Analysis of the need for a mobile application to support family caregivers of patients
with incurable cancer – The development of the “Angehörigen-App”: a qualitative study
in Switzerland
DOI: https://doi.org/https://doi.org/10.57187/s.4089
Beat Hubera,
Natalie Rödererb,
Monica Fliednera,
Alexander Wünscha
a University
Centre for Medical Oncology, Inselspital, University Hospital Bern, Bern,
Switzerland
b University
Medical Centre Freiburg, Department of Psychosomatic Medicine and
Psychotherapy, Faculty of Medicine, Albert Ludwigs University, Freiburg,
Germany
Summary
BACKGROUND: The prevalence of cancer is rising continuously worldwide. Relatives
play an important role in caring for cancer patients and are at the same time affected
by the illness and treatment of their loved ones. They have often been referred
to as a forgotten group. Advances in digital technology offer various
opportunities to enhance the well-being of and care for relatives.
OBJECTIVES: The aim of the study was to investigate the utility of a
mobile application to support the relatives of palliative cancer patients in
Switzerland, the potential content elements of such an app, and its optimal
functional and structural design.
METHOD: Using a purposive sampling strategy, three focus group
discussions were conducted at the University Hospital of Bern. The 15
participants included both relatives and experts. Data was analysed using content
structuring qualitative content analysis according to Kuckartz and Rädiker.
RESULTS: Statements from the focus groups were summarised in four main
categories. These included statements from participants about the need for and potential
benefits of an app, such as resource gains or easier access to care. Statements
regarding possible content components of the app, such as tools for
professional support and coordination or the provision of information, were
also summarised. Statements were also included on the necessary functional
features and the structural embedding of the app.
CONCLUSIONS: The results indicate a need for a caregivers app in
Switzerland. The app should reduce gaps in care, focus on family members, and
strengthen their empowerment and access to resources. In terms of content,
bundled information, low-threshold support offers, coordination tools, and
self-care options should be guaranteed. The modular and simply structured app should
be designed in a needs-oriented manner to be used safely throughout
Switzerland.
Introduction
The global prevalence of cancer has increased in recent years, a trend
also seen in the Swiss population [1], and further increases are expected [2]. Despite
improved treatment options, the
number of patients with incurable disease, and thus the absolute number of
deaths per year, is also increasing. Oncology guidelines not only provide standards
for the care of patients but also emphasise the importance of support for their
relatives [3]. In a
meta-analysis of 85 included studies, Pan and Lin [4] report an approximate 42% prevalence
of
depressive symptoms in family caregivers of patients in the palliative stage.
In a study by Rosenberger et al. [5], 95% of family caregivers registered at an outpatient
care centre
reported elevated stress scores on the Distress Thermometer, a screening
instrument for psychosocial distress [6, 7]. However, only 21% reported seeking psycho-oncology
treatment [5]. This treatment gap
is particularly regrettable, as various interventions have been shown to reduce
the psychological and psychosocial stress of relatives and have a positive
effect on their quality of life [8]. This makes it even more important to identify
and reduce the gap
between the significant psychosocial symptom load and the active search for
support. Various barriers, such as lack of information or time and resource
constraints, may be reasons for this gap [9]. Relatives, in particular, are often
neglected in care, partly due to a lack of resources, although they face
enormous challenges in various phases of the disease process [10]. In addition, there
is a lack of low threshold services in outpatient and intermediate settings, and
of the quickly accessible services necessary in crises. Factors specific to certain
groups, such as low socioeconomic status, migration background, living in a
rural environment, or state of health due to illness, also contribute to increased
difficulty in accessing services [11].
One option to overcome such barriers is offered by the continuing digitalisation
of the healthcare sector [12]. In a
narrative review, Springer and Mehnert-Theuerkauf [13] summarise different mobile
health (mHealth) applications
in the field of psycho-oncology, reporting them to be a good addition to
face-to-face psycho-oncological therapy. Lack of evidence regarding the
effectiveness of mHealth applications is still a fundamental problem [14]; this also
applies
to apps for family caregivers [15]. Meanwhile, the majority of applications is tailored
to patients and
do not focus on their caregivers [16]. Even among apps that have been developed specifically
for family
caregivers, most are designed primarily to assist family caregivers in supporting
patients rather than to support the caregivers themselves [17].
The aim of this qualitative study was to determine the need among family
caregivers and professionals for an mHealth application in the form of a mobile
app, which could help to reduce distress in relatives and open up low threshold
access for professional support.
Materials and methods
Study design
This was a
qualitative study which used focus group interviews. The research questions aimed
to determine the need for a digital application in the area of care for
relatives of palliative cancer patients and the potential requirements of such
an app. A qualitative study design was particularly suitable for this, as it
allowed the experiences and expertise of the participants to be recorded as
openly and exploratively as possible. As a result, no hypotheses were made in
advance, and the research questions were designed to be open [18]. The
qualitative study design also enabled a holistic recording of the subjective
considerations of the participants as well as their systematic analysis and
interpretation.
Sampling and recruitment
For the three planned focus groups, a group size of seven people was
targeted, stemming from theoretical considerations regarding the group
composition of people with expert status. Preferably, each group was to consist
of two patient relatives and one specialist from each of the fields of
psychology, nursing, social work, medicine and medical informatics.
To achieve more diverse results, linguistically diverse focus groups were
conducted to ensure representation of the different language regions of
Switzerland in the data collection. The two most populated language regions of
Switzerland were covered by including German and French speakers, with the
largest, German-speaking, population the most represented.
Flyers with study information were distributed in the outpatient clinic
of the medical oncology department at Inselspital Bern and sent to contact
persons of the Cancer League Bern.
People with expert status, referred by the psycho-oncology team at
Inselspital Bern, were approached. Eligible participants were recruited by
email and telephone by an independent person (neither a colleague nor healthcare
professional involved in the care for the sick family member of the participant).
Data collection
Data was collected using focus group interviews. A focus group is
defined as a moderated discourse on a specific topic and can be used to
investigate unknown topics or to present exploratory questions of different
theoretical backgrounds [19].
According to Bär et al. [20], needs
analyses and idea generation are appropriate applications of focus groups, favoured
by the advantages of group dynamics.
A guideline was developed for the interviews based on the phases of group
dynamic processes of focus groups [21]. The interview guideline was developed based
on related topics derived
from literature. For example, the eHealth Suisse criteria catalogue [22] was included.
The
questions also aimed to identify the gaps in care for relatives that emerged
from literature and to generate ideas for digital solutions. As a further
source of ideas for the discussion, examples of existing apps were shown.
The focus groups were conducted in May 2023 at Inselspital Bern and moderated
by a masterʼs student with the support of another master's student as co-moderator.
The discussions were audio-taped so that the collected data
could be further processed.
Data analysis
First, the recordings were transcribed using the simplified
transcription according to Kuckartz [23]. The interviews with the German-language
groups were transcribed directly
into written German. The French-language group interview was first transcribed
and then translated into German using the online tool DeepL and checked by a bilingual
person.
The transcripts were then analysed using qualitative content analysis [24]. Main categories
were established inductively, based on the theoretical background information
and the interview guide. The transcribed data material, consisting of 287 text
passages, was coded using these defined main categories. Subcategories were
derived both inductively and deductively from the transcripts.
The derivation of the category system and the coding of the data was
carried out by one masterʼs student in close consultation with the project leader,
an expert in
qualitative research.
MAXQDA 2022 Analytics Pro software [25] was used as part of the qualitative content
analysis to support the transcription of the audio files and coding.
Ethical considerations
No health-related data were collected or analysed during the needs
assessment, meaning the study does not fall under the Human Research Act. For
this reason, the Cantonal Ethics Committee for Research of the Canton of Bern required
no further action on the ethics request. Nevertheless, the needs analysis was
conducted in compliance with the guidelines of Good Clinical Practice [26], which
also
included obtaining informed consent from the participants. Participants were
informed about the voluntary nature of the study and that they could withdraw
from the study at any time without giving a reason.
Results
Participants
Three focus groups lasting between 70 and 100 minutes were conducted to
collect data for this study. Two of these involved German-speaking participants,
and one was conducted in French. The main socio-demographic details of the
focus group participants, collected in advance by questionnaire, are listed in table
1. A total of n = 15 people took part in the focus groups. There were six
participants in the first German-speaking group and five in the second. The French-speaking
group consisted of four participants. Across all groups, the focus group
participants had a mean age of 47.73 years (Standard deviation: 8.10 years, range:
31–58 years). In focus groups 1 and 3, the gender distribution was balanced. In
focus group 2, there was a 4 to 1 ratio of female to male participants.
Table 1Socio-demographic
information on the participants.
| Focus group |
Gender |
Age (years) |
Profession |
Relative |
Attitude towards digital applications |
| German-speaking groups |
| 1 |
Female |
57 |
Registered nurse |
R |
→ |
| 1 |
Male |
52 |
Psycho-oncologist |
|
→ |
| 1 |
Female |
45 |
Registered nurse |
|
→ |
| 1 |
Female |
52 |
Social worker |
R* |
→ |
| 1 |
Male |
33 |
Medical IT specialist |
R* |
↑ |
| 1 |
Male |
44 |
Oncologist |
R* |
→ |
|
| 2 |
Female |
38 |
Registered nurse |
R |
→ |
| 2 |
Female |
54 |
Psycho-oncologist |
|
→ |
| 2 |
Female |
50 |
Nurse with additional expertise |
R* |
→ |
| 2 |
Female |
58 |
Social worker |
|
↑ |
| 2 |
Male |
55 |
Medical IT specialist |
|
↑ |
| French-speaking group |
| 3 |
Female |
54 |
Music therapist |
|
→ |
| 3 |
Female |
45 |
Nurse with additional expertise |
|
↑ |
| 3 |
Male |
48 |
Social worker |
|
→ |
| 3 |
Male |
31 |
Resident |
|
→ |
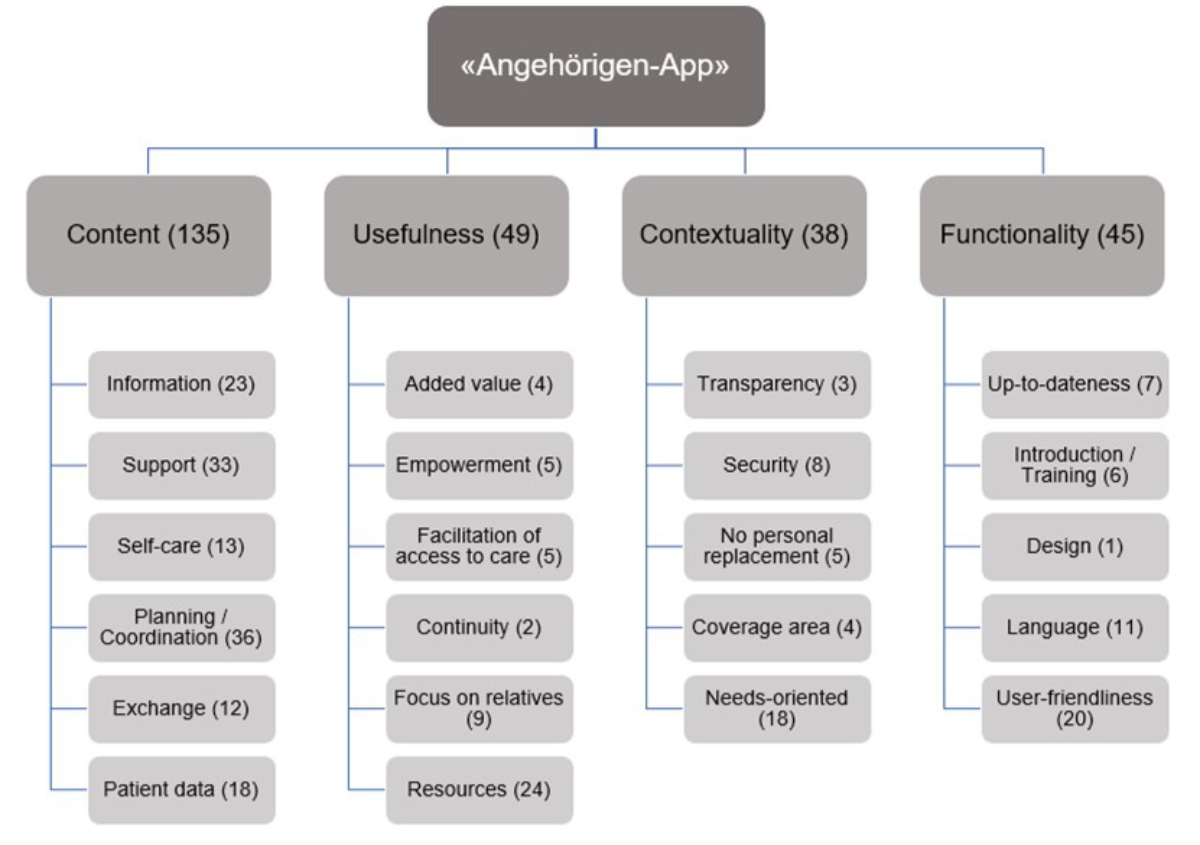
Category system
A category system consisting of four main categories and corresponding
subcategories was developed for a total of 287 text passages;the categories were
derived partly inductively and partly deductively. Figure 1 gives an overview
of the category system. The main categories are discussed in more detail in the
following sections.
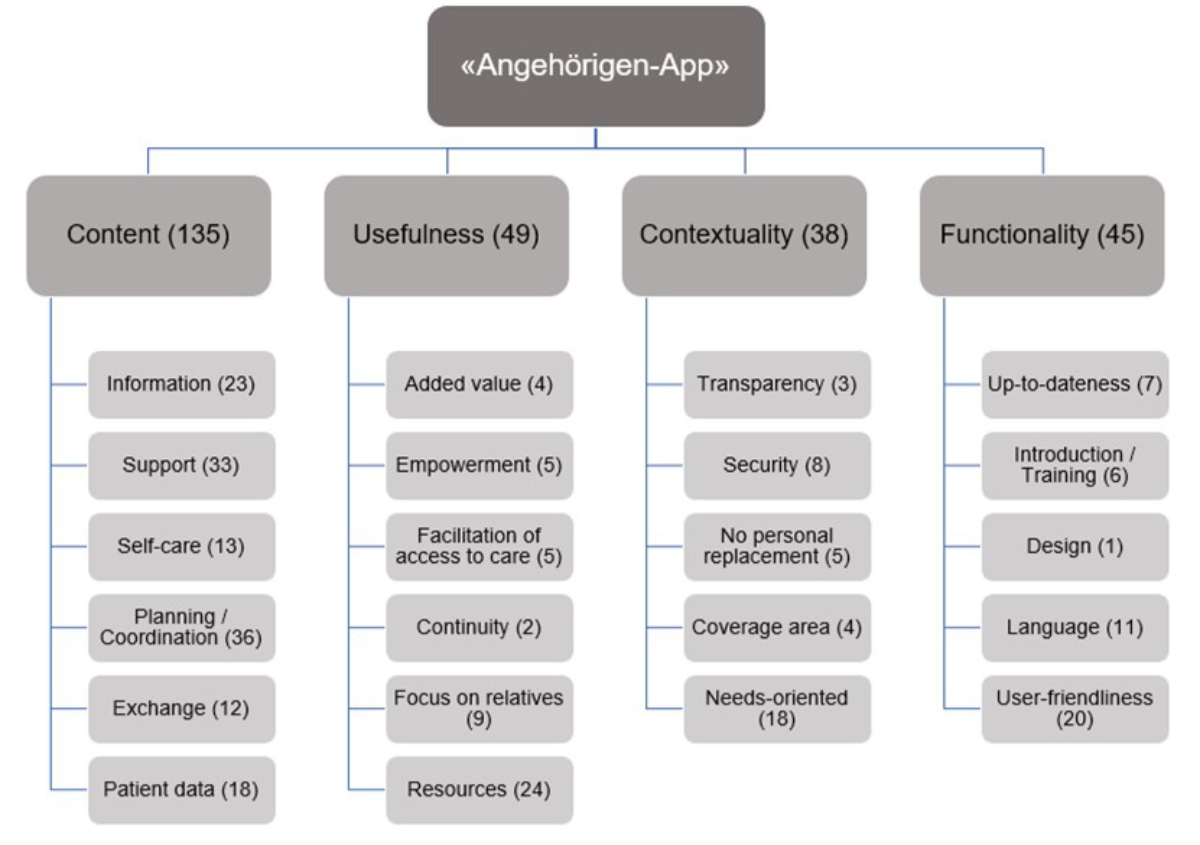
Figure 1Category
system “Angehörigen-App”. The simplified category system developed from
the statements of the focus groups, with the four main categories and corresponding
subcategories. The number of text passages in which the categories were
mentioned is written in brackets. Not shown in this figure is a residual
category containing 20 irrelevant text passages.
Content – What content
elements should the app include?
The requirements regarding content elements of the app are summarised in
the category content. According to the participants, the app should be
used to provide relatives with information. This could cover various topics,
although a specific focus should be placed on legal information. In principle,
the information does not necessarily have to be directly accessible in the app,
but could also be linked to. Summarising the provided information was
considered particularly important.
“And an app like this could at least bundle the
information.”(Psycho-oncologist, focus group 1)
Furthermore, the information content should appeal to different learning
styles, such as visual and auditory, and not just be available in a written
form.
Another element of the appʼs content should be support for relatives. The focus group
participants
mentioned the general need for support, which could, for example, involve
assistance from specialists for yet unanswered questions, or organisational options
for concrete and practical support, such as help for setting up a night watch.
In addition, the need for fast and constant availability was expressed several
times. Digital applications were seen as an opportunity in this context.
“I feel like I should be able to reach someone at any
time to help me with questions. If I have something, I should be able to call a
phone number or use an app to get in contact with someone.” (Medical
IT specialist, focus group 2)
The integration of an emergency button in the app was also discussed as
a concrete solution for constant availability. The feasibility of
implementation must be clarified in advance, as accessibility in emergencies
must be guaranteed at all times if the decision is made to integrate such an
application.
The integration of self-care tools into the app was also mentioned
several times. For example, intervention options of meditation or
self-hypnosis, which are already integrated with other apps, were discussed.
Furthermore, general ideas were suggested to distract relatives from the
stresses of everyday life and to show them ways to find relief or relaxing
moments.
Another suggested content element of the app was a focus on the planning
and coordination of care, covering various aspects such as planning
appointments with healthcare professionals.
“Because they were simply overwhelmed with
coordinating all the appointments that came with the illness.” (Registered
nurse, focus group 1)
More general topics were also discussed, such as coordination between
relatives, patients and specialists, planning over the entire course of the
illness, and future care planning.
One content-related element discussed that proved very controversial was
the opportunity to make contact with peers. Positive aspects, such as the
exchange of experiences and information, were seen to potentially conflict with
negative aspects, such as the risk of negative group dynamics.
There was a consensus among the participants that any opportunities for
exchange, such as chats and forums, should be managed professionally and on an
ongoing basis.
“And I would be careful with chatting, or it would
have to be well moderated, because I think that could also create certain
dynamics that are not necessarily beneficial when youʼre in a
crisis situation.” (Social worker, focus group 1)
It emerged from the discussions that there is no need for a tool to
collect patient data.
“I would perhaps even explicitly exclude the
recording of things like symptoms. I just remember – maybe that has changed in
the meantime – when we were doing research, the adherence to doing it really
conscientiously decreased extremely quickly.” (Oncologist, focus
group 1)
However, it would be desirable to guarantee access to patientsʼ clinical documents
to
simplify exchanges with specialists and ensure that the patientʼs information is up
to date.
Usefulness – What added value
should the app generate?
Specific aspects relating to the practical benefits of an app were
assigned to the category usefulness. The advantages and opportunities
that can arise with the development of a digital application related to care
for relatives were highlighted. From the statements of the participants, various
subcategories were differentiated, as discussed below.
There was a clear consensus among the participants that there must be
some fundamental added value from the app for it to be used. The app should not
simply serve to reproduce or replace something that already exists on the internet.
“All in all, there simply has to be some added
value for me to use it. So basically, why do I need an app?” (Medical
IT specialist, focus group 2)
The fact that digital applications increase the opportunity for self-determination
and autonomy of those affected was also emphasised. On the one hand, this includes
indicating
all available options as the basis for self-determined action. On the other, it
was mentioned that an app can greatly increase accessibility to support. These
two points promote autonomy by reducing dependence on other people and office
hours.
“For me, itʼs that you always
have access, day and night. […] Thatʼs the accessibility,
thatʼs the biggest advantage of digitalisation for me.” (Social
worker, focus group 3)
Facilitating access to care through an app was also mentioned as a
benefit by participants. In this context, the primary barriers to care were
identified as living in rural areas and problems arising from different
cantonal regulations. Digital applications could simplify access, particularly for
people living in rural areas.
“I also think [...] that relatives are often not
given enough support, especially when it comes to non-urban regions. We still
have a lot of people who come from far away, from small villages, and then we
would have more opportunities to support them there.” (Music
therapist, focus group 3)
The desire for continuity over the course of a patientʼs illness emerged as
a further need from the group discussions. Ideally, the affected people, both
patients and their relatives, would experience a certain stability in their
care. For example, this could mean having one main contact person throughout
the course of the illness. Continuity requires many diverse resources, and
digital applications could provide support in this regard.
“There are care advisors who are always in contact
with the patients, from the diagnosis to the end. I think it should go in this
direction, and this could also be on a digital level, it doesnʼt matter.
Continuity is certainly an important point.”(Registered
nurse, focus group 1)
The discussions highlighted the importance of emphasising the
significance of relatives and ensuring a greater focus on them. The statements
made clear that cancer care is strongly centred on the patient and that
relatives are often neglected. As the name suggests, the development of an app
for relatives should be made deliberately for relatives and primarily cover
their needs. For this reason, the importance of involving relatives in the
development was emphasised.
“And that we are visible as relatives. I donʼt know
how it feels for you [a relative is addressed], but it takes a very long time
before relatives are asked how they are doing.” (Nurse with
additional expertise and relative, focus group 2)
In one of the subcategories on usefulness, various aspects were
discussed relating to resource scarcity and resource promotion through digital
applications. The core statements of the professionals emphasised their
experience that time is a very limited resource in care. Meanwhile, relatives
mentioned that every opportunity to save time in the treatment situation is a
gain in quality of life. However, financial resources often limit the extent to
which palliative care is tailored to the needs of those affected. An app could
enable financial savings in certain areas, for example, through improved
coordination. An app could also reduce stress by making certain tasks easier.
However, it is important that constant digital availability does not result in
even more care tasks falling on relatives. In the discussions, the importance
of improving the quality of life was explicitly emphasised by relatives.
“I believe that living life, apart from everything
else, is the most important thing you can still have.” (Relative,
focus group 1)
Contextuality – How should the
app be structurally embedded and organised?
Participants discussed the structural embedding and organisation of the
app. The topics mentioned in this regard were summarised in the category contextuality.
The topic of security was mentioned by the participants. Data protection
was mentioned as a fundamental concern in all focus groups, and was highlighted
as one of the greatest challenges of digitalisation. The integration of data
and documents from patients and controlling access to them could be
particularly problematic.
The category of transparency was relevant for some participants. In this
regard, the importance of a trustworthy provider and the transparent
presentation of sources was mentioned. In addition, reliable sources for the content
should be guaranteed. This would promote trust in the application and its use.
“I also see added value when the provider of such an
app is someone who has a certain level of trust. Especially on the internet, itʼs very
important to have reliable sources that you can recommend.” (Medical
IT specialist, focus group 1)
The participants also emphasised that support from a digital application
is only desirable if the intention behind it is not to replace specialists and
leave those affected with only digital solutions. An app should be used as a
supplementary means to contact professionals, and the support of a person
behind the given information should be guaranteed.
“And also what you said before, that it cannot
replace personal contact. It should be a supplement, an additional security,
provide additional security and give additional input, but not replace a
specialist.” (Registered nurse, focus group 2)
The geographical area that the provided information should cover was
also discussed. The participants agreed that the app should cover a limited area
and not be intended for global use. An exact definition of the boundaries was
not mentioned, but an area of use limited to Switzerland was certainly considered
desirable.
“And I think it really has to be local and specific.
It has to be either be Swiss or German, or something local and culturally
coherent. Because otherwise itʼs difficult.”(Oncologist, focus group 1)
Another relevant point of discussion was the structure of the app. The
app should be developed according to a modular structure appropriate to the
various needs of the relatives. A needs-oriented selection is important because
while relatives can take on different roles in patientsʼ care, they also have different
needs of
their own. These needs may depend on the relationship between the relative and
the patient and the relativeʼs age, as children and adolescents may also be affected
and would have
different needs. On the other hand, the needs also depend on the situational
conditions, such as the stage of the patientʼs illness.
“Perhaps also divided into different roles, e.g.
grandparents, children, or adults; very close caregivers or spouses. You could
divide them up according to who is affected by what. I think the needs of these
groups are different.” (Psycho-oncologist, focus group 2)
The topic of separating content between relatives and the patient was
also discussed. It emerged that the question of clear separation must be
addressed before an app is developed. The tendency of the participantsʼ statements
was
strongly in the direction of a modular division. It should also be taken into
account that relatives should be able to choose for themselves which modules
would be suitable for them.
Functionality – What functional
and technical features should the app contain?
It was possible to define the main category functionality, which
covers aspects that deal with the functional and technical features of the app.
The various subcategories that emerged from the participantsʼ discussions on the
topic of functionality are explained below.
The support and maintenance of the app after its launch were emphasised
as important aspects. Continuous further development and updating of the app were
mentioned as absolutely essential. Participant statements refer to the content itself,
which should not contain any outdated information, while also highlighting the
importance of ensuring technical support and continuous development of the
application.
“It should certainly also be up to date. If you say
you want to network with advisory services or local networks, then it shouldnʼt be
outdated so that you canʼt find information that is no longer valid.” (Social
worker, focus group 1)
Participants also mentioned the need for expert introductory training on
how to use the app. The lack of initial training could lead to potential users
being lost as they feel overwhelmed by the app and consequently stop using it.
One exclusion criterion mentioned was the potential unappealing design
of the app.
“If it looked ugly. If it were an ugly app” (Psycho-oncologist,
focus group 2)
Otherwise, the visual design of the app was not discussed in detail.
Great importance was attached to the topic of language. The subjects of
multilingualism and simplified language were both discussed. Due to the
different national languages, and the different countries of origin of those
affected, the importance of language selection was emphasised. On one hand,
this relates to the language settings of the app itself, but should also be
ensured at the content level whenever possible.
“And if the information is now available in German,
then itʼs no problem to make it available in French,
Albanian or other languages.” (Psycho-oncologist, focus group 1)
Simplified language is primarily about considering the various
circumstances which can make complex language more difficult to understand. The
content should be offered in simplified language so that people with cognitive
impairments, for example, can also make optimum use of it.
“Ah yes, that reminds me of the whole concept of ʻsimplified
languageʼ. We havenʼt thought about it
yet. Especially for sick people with cognitive problems.” (Music therapist,
focus group 3)
An important aspect in terms of functionality is the user-friendliness
of the app. Complexity should be avoided so that the app is not overloaded with
content and information and is kept simple.
“It can also be too complicated. We have suggested
many things. I think it will be difficult to make something simple out of it.” (Resident,
focus group 3)
In addition, participants discussed the need for options for functional
customisation. This relates to aspects of the settings, such as font size, and
also for using the app on different end devices.
“And Iʼm thinking of the
people who are already of a certain age. It would also be good if the font can
be a certain size.” (Social worker, focus group 3)
The app should function in such a way that no mandatory information needs
to be filled in for it to be used. The participants expressed their disapproval
of apps that can only be used if, for example, several questions have been
answered first. They pointed out that advertising, mandatory newsletters, and
constant requests to use the app should be avoided.
“So that there is not a newsletter that is offered
or that is mandatory. I understand if someone says: No, I donʼt want
to.” (Music therapist, focus group 3)
Differences between language regions
Finally, the participants discussed the differences between the language
regions and how these should be addressed in the development of the app. The participants
mainly referred to the problems that could arise due to the different languages
and cultures of the regions. These include, for example, the difficulty of
adequately treating German-speaking patients in French-speaking care facilities
and vice versa, resulting from a lack of bilingual staff. It was also mentioned
that coordination between facilities in the different language regions is not
always optimal.
“And I have to say that I also find it scandalous,
but really scandalous, that we have too few resources, for example in
translation.” (Nurse with additional expertise, focus group 3)
Discussion
Main findings
This study served as a needs analysis and the basis for the development
of content and structure of a mobile support app for family caregivers of
patients with advanced life-limiting cancer. The analysis of the statements
from the focus groups led to the identification of four main categories with
corresponding subcategories. The main categories covered the topics of content
elements, general usefulness, structural embedding, and functionality of the
app.
Need and usefulness
According to the participants, relatives are often neglected in the
treatment process. From the discussions, it emerged that there is a general need
for an app to provide psychological support for the relatives of people with life-limiting
cancer in Switzerland. This is in line with the report by Given et al. [10], which
states the
importance of support measures for relatives to reduce various stress factors.
In the development of an app for family caregivers, specifically taking
their needs into account was seen as a possible measure. According to participants,
several barriers that make it difficult to provide optimal care must be considered.
A lack of care services, disadvantages for patients with limited financial
resources [11], and a
lack of time for professionals [9] were key factors mentioned. The intended app can
be seen as a
low-threshold service that can provide support, for example, during the
bridging period between diagnosis and the initiation of the treatment. Increased
efficiency through digital applications is accompanied by both time savings for
professionals and a reduction in costs for service providers, which in turn
could have positive long-term effects in terms of cost reduction for service
users [27]. In
addition, the gap in care is particularly noticeable in rural areas [11], which was
also
mentioned by participants. However, they immediately emphasised the potential
of digital applications to counteract these effects in undersupplied rural
regions.
The participants also emphasised that an app can help promote autonomy
and ensure constant access to services. One study showed that relatives who
received app-based empowerment support had lower stress scores on the Distress
Thermometer than those in the control group [28], reinforcing our participantsʼ statements.
The
results of the aforementioned study also showed that empowerment support was
associated with higher scores in terms of quality of life. The aspects of
reducing stress and increasing quality of life were mentioned by the
participants as an advantage of digital support apps.
Content elements
In terms of the content requirements of the app, a number of aspects
were mentioned by participants. One important aspect concerned the provision of
information, which should be bundled and clearly presented. Given the enormous
amount of information available, it can be challenging to select and provide
relevant information. Therefore, it will be important to ensure well-founded
and up-to-date information, especially on legal and financial aspects, to
reduce any additional burden for relatives [29].
The need for increased support for relatives by healthcare professionals
has been previously recognised and should be urgently promoted [10]. As mentioned
by participants,
support is necessary throughout the course of the illness and should include
rapid availability and professional assistance in emergencies. For example, the
app should ensure that rapid personal contact is guaranteed when necessary. An
emergency button could offer the concrete possibility of assistance. It remains
to be defined whether the contact would be a single triaging professional or
several contacts would be available for specific topics. It should be possible
to make an emergency call 24/7 through the app to initiate support within a
very short time. However, the service behind this emergency button still needs
to be clarified.
Coordinating appointments with third parties is one of the other tasks
that can place an extra burden on relatives, in addition to caring for the
person with cancer [30]. If such
additional administrative tasks could be simplified using an app, it would
relieve the burden of planning on relatives. It was mentioned that coordination
between parties could be optimised using digital applications, both between
caretakers and professionals and within care teams. In this respect, digitalisation
offers opportunities to make internal communication more efficient, which also
saves time and reduces costs [27].
According to participants, the inclusion of detailed psychosocial
interventions, such as relaxation exercises – or at least a link to relevant information
– should be considered. The app should also contain suggestions that are not
necessarily intervention-based. The effectiveness of various eHealth
interventions for relatives has already been proven, including increases in
quality of life measurements and a reduction in depressive symptoms in family
caregivers [31]. These
findings support the integration of interventions into the app, although these
must be scientifically based and tailored to the individual.
When integrating content elements, two aspects were discussed critically
with some controversy. One aspect was personal exchanges between those
affected. If a chat or forum function is provided for personal exchanges, it
must be ensured that valid information is provided in a professional manner. Although
support groups are less important as a source of information for relatives than
for patients and are less important than the internet in terms of information
access [32], it has
been indicated that internet support groups have positive effects on social
support and self-efficacy of family caregivers [33]. This need should be investigated
further.
Another critical aspect was the specific collection of patient data using
an app. One study reported positive correlations between electronic symptom
recording by patients and their treatment outcomes [34]. The participantsʼ scepticism
is nevertheless justified, as the
app would be aimed towards relatives and the patients; data collection could
mean additional effort on the part of caregivers. However, the integration of
existing relevant documents could be considered, as this would facilitate
communication between professionals and family caregivers, provided these
documents are up to date.
Functionality and contextuality
The participants also addressed the question of the functionality and
structural embedding of the app. In terms of functionality, the aim would be to
achieve a high level of user acceptance. The participants considered it essential
that the app is not complex and is kept as simple as possible. Wang and Qi [35] summarise
that the
simplicity of an app and user acceptance are related. In terms of
user-friendliness, the need for modifiable functional settings, such as font
size, was also mentioned by the participants. This is in line with the
usability quality principle of the eHealth Suisse criteria catalogue for
self-declaration of the quality of health apps, which states that an app should
be functionally customisable for specific target groups [22]. The eHealth Suisse
criteria catalogue also emphasises the importance of ensuring apps are
technically up to date, a requirement also mentioned by the participants. This
includes the transparent, comprehensible, and traceable presentation of sources
and information. Furthermore, the use of a reputable publisher within the app was
discussed as a central aspect of the "transparency" quality principle.
Data protection was mentioned by the participants as one of the main
concerns regarding the use of digital applications. In a study by Kessel et al.
[36] on the
use of app-assisted cancer care, data protection was named as one of the most
important issues needing consideration. The relevance of taking data protection
into account in the development of the app was further increased by the
revision of the Federal Act on Data Protection in Switzerland, which has been
in force since September 2023. The new Federal Act stipulates that necessary
data protection and processing principles, such as ensuring the highest level
of security when introducing a product, must already be taken into account in
the planning and development of any digital application [37].
A fundamental question for participants was whether the app should be
designed for relatives more generally, or specifically those in a caregiving
role. The participants indicated that both aspects could be integrated.
However, these should be modularly separated, and the decision to access different
modules should lie with the user. The app should also take personal and
situational needs into account. For example, a modular selection should make it
possible for a user to choose relevant information depending on whether they
are a caregiver, or on the patientʼs stage of illness. In addition, the varying needs
of different users
should be considered in terms of their role in relation to the patient, as the
stresses and concerns of relatives with different roles are diverse [38]. The supportive
value of an app as an addition to the care structure was emphasised in all
focus groups. However, it is imperative to avoid giving family carers the
feeling that the app is replacing personal support from healthcare
professionals.
Implications regarding language regions
The inclusion of different language regions in the development of the
app was an asset in this study, because of the regional differences in the
Swiss healthcare system [39]. The
statements from the focus groups mainly referred to problems that arise due to
the different languages spoken. When developing the app, it will therefore be
important to cover the linguistic diversity of Switzerland. In terms of its
functionality, the possibility of using the app in different languages is part
of this, but regional linguistic integration should go further. The content,
such as region-specific information or links, should be specifically tailored
so that the app is useful throughout Switzerland. The importance of
coordination between care facilities was also mentioned, especially when it
comes to facilities across different language regions. In this regard, the development
of the app should target comprehensive integration in oncological care
facilities across Switzerland to increase the efficiency of coordination on an
interregional level.
Limitations
The generalisability of our findings is limited for various reasons. We did
not achieve the planned number of participants due to last-minute withdrawals. In
addition, the target of two patient relatives per focus group could not be
achieved. It should also be noted that 10 of the 15 participants, regardless of
their mother tongue, were employees of Inselspital Bern. However, the
participants in the French-speaking focus group were able to draw on their
experience of previous employment in French-speaking regions. Additional
interviews in French-speaking regions of Switzerland could add insights into
regional differences.
The fundamental problem of the adequate transferability of classical
quality criteria to qualitative content analysis posed a methodological
challenge [40]. However,
the use of the classic quality criteria in qualitative research has been
criticised. Other quality criteria, such as transparency or intersubjectivity,
are more relevant when conducting qualitative research [41, 42] and were therefore
taken
into account in this study. Nevertheless, the lack of resources for
implementing the recommended reliability provisions in content analyses [24, 40] remained
a
challenge. Intercoder reliability was not applicable for resource-related
reasons; nonetheless, the creation and revision of the category system took
place in close consultation with the project leader.
Conclusion
The outcomes of this analysis indicate that there is a need for an app
for the relatives of patients with incurable cancer in Switzerland. Reducing
the known barriers to care [11] and an increased focus on relatives are two key aspects
that should be
achieved with an app. Digital applications have the potential to increase the
empowerment of relatives and strengthen their use of resources. Relevant structural,
functional, and content-related needs for achieving the objectives were also
identified. The potential “Angehörigen-App” should be developed in structured
modules, whose use can be adapted depending on the needs of the relatives, increasing
its effectiveness [31]. The
development of the app should take place under consideration of quality
criteria, which include the topics of transparency, data security, and various
functional requirements [22].
Furthermore, the future app should appeal to users from all over Switzerland
due to its simplicity. A relevant added value of the app should be to provide
content that is tailored to the Swiss healthcare system and takes regional
circumstances into account. The content should consist of diverse but bundled
information, support and coordination tools, data storage options, and
self-care options. The aim of the app is not to replace personal contacts with
healthcare providers, but to offer additional support for relatives during the
illness of their loved ones.
Statement on data availability
To protect the privacy of the participants, the
data that support the findings of this study are available from the
corresponding author, AW, upon reasonable request.
Acknowledgments
The authors would like to thank all relatives
and experts for their participation in the focus groups. We would also like to
thank Professor Birgit Kleim for her contribution to this study and Amandine
Pichon for her support in conducting the focus groups and processing the data.
Prof. Dr. phil.
Alexander Wünsch
Inselspital, Bern
University Hospital
Department of Medical Oncology
Freiburgstrasse
CH-3010 Bern
Alexander.Wuensch[at]insel.ch
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global
cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for
36 cancers in 185 countries. CA Cancer J Clin. 2021 May;71(3):209–49. 10.3322/caac.21660
2. Cirillo P, Feller A, Hošek M, et al. Schweizerischer Krebsbericht 2021: Stand und
Entwicklungen. Bundesamt für Statistik (BFS); 2021. Available from https://www.swissstats.bfs.admin.ch/collection/ch.admin.bfs.swissstat.de.issue211411772100/article/issue211411772100-01
3. Schweizerische Gesellschaft für Psychoonkologie. Leitlinien zur psychoonkologischen
Betreuung von erwachsenen Krebskranken und ihren Angehörigen. SGPO. 2023. Available
from: https://www.psychoonkologie.ch/storage/app/media/downloads/2024_SGPO_Leitlinien.pdf
4. Pan YC, Lin YS. Systematic review and meta-analysis of prevalence of depression among
caregivers of cancer patients. Front Psychiatry. 2022 May;13:817936. 10.3389/fpsyt.2022.817936
5. Rosenberger C, Höcker A, Cartus M, Schulz-Kindermann F, Härter M, Mehnert A. Angehörige
und Patienten in der ambulanten psychoonkologischen Versorgung: Zugangswege, psychische
Belastungen und Unterstützungsbedürfnisse [Outpatient psycho-oncological care for
family members and patients: access, psychological distress and supportive care needs].
Psychother Psychosom Med Psychol. 2012 May;62(5):185–94. 10.1055/s-0032-1304994
6. Holland J; National Comprehensive Cancer Network. NCCN practice guidelines for the
management of psychosocial distress. Oncology (Williston Park). 1999 May;13 5A:113–47.
7. Mehnert A, Müller D, Lehmann C, Koch U. Die deutsche Version des NCCN Distress-Thermometers:
Empirische Prüfung eines Screening-Instruments zur Erfassung psychosozialer Belastung
bei Krebspatienten. Z Psychiatr Psychol Psychother. 2006;54(3):213–23. 10.1024/1661-4747.54.3.213
8. Ahn S, Romo RD, Campbell CL. A systematic review of interventions for family caregivers
who care for patients with advanced cancer at home. Patient Educ Couns. 2020 Aug;103(8):1518–30.
10.1016/j.pec.2020.03.012
9. Dilworth S, Higgins I, Parker V, Kelly B, Turner J. Patient and health professional’s
perceived barriers to the delivery of psychosocial care to adults with cancer: a systematic
review. Psychooncology. 2014 Jun;23(6):601–12. 10.1002/pon.3474
10. Given BA, Given CW, Sherwood P. The challenge of quality cancer care for family caregivers.
Semin Oncol Nurs. 2012 Nov;28(4):205–12. 10.1016/j.soncn.2012.09.002
11. Stocker D, Stettler P, Jäggi J, et al. Versorgungssituation psychisch erkrankter Personen
in der Schweiz. Büro Für Arb- Sozialpolitische Stud BASS. 2016. Available from: https://www.buerobass.ch/fileadmin/Files/2016/BAG_2016_VersorgungssituationPsychischErkrankterPersonen_Schlussbericht.pdf
12. Angerer A, Hollenstein E, Russ C. Der Digital Health Report 21/22: die Zukunft des
Schweizer Gesundheitswesens. ZHAW Zürcher Hochschule für Angewandte Wissenschaften;
2021. Available from: https://www.zhaw.ch/storage/hochschule/medien/news/2021/210914-digital-health-report-2021.pdf
13. Springer F, Mehnert-Theuerkauf A. Content features and its implementation in novel
app-based psycho-oncological interventions for cancer survivors: a narrative review.
Curr Opin Oncol. 2022 Jul;34(4):313–9. 10.1097/CCO.0000000000000836
14. Neary M, Schueller SM. State of the field of mental health apps. Cogn Behav Pract.
2018 Nov;25(4):531–7. 10.1016/j.cbpra.2018.01.002
15. Kelley MM, Powell T, Camara D, Shah N, Norton JM, Deitelzweig C, et al. Mobile Health
Apps, Family Caregivers, and Care Planning: scoping Review. J Med Internet Res. 2024 May;26:e46108.
10.2196/46108
16. Shaffer KM, Turner KL, Siwik C, Gonzalez BD, Upasani R, Glazer JV, et al. Digital
health and telehealth in cancer care: a scoping review of reviews. Lancet Digit Health.
2023 May;5(5):e316–27. 10.1016/S2589-7500(23)00049-3
17. Park JY, Tracy CS, Gray CS. Mobile phone apps for family caregivers: A scoping review
and qualitative content analysis. Digit Health. 2022 Feb;8:20552076221076672. 10.1177/20552076221076672
18. Breuer F. Wissenschaftstheoretische Grundlagen qualitativer Methodik in der Psychologie.
In: Mey G, Mruck K, editors. Handb Qual Forsch Psychol Band 1 Ansätze Anwendungsfelder.
2. Auflage. Wiesbaden: Springer Fachmedien; 2020. p. 27–48.
19. Schulz M, Mack B, Renn O, editors. Fokusgruppen in der empirischen Sozialwissenschaft:
von der Konzeption bis zur Auswertung. Wiesbaden: Springer Verlag; 2012. doi: https://doi.org/10.1007/978-3-531-19397-7
20. Bär G, Kasberg A, Geers S, et al. Fokusgruppen in der partizipativen Forschung. In:
Hartung S, Wihofszky P, Wright MT, editors. Partizipative Forsch. Wiesbaden: Springer
Fachmedien Wiesbaden; 2020. pp. 207–32., Available from http://link.springer.com/10.1007/978-3-658-30361-7_7. 10.1007/978-3-658-30361-7_7 10.1007/978-3-658-30361-7_7
21. Benighaus C, Benighaus L. Moderation, Gesprächsaufbau und Dynamik in Fokusgruppen.
In: Schulz M, Mack B, Renn O, editors. Fokusgruppen Empirischen Sozialwissenschaft.
Wiesbaden: VS Verlag für Sozialwissenschaften; 2012. pp. 111–32., Available from http://link.springer.com/10.1007/978-3-531-19397-7_6. 10.1007/978-3-531-19397-7_6 10.1007/978-3-531-19397-7_6
22. Albrecht UV. Einheitlicher Kriterienkatalog zur Selbstdeklaration der Qualität von
Gesundheits-Apps. Medizinische Hochschule Hannover Bibliothek; 2019. Available from:
https://mhh-publikationsserver.gbv.de/receive/mhh_mods_00000021 https://doi.org/10.26068/MHHRPM/20190416-004
23. Kuckartz U, Dresing T, Rädiker S, et al. Qualitative Evaluation: Der Einstieg in die
Praxis. 2. Aufl. Wiesbaden: VS Verlag für Sozialwissenschaften! GWV Fachverlage GmbH;
2008.
24. Kuckartz U, Rädiker S. Qualitative Inhaltsanalyse: Methoden, Praxis, Computerunterstützung:
Grundlagentexte Methoden. 5th ed. Weinheim, Basel: Beltz Juventa; 2022.
25. MAXQDA. Software für qualitative Datenanalyse. Berlin, Deutschland: VERBI Software.
Berlin, Deutschland: Consult. Sozialforschung GmbH; 2022.
26. Harmonised Guideline IC. Integrated Addendum to ICH E6 (R1): Guideline for Good Clinical
Practice E6(R2). International Council for Harmonisation of Technical Requirements
for Pharmaceuticals for Human Use (ICH); 2016. Available from: https://database.ich.org/sites/default/files/E6_R2_Addendum.pdf
27. Hämmerli M, Müller T, Biesdorf S, et al. Digitalisierung im Gesundheitswesen: Die
8,2-Mrd.-CHF-Chance für die Schweiz. McKinsey Digital; 2021. Available from: https://www.mckinsey.com/ch/~/media/mckinsey/locations/europe%20and%20middle%20east/switzerland/our%20insights/digitization%20in%20healthcare/digitalisierung%20im%20gesundheitswesen%20%20die%2082mrdchance%20fr%20die%20schweiz%20de.pdf
28. Uysal N, Bağçivan G, Özkaraman A, Karaaslan Eşer A, Çetin F, Çalışkan BB, et al. Empowering
caregivers in the radiotherapy process: the results of a randomized controlled trial.
Support Care Cancer. 2021 May;29(5):2395–404. 10.1007/s00520-020-05743-z
29. Mehnert A, Vehling S. Psychoonkologische Unterstützung von Patienten und Angehörigen
in der Terminalphase [Psychooncological support for patients and relatives in the
terminal phase]. Forum (Genova). 2018;33(1):30–4. 10.1007/s12312-017-0363-2
30. Johannsen LJ, Geertz W, Bergelt C, Inhestern L. Belastungen bei Angehörigen von Krebserkrankten
erkennen und versorgen. InFo Hamatol Onkol. 2022;25(6):15–8. doi: https://doi.org/10.1007/s15004-022-9086-3
31. Li Y, Li J, Zhang Y, Ding Y, Hu X. The effectiveness of e-Health interventions on
caregiver burden, depression, and quality of life in informal caregivers of patients
with cancer: A systematic review and meta-analysis of randomized controlled trials.
Int J Nurs Stud. 2022 Mar;127:104179. 10.1016/j.ijnurstu.2022.104179
32. Rudolph I, Seilacher E, Köster MJ, Stellamanns J, Liebl P, Zell J, et al. Der Informationsbedarf
von Patienten mit Krebserkrankungen in Deutschland - eine Befragung von Patienten
und Angehörigen [Survey on information needs of cancer patients and ther relatives
in Germany]. Dtsch Med Wochenschr. 2015 Mar;140(5):e43–7. 10.1055/s-0041-100585
33. Parker Oliver D, Patil S, Benson JJ, Gage A, Washington K, Kruse RL, et al. The effect
of Internet group support for caregivers on social support, self-Efficacy, and caregiver
burden: A meta-analysis. Telemed J E Health. 2017 Aug;23(8):621–9. 10.1089/tmj.2016.0183
34. Basch E, Charlot M, Dueck AC. Population-level evidence of survival benefits of patient-reported
outcome symptom monitoring software systems in routine cancer care. Cancer Med. 2020 Nov;9(21):7797–9.
10.1002/cam4.3480
35. Wang C, Qi H. Influencing factors of acceptance and use behavior of mobile Health
application users: systematic Review. Healthcare (Basel). 2021 Mar;9(3):357. 10.3390/healthcare9030357
36. Kessel KA, Vogel MM, Kessel C, Bier H, Biedermann T, Friess H, et al. Mobile health
in oncology: A patient survey about app-assisted cancer care. JMIR Mhealth Uhealth.
2017 Jun;5(6):e81. 10.2196/mhealth.7689
37. KMU-Portal, für kleine und mittlere Unternehmen. Neues Datenschutzgesetz (revDSG).
2023. Available from: https://www.kmu.admin.ch/kmu/de/home/fakten-trends/digitalisierung/datenschutz/neues-datenschutzgesetz-rev-dsg.html
38. Fenton AT, Keating NL, Ornstein KA, Kent EE, Litzelman K, Rowland JH, et al. Comparing
adult-child and spousal caregiver burden and potential contributors. Cancer. 2022 May;128(10):2015–24.
10.1002/cncr.34164
39. Höglinger M. Mehr Transparenz für alle – der Schweizer Atlas der Gesundheitsversorgung.
Gesundheitsökonomie ZHAW. 2023. Available from: https://blog.zhaw.ch/gesundheitsoekonomie/2023/04/20/mehr-transparenz-fuer-alle-der-schweizer-atlas-der-gesundheitsversorgung/
40. Mayring P. Qualitative Inhaltsanalyse. Grundlagen und Techniken. 13. Überarb. Weinheim:
Beltz Pädagogik; 2022.
41. Baur N, Blasius J, editors. Handbuch Methoden der empirischen Sozialforschung. 3.,
vollständig überarbeitete und erweiterte Auflage. Wiesbaden: Springer VS; 2022. doi: https://doi.org/10.1007/978-3-658-37985-8
42. Mayring P. Einführung in die qualitative Sozialforschung: eine Anleitung zu qualitativem
Denken. 6., überarbeitete Auflage. Weinheim, Basel: Beltz; 2016.