doi: https://doi.org/10.1089/jpm.2010.0212
10.Isenberg SR, Lu C, McQuade J, Razzak R, Weir BW, Gill N, et al. Economic Evaluation of a Hospital-Based Palliative Care Program. J Oncol Pract. 2017 May;13(5):e408–20. doi: https://doi.org/10.1200/JOP.2016.018036
11.Abian MH, Antón Rodríguez C, Noguera A. End of Life Cost Savings in the Palliative Care Unit Compared to Other Services. J Pain Symptom Manage. 2022 Nov;64(5):495–503. doi: https://doi.org/10.1016/j.jpainsymman.2022.06.016
12.Martins Rozman L, Gonçalves Campolina A, González Patiño E, Coelho de Soárez P. Factors Associated with the Costs of Palliative Care: A Retrospective Cost Analysis at a University Cancer Hospital in Brazil. J Palliat Med. 2021 Sep;24(10):1481–8. doi: https://doi.org/10.1089/jpm.2020.0600
13. May P, Normand C, Cassel JB, Del Fabbro E, Fine RL, Menz R, u. a. Economics of Palliative Care for Hospitalized Adults With Serious Illness: A Meta-analysis. JAMA Intern Med. 1. Juni 2018;178(6):820–9.
14.Walker H, Anderson M, Farahati F, Howell D, Librach SL, Husain A, et al. Resource use and costs of end-of-Life/palliative care: ontario adult cancer patients dying during 2002 and 2003. J Palliat Care. 2011;27(2):79–88. doi: https://doi.org/10.1177/082585971102700203
15.Eagar K, Green J, Gordon R. An Australian casemix classification for palliative care: technical development and results. Palliat Med. 2004 Apr;18(3):217–26. doi: https://doi.org/10.1191/0269216304pm875oa
16. Hodiamont F, Schatz C, Gesell D, Leidl R, Boulesteix AL, Nauck F, u. a. COMPANION: development of a patient-centred complexity and casemix classification for adult palliative care patients based on needs and resource use - a protocol for a cross-sectional multi-centre study. BMC Palliat Care. 4. Februar 2022;21(1):18.
17. Guo P, Dzingina M, Firth AM, Davies JM, Douiri A, O’Brien SM, u. a. Development and validation of a casemix classification to predict costs of specialist palliative care provision across inpatient hospice, hospital and community settings in the UK: a study protocol. BMJ Open. 17. März 2018;8(3):e020071.
18.Eychmüller S, Ebneter AS, Fliedner M. Zentrum für Palliative Care Universitätsspital Bern; 2024. Verfügbar unter: https://palliativzentrum.insel.ch/fileadmin/Palliativzentrum/Bilder/Aerzte_und_Zuweiser/RL_CareTypes.pdf
19. Sturny, I. (2020). The Swiss health care system. International profiles of health care systems, 191.
20. Stürmer T, Webster-Clark M, Lund JL, Wyss R, Ellis AR, Lunt M, u. a. Propensity Score Weighting and Trimming Strategies for Reducing Variance and Bias of Treatment Effect Estimates: A Simulation Study. Am J Epidemiol. 1. August 2021;190(8):1659–70.
21.Cole SR, Hernán MA. Adjusted survival curves with inverse probability weights. Comput Methods Programs Biomed. 2004 Jul;75(1):45–9. doi: https://doi.org/10.1016/j.cmpb.2003.10.004
22. Lee LA, Eagar KM, Smith MC. Subacute and non-acute casemix in Australia. Med J Aust. 19. Oktober 1998;169(S1):S22-25. doi: https://doi.org/10.5694/j.1326-5377.1998.tb123471.x
23.HealthData.gov. [Internet]. [zitiert 2. Juni 2024]. Verfügbar unter: https://healthdata.gov/browse?q=Case%20mix%20index%20retrieved%202024-11-04&sortBy=relevance
24.Eagar K, Gordon R, Green J, Smith M. An Australian casemix classification for palliative care: lessons and policy implications of a national study. Palliat Med. 2004 Apr;18(3):227–33. doi: https://doi.org/10.1191/0269216304pm876oa
25.Masso M, Allingham SF, Banfield M, Johnson CE, Pidgeon T, Yates P, et al. Palliative Care Phase: inter-rater reliability and acceptability in a national study. Palliat Med. 2015 Jan;29(1):22–30. doi: https://doi.org/10.1177/0269216314551814
26.Eagar K, Watters P, Currow DC, Aoun SM, Yates P. The Australian Palliative Care Outcomes Collaboration (PCOC)—measuring the quality and outcomes of palliative care on a routine basis. Aust Health Rev. 2010 May;34(2):186–92. doi: https://doi.org/10.1071/AH08718
27.Murtagh FE, Guo P, Firth A, Yip KM, Ramsenthaler C, Douiri A. u. a. A casemix classification for those receiving specialist palliative care during their last year of life across England: the C-CHANGE research programme [Internet]. Southampton (UK): National Institute for Health and Care Research; 2023 [zitiert 2. Juni 2024]. (Programme Grants for Applied Research). Verfügbar unter: http://www.ncbi.nlm.nih.gov/books/NBK597740/
28.May P, Garrido MM, Del Fabbro E, Noreika D, Normand C, Skoro N, et al. Does Modality Matter? Palliative Care Unit Associated With More Cost-Avoidance Than Consultations. J Pain Symptom Manage. 2018 Mar;55(3):766–774.e4. doi: https://doi.org/10.1016/j.jpainsymman.2017.08.011
29. Morrison RS, Penrod JD, Cassel JB, Caust-Ellenbogen M, Litke A, Spragens L, u. a. Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med. 8. September 2008;168(16):1783–90.
30.Starks H, Wang S, Farber S, Owens DA, Curtis JR. Cost savings vary by length of stay for inpatients receiving palliative care consultation services. J Palliat Med. 2013 Oct;16(10):1215–20. doi: https://doi.org/10.1089/jpm.2013.0163
31.PricewaterhouseCoopers. Schweizer Spitäler: So gesund waren die Finanzen 2022 [Internet]. 2023 [zitiert 4. Juni 2024]. Verfügbar unter: https://www.pwc.ch/de/insights/gesundheitswesen/spitalstudie-2023.html
32.Chai H, Guerriere DN, Zagorski B, Kennedy J, Coyte PC. The size, share, and predictors of publicly financed healthcare costs in the home setting over the palliative care trajectory: a prospective study. J Palliat Care. 2013;29(3):154–62. doi: https://doi.org/10.1177/082585971302900304
33.Chai H, Guerriere DN, Zagorski B, Coyte PC. The magnitude, share and determinants of unpaid care costs for home-based palliative care service provision in Toronto, Canada. Health Soc Care Community. 2014 Jan;22(1):30–9. doi: https://doi.org/10.1111/hsc.12058
34.Plonk WM Jr, Arnold RM. Terminal care: the last weeks of life. J Palliat Med. 2005 Oct;8(5):1042–54. doi: https://doi.org/10.1089/jpm.2005.8.1042
35.Yen PY, Kellye M, Lopetegui M, Saha A, Loversidge J, Chipps EM, et al. Nurses’ Time Allocation and Multitasking of Nursing Activities: A Time Motion Study. AMIA Annu Symp Proc. 2018 Dec;2018:1137–46.
36. Christ SM, Hünerwadel E, Hut B, Ahmadsei M, Matthes O, Seiler A, u. a. Socio-economic determinants for the place of last care: results from the acute palliative care unit of a large comprehensive cancer center in a high-income country in Europe. BMC Palliative Care. 8. August 2023;22(1):114.
37. Stettler P, Bischof P, Bannwart L. Bevölkerungsbefragung Palliative Care 2017. Ergebnisse der Befragung 2017 und Vergleich zur Erhebung von 2009. Bern: Bundesamt für Gesundheit; 2018.[ [cited 2024 Jun 1]], Available at https://www.plattform-palliativecare.ch/sites/default/files/page/files/2018_Bev%C3%B6lkerungsbefragung_Palliative%20Care_Schlussbericht_1.pdf
38. Lee EJ, Lee NR. Factors associated with place of death for terminal cancer patients who wished to die at home. Medicine (Baltimore). 30. September 2022;101(39):e30756. doi: https://doi.org/10.1097/MD.0000000000030756