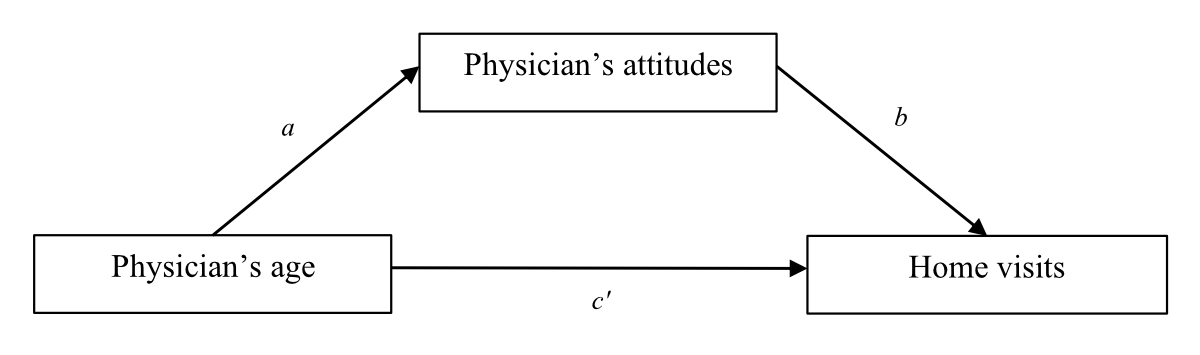
Figure 1Model of the hypothetical association pathways between physician’s age (the predictor), physician’s (negative or positive) attitudes towards home visits (the mediator) and home visits (the outcome).
DOI: https://doi.org/https://doi.org/10.57187/s.4039
Home visits help physicians gain insights into patients’ living conditions and social contexts, addressing medical and psychosocial needs [1, 2]. Family physicians build trust [3], enhance communication and empower patients to actively participate in their healthcare decisions by providing care directly in patients’ homes [4]. A decline in general practitioner (GP) home visits over recent years [5–7] may negatively impact the quality of care, especially for older and frail patients. One reason for the decline may be generational [8]. Compared to their younger counterparts, older physicians may frequently conduct home visits for reasons linked to their model of the doctor-patient relationship in which home visits are seen as a standard and essential part of family medicine. Additionally, there could be a gender effect [8], with female doctors conducting fewer home visits than male doctors due to, for example, family responsibilities or concerns about personal safety. Another reason may lean into individual factors, including attitudes, which refer to positive or negative beliefs, thoughts and attributes associated with home visits that guide behaviours (i.e. number of home visits).
This cross-sectional study was conducted in Canton Ticino (Switzerland) from June to October 2023. The first hypothesis (HP1) tested whether younger general practitioners and female doctors performed fewer home visits (i.e. generational and gender effects on home visits). Age and gender were then the predictors. The second hypothesis (HP2) tested whether positive or negative attitudes (i.e. the mediator) mediated the relationship between age (i.e. the predictor) and home visits (i.e. the outcome).
The eligibility criterion was being a general practitioner. The questions were created ad hoc for this study and pilot-tested with six family doctors. In late June 2023, the Ticino Medical Professional Association (OMCT) invited all members to complete the questionnaire via email. Data collection occurred anonymously via an online link on Qualtrics. Participants provided electronic informed consent. The Institutional Ethical Board approved the study (decision CE_2024_01).
The number of home visits in a typical week.
Gender, age and attitudes. For the latter, 11 items were created ad hoc (see table 1), tapping into positive and negative attitudes regarding home visits (response options ranged from 1 Disagree to 5 Fully agree).
Table 1Factor loadings and results of the factor analysis on the attitude scale items.
| Factor loadings | ||
| Items | Negative attitudes | Positive attitudes |
| The diagnostic and therapeutic options during a home visit are too limited to address anything seriously for the patient. | 0.77 | |
| During home visits, I miss the assistance of the staff I normally have in the clinic. | 0.75 | |
| Compared to a clinic visit, being at a patient’s home might make recognising a serious medical condition challenging. | 0.70 | |
| The presence of relatives during a home visit can lead to family discussions, making my work more complex. | 0.56 | |
| Most home visits are motivated by serious concerns from family members. | 0.71 | |
| During a home visit, I can gather information about my patient’s condition by asking questions to their caregiver. | 0.68 | |
| Seeing me in their home might make people more confident and open in their interactions with me. | 0.68 | |
| In a typical week, I see several patients in my clinic who I would have preferred to stay home and requested a home visit. | 0.46 | |
| I can provide better advice because I see the patient’s living conditions. | ||
| Since I can see my patient, a home visit allows me to provide a much more reliable assessment of their health status than a phone call. | ||
| Most of the home visits I conduct are for patients who would not have been able to come to my clinic. | ||
A first factor analysis on the 11 items (Kaiser-Meyer-Olkin test = 0.73, χ2 (55) = 294.004, p <0.001; 53% of the variance) suggested excluding the last three items because they saturated both factors.
A second factor analysis on the remaining 9 items (Kaiser-Meyer-Olkin test = 0.68, χ2 (28) = 136.34, p <0.001, 28% of the variance) extracted one factor corresponding to negative attitudes (α = 0.67, rs >0.32), and one corresponding to positive attitudes (α = 0.53, rs >0.20).
Number of patients, location of the clinic (rural <10k, suburban 10k–20k, urban area >20k), age of the patients compared to the Swiss average age of 44.8 (younger than, similar to, older than), age of the patients visited at home compared to the Swiss average age of 44.8 (younger than, similar to, older than), half workdays in a week spent on patient care, minutes spent with the patients during a home visit.
A factor analysis was carried out on the 11-item attitude scale to test the two expected factors, i.e. positive and negative attitudes (see table 1).
One-tailed correlations were tested since HP1 hypothesised that younger general practitioners performed fewer home visits. A one-tailed correlation is a statistical test used when there is a specific directional hypothesis about the relationship between two variables, such as in this case (age is a predictor of home visits). Pearson’s r was applied to test HP1 when continuous variables were considered. The effect of gender on home visits was tested with a t-test. The location of the clinic is an ordinal-level variable; therefore, Kendall’s Tau b was used to measure the correlations with other variables. The age of the patients was categorised as an ordinal variable (younger, similar, older than the average Swiss population of 44.8). Therefore, Spearman’s rho correlations were applied to this variable when testing HP1. These analyses were conducted using the software SPSS v. 29.
HP2 was tested with two mediation analyses with 5000 bootstrap samples and 95% confidence intervals, as suggested by Hayes [8], via Process Macro for SPSS v.29, applying ordinary least squares. Age was the independent variable determining home visits (the outcome), with positive attitudes (in the first analysis) and negative attitudes (in the second analysis) as the mediator. Gender was included in the models as a covariate.
According to Hayes [8], a mediation analysis tests (1) the indirect effect, (2) the direct effect and (3) the total effect. As depicted in figure 1, the indirect effect ab combines the association path between age and (positive or negative) attitudes (a in figure 1) and the association path between (positive or negative) attitudes and home visits (b in figure 1). The direct effect c' (see figure 1) tests the association path between age and home visits. The total effect combines the direct and indirect effects: c = c' + ab. The effects of paths a, b and c' are tested via the significance of the betas (standard errors [SE] and 95% confidence intervals are reported as well). The indirect effect ab is tested via the bias-corrected 95% confidence intervals and it is significant when zero is not included in the interval.
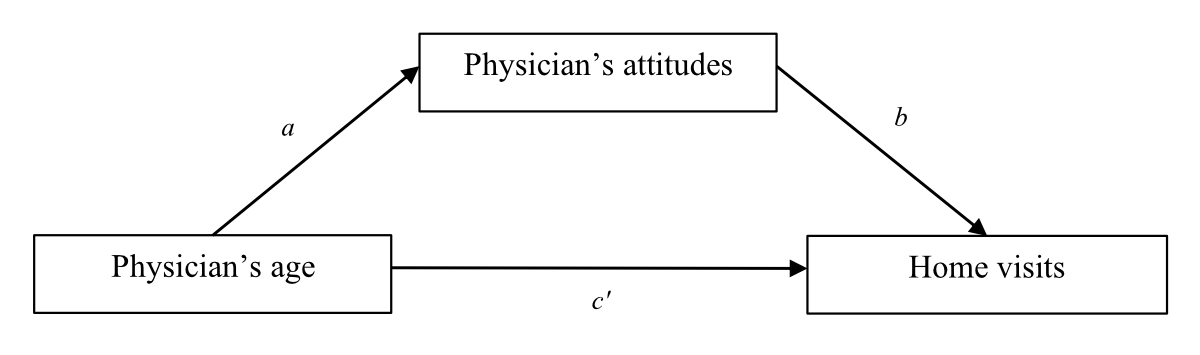
Figure 1Model of the hypothetical association pathways between physician’s age (the predictor), physician’s (negative or positive) attitudes towards home visits (the mediator) and home visits (the outcome).
The mediation analysis is present and called full when the indirect effect ab is significant. If both ab and c' are significant, the mediation is present and called partial. The total effect may or may not be significant.
In the dataset, there was no missing data; continuous variables were normally distributed, and the main assumptions for the mediation models were met.
An a priori sample size was estimated on G*Power.
Expected sample size for HP1 based on correlation: bivariate normal model, two-tailed, effect size = 0.25 (prudentially medium-low), α = 0.05, power = 0.80, sample size min. estimation = 123. Estimated sample size for HP2 based on regression: fixed method, R2 increase, part. R2 = 0.10 (prudentially low), α = 0.05, power = 0.80, sample size min. estimation = 102.
Final sample size n = 142. 135 (95%) doctors reported regularly conducting home visits; the remaining 7 did not conduct home visits. Therefore, the analyses were performed on the 135 general practitioners who conducted home visits. See figure 2 for the inclusion process and table 2 for the basic descriptors.
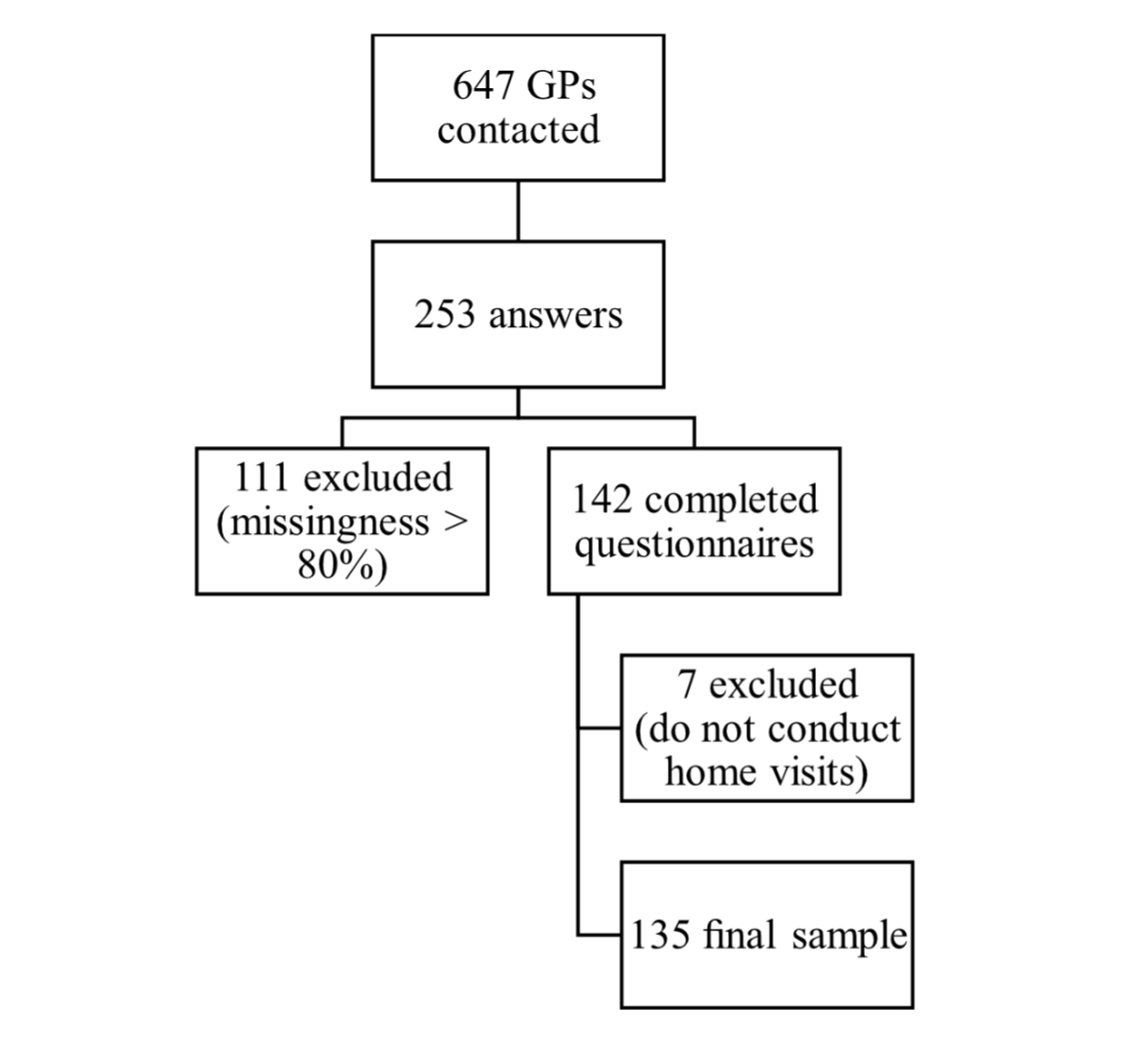
Figure 2Inclusion process.
Table 2Basic descriptive statistics.
| Min | Max | Mean ± standard deviation or n (%) | |
| Physician’s age in years | 36 | 83 | 56±12 |
| Physician’s sex | 72% men | ||
| 28% women | |||
| Location of the clinic | 40% urban area (>20k) | ||
| 30% suburban area (10k–20k) | |||
| 12% rural area (<10k) | |||
| Number of patients | 932±426 | ||
| Age of patients in relation to the Swiss average age of 44.8* | 3% younger | ||
| 30% similar | |||
| 57% older | |||
| Age of patients visited at home in relation to the Swiss average age of 44.8 | 18% similar | ||
| 82% older | |||
| Half workdays in a week | 1 | 12 | 3.5±2 |
| Number of home visits in the past week | 1 | 15 | 3.5±3 |
| Minutes spent with the patient during a home visit | 15 | 60 | 31±11 |
| Positive attitudes | 1.5 | 4.5 | 3.35±0.52 |
| Negative attitudes | 1 | 4.75 | 2.65±0.80 |
* The question was “Compared to the average age of the Swiss population (44.8 years), are your patients younger than, similar to or older than the Swiss average?”
HP1 was confirmed: younger general practitioners conducted fewer home visits than older doctors (see table 3). The t-test, t(100.8) = 3.77, p <0.001, confirmed that female doctors conducted fewer home visits (M = 2.39±1.8) than male doctors (M = 4.09±2.9).
Table 3Correlation analysis (n = 135).
| Age | Location of clinic | N° of patients | Age of patients visited at home | Half workdays | N° of home visits in past week | Minutes spent with patients at home visits | Positive attitude | Negative attitude | |
| Age in years | 1 | −0.06 | 0.12 | −0.08 | −0.004 | 0.32** | −0.15 | 0.15 | −0.38** |
| Location of clinic (reference category = rural area) | 1 | −0.03 | 0.01 | −0.009 | −18* | 0.32** | 0.13 | 0.14 | |
| N° of patients | 1 | −0.12 | 0.20* | 0.11 | −0.13 | 0.08 | −0.17 | ||
| Age of patients visited at home (reference category = younger than the average of 44.8) | 1 | 0.23* | 0.07 | 0.008 | 0.18* | −0.11 | |||
| Half workdays | 1 | 0.18* | 0.002 | −0.05 | −0.02 | ||||
| N° of home visits in past week | 1 | −35** | 0.09 | −0.33** | |||||
| Minutes spent with patients at home visits | 1 | 0.07 | 0.05 | ||||||
| Positive attitude | 1 | −0.12 | |||||||
| Negative attitude | 1 |
* p <0.05
** p <0.001
In the first mediation model, with positive attitudes as the mediator, the indirect path (ab) was not significant, meaning there is no effect of age on home visits through the mediation of positive attitudes.
The second model with the negative attitudes as a mediator showed that younger physicians had more negative attitudes towards home visits (path a figure 3) and more negative attitudes decreased the home visits (path b figure 3). The indirect effect ab was significant, while the direct effect c' was not significant. This combination confirms the full mediation of negative attitudes between age and home visits and endorses HP2. Younger physicians have more negative attitudes towards home visits, leading to fewer home visits, even controlling for gender that was not significant (table 4).
The total effect c was significant.
Table 4Mediation analysis with negative attitudes.
| Mediation | Coefficients | |||
| Effects | B | SE | t | LLCI-ULCI |
| Age on negative attitudes (path a) | −0.02 | 0.007 | 6.6** | −0.04–−0.01 |
| Negative attitudes on home visits (path b) | −0.90 | 0.34 | −2.62* | −1.59–−0.22 |
| Indirect effect (path ab) | 0.02 | 0.01 | 0.004–0.05 | |
| Direct effect (path c') | 0.04 | 0.02 | 1.53 | |
| Total effect (path c = c’ + ab) | 0.06 | 0.02 | 2.49** | 0.01–0.11 |
* p <0.05
** p <0.001. Gender was included as a covariate, but it was not significant.
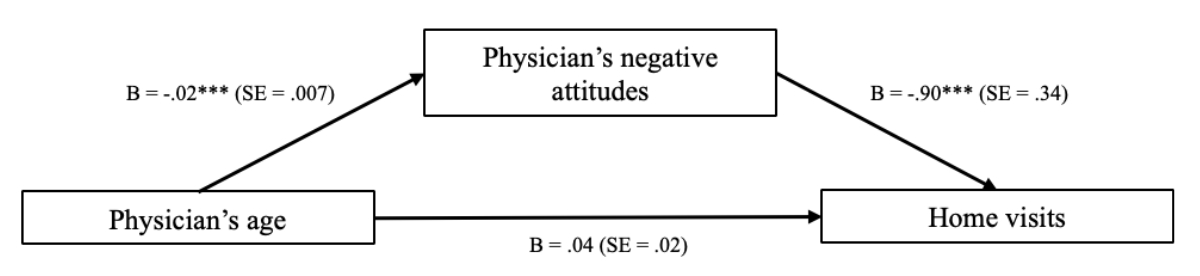
Figure 3Effects of physician’s age on home visits via the mediation of the negative attitudes. B = beta value; SE = standard error. *** p <0.001.
Overall, the findings suggest that most general practitioners (GPs) working in the Italian region of Switzerland reported regularly conducting home visits, emphasising their importance in primary care delivery, especially in areas with an ageing population, despite the concerns about declining trends [7]. The findings also suggested a generational effect on home visits; older general practitioners are more available to reach the patients at home, reflecting their training when home visits were more common [see also 2, 7]. In contrast, female doctors conducted fewer visits but allocated more time [8]. These findings suggest that societal factors influence physicians’ approaches to home visits.
The mediation analysis (HP2) revealed that older physicians exhibited fewer negative attitudes towards home visits, which, in turn, negatively influenced their likelihood of conducting such visits, controlling for gender. These negative attitudes concerned the adequacy of the medical resources and interventions available outside the clinical setting and the technical challenges when delivering care outside the clinic regarding access to ancillary support services and resources. Another perceived barrier was the presence of the relatives during home visits, with participants noting that “family discussions” can detract from the efficiency and focus of the consultation.
Self-reporting, sample size, selection bias and confounding limit the generalisability of the results. The cross-sectional design limits any appreciation of causal relationships. Interventions that promote positive attitudes towards home visits, such as targeted training programmes or initiatives highlighting the benefits of home-based care, may help mitigate the decline in home visit frequency observed among younger physicians. Similarly, future research could benefit from exploring a more comprehensive set of elements to inform interventions to promote and sustain home visit practices in family medicine. By understanding the drivers and barriers influencing home visit practices, healthcare policymakers and practitioners can work towards preserving and enhancing the role of home visits in delivering patient-centred care and promoting the health and wellbeing of diverse patient populations.
The data supporting the findings of this study are available on request from the corresponding author. The available data include individual participant data that underlie the results of this study, after deidentification. The data will be available for a period of 12 months after the publication. The data will be available to anyone who wishes to access the data for meta-analysis purposes.
This study received no funding.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Kao H, Conant R, Soriano T, McCormick W. The past, present, and future of house calls. Clin Geriatr Med. 2009 Feb;25(1):19–34.
2. Theile G, Kruschinski C, Buck M, Müller CA, Hummers-Pradier E. Home visits - central to primary care, tradition or an obligation? A qualitative study. BMC Fam Pract. 2011 Apr;12(1):24. doi: https://doi.org/10.1186/1471-2296-12-24
3. Petrocchi S, Iannello P, Lecciso F, Levante A, Antonietti A, Schulz PJ. Interpersonal trust in doctor-patient relation: evidence from dyadic analysis and association with quality of dyadic communication. Soc Sci Med. 2019 Aug;235:112391. doi: https://doi.org/10.1016/j.socscimed.2019.112391
4. van Kempen JA, Robben SH, Zuidema SU, Olde Rikkert MG, Melis RJ, Schers HJ. Home visits for frail older people: a qualitative study on the needs and preferences of frail older people and their informal caregivers. Br J Gen Pract. 2012 Aug;62(601):e554–60. doi: https://doi.org/10.3399/bjgp12X653606
5. Neuner-Jehle S, Graber SM, Keizer E, Huber C, Blozik E, Rosemann T, et al. Time trends in general practitioners’ home visits for older patients: a retrospective cross-sectional study from Switzerland. Swiss Med Wkly. 2021 Jul;151(2728):w20539. doi: https://doi.org/10.4414/smw.2021.20539
6. Boerma WG, Groenewegen PP. GP home visiting in 18 European countries. Adding the role of health system features. Eur J Gen Pract. 2001 Jul;7(4):132–7.
7. Mueller Y, David S, Cohidon C, Locatelli I, Senn N. Home visits made by general practitioners in the canton of Vaud between 2006 and 2015. Swiss Med Wkly. 2019 Mar 24;149(1112):w20037. doi: https://doi.org/10.4414/smw.2019.20037
8. Cohidon C, Cornuz J, Senn N. Primary care in Switzerland: evolution of physicians’ profile and activities in twenty years (1993-2012). BMC Fam Pract. 2015 Aug;16(1):107. doi: https://doi.org/10.1186/s12875-015-0321-y
9. Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. 3rd ed. Guilford publications; 2017.