Reporting of paediatric exercise-induced respiratory symptoms by physicians and parents:
an observational prospective study
DOI: https://doi.org/https://doi.org/10.57187/s.3939
Eva S. L. Pedersenab,
Sarah Glicka,
Carmen C. M. de Jongac,
Cristina Ardura-Garciaa,
Anja
Jochmannd,
Carmen Casaultace,
Katharina
Hartogf,
Diana Marangu-Booreg,
Dominik Mueller-Suterh,
Nicolas Regameyi,
Florian Singercjk,
Alexander Moellerj,
Claudia E. Kuehniac
a Institute of Social and Preventive Medicine,
University of Bern, Bern, Switzerland
b Department of Clinical Research, University of Bern, Bern,
Switzerland
c Division of Paediatric Respiratory Medicine and Allergology, Department of Paediatrics,
Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland
d Department of Paediatric Respiratory Medicine, University Children’s
Hospital Basel (UKBB), Basel, Switzerland
e Division of Paediatric Pulmonology, Children’s
Hospital Chur, Chur, Switzerland
f Division of Paediatric Pulmonology, Children’s
Hospital St. Gallen, St. Gallen, Switzerland
g Department of Paediatrics and Child Health,
University of Nairobi, Nairobi, Kenya
h Department of Paediatrics, Kantonsspital Aarau, Aarau,
Switzerland
i Division of Paediatric Pulmonology, Children’s
Hospital of Central Switzerland, Lucerne, Switzerland
j Department of Paediatric Pulmonology, University
Children’s Hospital Zurich, University of Zurich, Zurich, Switzerland
k Division of Paediatric Pulmonology and Allergology,
Department of Paediatrics and Adolescent Medicine, Medical University of Graz,
Graz, Austria
Summary
STUDY AIMS: Routinely collected health data are
increasingly used for research; however important anamnestic details may be missing
from medical records. We compared physician documentation of paediatric exercise-induced
respiratory symptoms in clinical notes with parental questionnaire responses for
the same children.
METHODS: We analysed
data from the Swiss Paediatric Airway Cohort (SPAC), a multicentre
observational study of children treated in Swiss outpatient pulmonology clinics.
We included children aged 6 to 17 years who were referred to a paediatric
pulmonologist for evaluation of exercise-induced respiratory symptoms. Features
of exercise-induced respiratory symptoms recorded by physicians were extracted from
outpatient clinic letters transmitted to the referring physician, while
parent-reported exercise-induced respiratory symptom data was collected from a standardised
questionnaire completed at Swiss Paediatric Airway Cohort enrolment. We
calculated agreement between physician-documented and parent-reported exercise-induced
respiratory symptom characteristics using Cohen’s and Fleiss’s kappa.
RESULTS:Of 1669 children participating in the Swiss Paediatric Airway Cohort (2017–2019),
193 (12%) met the inclusion criteria, of whom 48% were girls. Physicians
provided detailed information on exercise-induced respiratory symptoms in 186
(96%) outpatient clinic letters. Documented characteristics included: type of
physical activity triggering exercise-induced respiratory symptoms (69%),
location of exercise-induced respiratory symptoms in chest or throat (48%),
respiratory phase of exercise-induced respiratory symptoms (45%) and timing of exercise-induced
respiratory symptoms during or after exercise (37%). Previous bronchodilator
use (94%) and its effect on exercise-induced respiratory symptoms (88%) were
consistently documented by physicians. The clinic letters for children
diagnosed with dysfunctional breathing more often contained detailed exercise-induced
respiratory symptom characteristics than those diagnosed with
asthma. The level of agreement between physician-documented and parent-reported
exercise-induced respiratory symptoms was moderate for use of bronchodilators (κ =
0.53) and poor-to-fair for all other features (κ = 0.01–0.36).
CONCLUSION: This study highlights that outpatient
clinic letters may lack some details on exercise-induced respiratory symptom
characteristics – information that parents could provide. A standardised and detailed
method for documenting paediatric respiratory
symptoms in the coordinated data infrastructure may
enhance future analyses of routinely collected health data.
Introduction
Exercise-induced
respiratory symptoms are common in childhood [1].
Symptom characteristics vary depending on the underlying respiratory aetiology [2–4],
which may include asthma, dysfunctional
breathing (e.g. inducible laryngeal obstruction, breathing pattern disorders)
or insufficient fitness [5–9]. The domains
of exercise-induced respiratory symptoms – such as timing of onset, severity, perceived
location, relation to exercise intensity and duration, and response to
treatment – are important features in the clinical history. Exercise-induced
wheeze, cough and chest tightness are common in asthma [10, 11], while stridor and
dyspnoea are more often noted with extrathoracic
dysfunctional breathing [9, 11]. Thoracic
dysfunctional breathing is associated with exertional dyspnoea, sighing and
dizziness, and may be accompanied by hyperventilation [12]. Poor differentiation between
isolated or co-existing
dysfunctional breathing and other entities may lead to misdiagnosis,
overtreatment (e.g. inhaled corticosteroids) and excess healthcare costs [13, 14].
Thus, detailed history-taking is essential
for evaluating the differential diagnosis in children referred with exercise-induced
respiratory symptoms.
With the
advent of electronic health record databases and the creation of clinical data
repositories, also known as coordinated data infrastructures, secondary use of routinely
collected health data to promote public health research is evolving [15]. The sharing
of depersonalised health data
will be increasingly important for enhancing the understanding, management and
prevention of disease [16]. The Swiss
Personalised Health Network (SPHN) aims to improve the utilisation of data
obtained during routine healthcare encounters by facilitating accessibility for
research [17]. Swiss paediatricians
agreed to uniformly capture a minimal set of variables in medical records [18], but
recording of symptoms has not been standardised
yet.
To our
knowledge, the comprehensiveness of documentation of exercise-induced
respiratory symptoms in outpatient clinic letters has not been previously studied.
This information is important for understanding the usability of exercise-induced
respiratory symptom-related data for healthcare research through, for example,
text search or similar methods. We analysed the characteristics of exercise-induced
respiratory symptom documentation in outpatient clinic letters and assessed the
level of agreement with parental information from a standardised questionnaire.
Materials and
methods
Study design
We used
data from the Swiss Paediatric Airway Cohort (SPAC), a national multicentre longitudinal
study of children evaluated in outpatient paediatric pulmonology clinics throughout
Switzerland (ClinicalTrials.gov identifier: NCT03505216) [19–22]. The SPAC study aims
to enrol all children
referred to the pulmonology clinics for respiratory problems such as wheezing,
coughing, dyspnoea and exercise-related symptoms. The SPAC study is
observational and embedded in routine medical care, and all diagnostic tests
are performed per clinical indication. Recruitment started in July 2017 and is
ongoing.
In
conjunction with SPAC study enrolment, parents complete a baseline
questionnaire, which collects data related to respiratory symptoms, medication
utilisation, environmental exposures and health behaviours at the time of
referral. On the first page of the standardised questionnaire,
written instructions encourage the parent(s) to involve the child in
questionnaire completion. The baseline questionnaire was modelled on questions developed
for the
International Study of Asthma and Allergies in Childhood (ISAAC) [23] and the Leicester
Respiratory Cohort (LRC)
[24], in conjunction with physician input.
The questions related to exercise-induced respiratory symptoms were developed de
novo by the authors (EP, CdJ, CK) and revised in conjunction with the Swiss
Paediatric Airway Cohort project collaborators, who are paediatric pulmonologists.
The SPAC baseline questionnaire was tested
among parents who provided comments related to construct and face validity, and
the questionnaire was adapted based on this feedback.
The
baseline questionnaire was completed by the parent either shortly before or
shortly after their child’s consultation with the paediatric pulmonologist and
enrolment in the SPAC study. Neither the child’s referring physician nor the
paediatric pulmonologist reviewed the questionnaire responses, which were
exclusively analysed by the SPAC research team. We also collected data from medical
records, including the reason for referral, diagnostic investigations, final
diagnosis, and prescribed treatment. All data was entered into a Research
Electronic Data Capture (REDCap) database [25].
Written informed consent was obtained at enrolment from parents and directly
from participants aged over 13 years. The SPAC study was approved by the Bern
Cantonal Ethics Committee (Kantonale Ethikkomission Bern 2016-02176) and the SPAC
study protocol was published [19]. A
separate protocol for this analysis of exercise-induced respiratory symptom
documentation was not independently published.
Inclusion criteria
We included
children aged 6–17 years who enrolled in the SPAC study between 1 July 2017 and
1 December 2019 and who had been primarily referred to the paediatric
pulmonology clinic for exercise-induced respiratory symptoms. We considered exercise-induced
respiratory symptoms to be the main reason for referral when the referral letter
or the first outpatient clinic letter listed exercise-induced respiratory symptoms
as the sole or main reason for specialist consultation.
Physician-documented
and parent-reported exercise-induced respiratory symptom data
We obtained
physician-documented exercise-induced respiratory symptom data from the outpatient
clinic letter that was transmitted to the referring physician. Physicians’
notes were individually reviewed by a SPAC investigator (EP), and relevant data
was manually extracted from the text. For any unclear physician notes, a second
reviewer (CdJ) independently examined the document, and the final extracted
data was based on agreement between the two reviewers. Extracted data included:
symptom(s) experienced by the child (e.g. wheezing, coughing, dyspnoea,
tingling in fingertips or lips); perceived symptom location (chest or throat);
respiratory phase in which symptoms occurred or were felt maximally
(inspiration or expiration); triggers of exercise-induced respiratory symptoms
(specific physical activities); timing of onset of exercise-induced respiratory
symptoms (during or after exercise); and use and effect of bronchodilator treatment
on exercise-induced respiratory symptoms (table 1). Parent-reported exercise-induced
respiratory symptom data was extracted from the baseline questionnaire (EP) (table
1).
Table 1Information extracted from the outpatient clinic letter (physician) and
standardised questionnaire (parent) to measure the level of agreement in
reporting of exercise-induced respiratory symptom characteristics. Total n = 193.
| Variable |
Physician documented exercise-induced
respiratory symptoms, extracted from outpatient clinic letter |
Question in Swiss Paediatric Airway Cohort
questionnaire |
| Any exercise-induced respiratory symptoms |
Does the child have any exercise-induced
symptoms? [ Yes | No | Not mentioned ] |
Does your child sometimes experience
breathing problems when exercising? [ Yes | No ] |
| Wheezing |
Does the child wheeze when exercising? [ Yes
| No | Not mentioned ] |
Which breathing problems does your child
experience when exercising? Wheezing or whistling breathing sounds [ Yes | No
] |
| Coughing |
Does the child cough when exercising? [ Yes |
No | Not mentioned ] |
Which breathing problems does your child
experience when exercising? Cough [ Yes | No ] |
| Dyspnoea |
Does the child experience dyspnoea, shortness
of breathing, difficulty breathing when exercising? [ Yes | No | Not
mentioned ] |
Which breathing problems does your child
experience when exercising? Dyspnoea or tightness [ Yes | No ] |
| Tingling in fingertips or lips |
Does the child experience a tingling feeling
in fingertips or lips while exercising? [ Yes | No | Not
mentioned ] |
Does your child sometimes experience a
sensation as if ants were creeping around the fingertips or lips while
exercising? [ Yes | No ] |
| Types of exercise-induced respiratory symptom
triggers |
Which of the following activities trigger
exercise-induced symptoms? [ Running | Bicycle riding | Intensive sport games
| Swimming | Cold weather sports | No exercise triggers specified ] |
In which of the following situations do the
breathing problems occur? [ Running short distances | Running middle
distances | Running longer distances | Biking | Sports games | Swimming ] |
| Location of dyspnoea |
Where are the exercise-induced symptoms felt
the strongest? [ Chest | Throat | Chest and throat | Not specified ] |
If dyspnoea or tightness, where is the
sensation felt the strongest? [ Chest | Throat | Everywhere (chest and
throat) ] |
| When are exercise-induced respiratory
symptoms worst |
In which respiratory phase are the
exercise-induced symptoms worst? [ During inspiration | During expiration | Equally
during inspiration and expiration | Not specified ] |
When are the breathing problems worst? [ During
inspiration | During expiration | Equally during inspiration and expiration ] |
| Onset of exercise-induced respiratory
symptoms |
When do the exercise-induced symptoms begin? [
During exercise | After exercise | Not specified ] |
When do the breathing problems begin? – When
your child, for example, runs a longer distance, then the breathing problems
normally begin: (Choose one) [ Straight away after the first steps | A few
minutes after beginning the exercise | After ending the exercise ] |
| Inhaled medications for exercise-induced
respiratory symptoms |
Has the child used any inhaled medication
before or during exercise? [ Yes | No | Not mentioned ] |
Has your child inhaled an asthma spray or
asthma powder for breathing problems occurring when exercising? [ Yes | No ] |
| Effect of inhaled medications |
If yes: How well does the medication help? [ Symptoms
disappear | Symptoms are reduced | No difference | Not mentioned ] |
If yes: How well does the medication help? (Choose
one): [ The breathing problems disappear | The breathing problems are reduced
| You almost feel no difference ] |
Medical diagnosis
associated with exercise-induced respiratory symptoms
The final diagnosis
assigned by the paediatric pulmonologist was extracted from the outpatient
clinic letter. We grouped diagnoses into five major categories consistent with
published literature: (1) asthma, (2) extrathoracic dysfunctional breathing (functional:
inducible laryngeal obstruction; structural: e.g. laryngomalacia,
tracheomalacia), (3) thoracic dysfunctional breathing (functional: exercise-induced
respiratory symptoms with hyperventilation, breathing pattern disorders), (4)
asthma plus dysfunctional breathing (for patients with co-existing diagnoses),
and (5) other diagnoses (e.g. insufficient fitness level, chronic cough or rare
pulmonary causes) [6, 8].
Statistical
analysis
We compared
proportions of physician-documented and parent-reported exercise-induced
respiratory symptoms using counts and percentages. We calculated the level of agreement
for specific characteristics among children where the characteristic was
mentioned in both the outpatient clinic letter and the parental questionnaire –
e.g. for onset of symptoms, we calculated agreement for whether symptoms
started during or after exercise if the clinic letter included information on the
timing of onset. Children for whom this characteristic was not mentioned in the
clinic letter were excluded from this analysis. We calculated kappa statistics
using Cohen’s kappa for dichotomous outcomes and Fleiss’ kappa for categorical
variables with more than two categories. The kappa was interpreted using Landis
and Koch’s criteria: 0.0–0.2 slight agreement, 0.21–0.40 fair agreement, 0.41–0.60
moderate agreement, 0.61–0.80 substantial agreement and 0.81–1.0 almost-perfect
to perfect agreement [26]. We also assessed
whether agreement in exercise-induced respiratory symptoms depended on who
filled in the baseline questionnaire (mother, father, child-assisted) using
kappa statistics. We used STATA version 14 for statistical analyses and the
analytical code is published as supplement 1 in the
appendix.
Results
Of the 1669
children who participated in the Swiss Paediatric Airway Cohort (SPAC) study within
the eligibility period, 193
(12%) met the inclusion criteria (table
2). The mean age was 12 years and 92 (48%) were girls. Most study
participants were seen in Lucerne (33%) followed by Zurich (25%), Basel (17%),
Aarau (12%), Bern (11%) and St. Gallen (2%). The final diagnosis from the paediatric
pulmonologist was asthma in 106 patients (55%), extrathoracic dysfunctional
breathing in 33 (overall 17%; functional in 30 [16%] and structural in 3 [1%]),
thoracic dysfunctional breathing in 21 (11%), asthma plus dysfunctional
breathing in 21 (11%) and other diagnoses in 12 (6%).
Table 2Characteristics of children referred to Swiss pulmonology outpatient clinics
for exercise-induced respiratory symptoms (n = 193). Counts and percentages are
in relation to the total sample of 193 children, unless otherwise indicated.
| Characteristic |
n (%) |
| Age at baseline visit in years, mean (SD) |
12 (3) |
| Female sex |
92 (48%) |
| BMI z-score, mean (SD) (n = 161) |
0.4 (1.1) |
| Overweight (BMI z-score >1) (n = 161) |
49 (25%) |
| Performs leisure-time sports* (n = 191) |
164 (86%) |
| Swiss nationality |
159 (82%) |
| Parental education (n = 185) |
Mother, tertiary** |
55 (30%) |
| Father, tertiary** |
75 (41%) |
| Current smoking (n = 190) |
Mother |
28 (15%) |
| Father |
34 (19%) |
| Respiratory
symptoms in past 12 months (parental questionnaire) (n
= 190) |
Wheezing |
105 (54%) |
| >3 attacks of wheezing |
58 (30%) |
| Any symptoms during exercise |
175 (94%) |
| Physician diagnosis |
Asthma |
106 (55%) |
| Extrathoracic dysfunctional breathing |
33 (17%) |
| Thoracic dysfunctional breathing |
21 (11%) |
| Asthma plus dysfunctional breathing |
21 (11%) |
| Other aetiology of exercise-induced respiratory
symptoms |
12 (6%) |
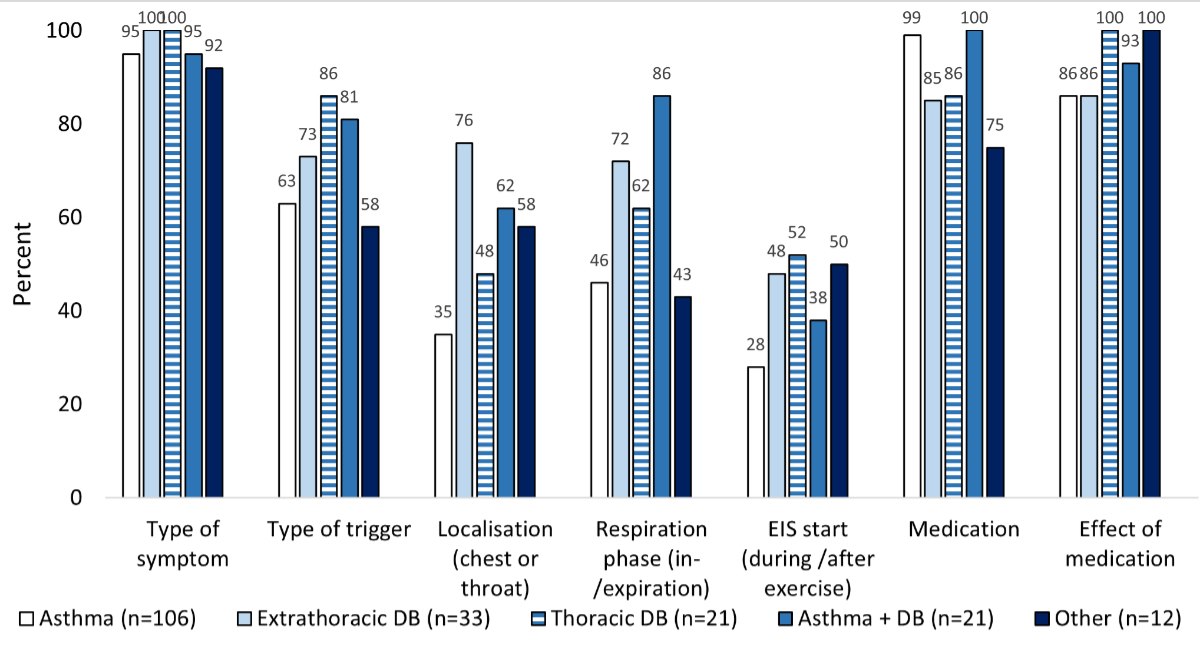
In the outpatient
clinic letter, the characteristics of exercise-induced respiratory symptoms were
documented in 186 (96%) of the 193 children. The type of symptom experienced
with exercise was almost always noted by physicians (96%), followed by triggering
physical activity (69%), perceived symptom location (48%), respiratory phase (45%)
and onset of exercise-induced respiratory symptoms relative to exercise (37%).
Bronchodilator use prior to paediatric pulmonology consultation was very
frequently documented in the outpatient clinic letter (94%), and the medication
effect was noted in 88% of the letters. Overall, characteristics of exercise-induced
respiratory symptoms were more often documented for children diagnosed with dysfunctional
breathing than for children diagnosed with asthma or other diagnoses (figure
1).
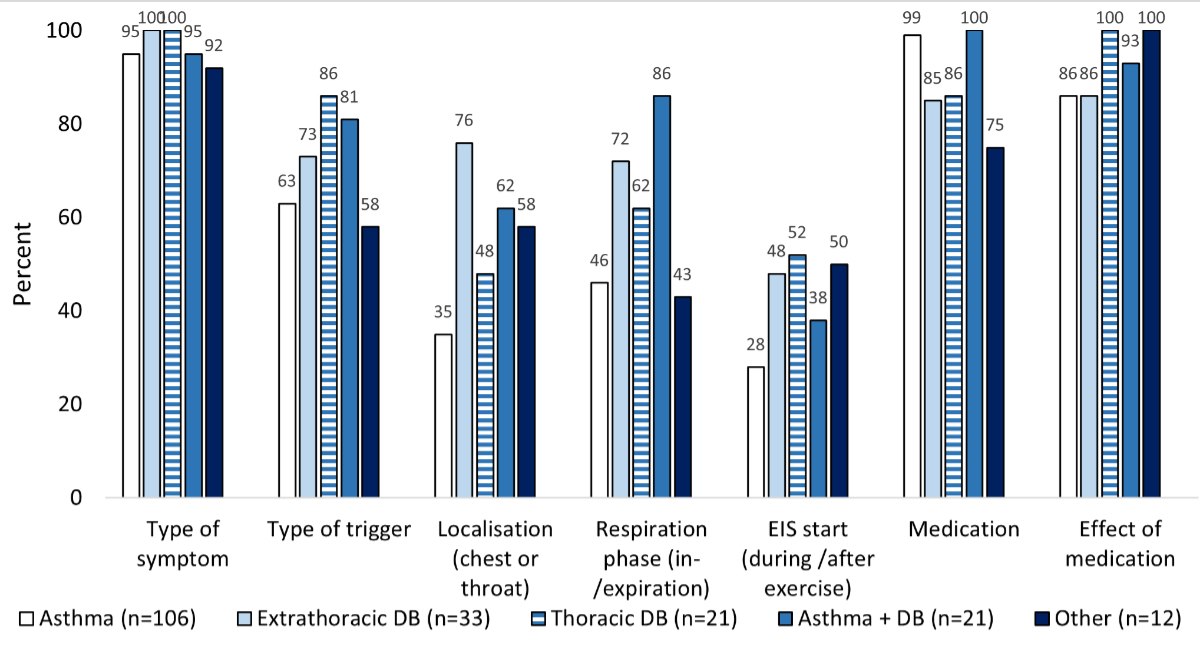
Figure 1Exercise-induced symptoms
documented by the physician in the outpatient clinic letter, by final diagnosis
(n = 193). Numbers displayed above each column indicate the exact percentage of
documentation of each exercise-induced respiratory symptom (EIS) in the
outpatient clinic letter. DB: dysfunctional breathing.
Parents
reported the type of respiratory symptom and triggering exercise more often than
physicians (table 3). The most frequent symptom, exercise-induced cough, was indicated
in 57% of parent-completed questionnaires versus 35% of clinic letters. Similarly,
tingling in fingers or lips – the rarest symptom to be noted – was reported
more often by parents (18%) than physicians (1%).
Table 3Level
of agreement between physician-documented and parent-reported exercise-induced
respiratory symptoms (n = 193). We analysed the level of agreement if the
characteristic in question was mentioned both in the physician’s outpatient
clinic letter and the parental questionnaire; thus characteristics that were
missing in both documents were excluded from this analysis. The n is provided
for each characteristic (out of the total 193 children).
|
Physician-documented
|
Parent-
reported |
Agreement
between physician-documented and parent-reported exercise-induced respiratory
symptoms |
Kappa |
|
|
Physician+
Parent+ |
Physician+
Parent– |
Physician–
Parent+ |
Physician–
Parent– |
|
| Symptom (n = 175) |
Wheezing or whistling sounds |
56 (32%) |
101 (58%) |
43 (25%) |
13 (7%) |
58 (33%) |
61 (35%) |
0.24 |
| Coughing |
61 (35%) |
100 (57%) |
52 (30%) |
9 (5%) |
48 (27%) |
66 (38%) |
0.39 |
| Dyspnoea |
114 (65%) |
146 (83%) |
101 (58%) |
13 (7%) |
45 (26%) |
16 (9%) |
0.17 |
| Tingling in fingers/lips |
2 (1%) |
31 (18%) |
2 (1%) |
0 |
29 (16%) |
145 (82%) |
0.09 |
| Type of exercise triggering exercise-induced
respiratory symptoms (n = 121) |
Running |
44 (36%) |
75 (62%) |
30 (25%) |
14 (12%) |
45 (37%) |
32 (26%) |
0.08 |
| Biking |
18 (15%) |
79 (65%) |
17 (14%) |
1 (1%) |
62 (51%) |
41 (34%) |
0.14 |
| Intensive sports |
81 (67%) |
94 (78%) |
63 (52%) |
18 (15%) |
31 (26%) |
9 (7%) |
0.01 |
| Swimming |
8 (7%) |
46 (38%) |
8 (7%) |
0 |
38 (31%) |
75 (62%) |
0.22 |
| Symptom location (n = 73) |
|
|
|
|
|
|
|
0.36 |
| Chest |
40 (55%) |
41 (56%) |
* |
|
|
|
|
| Throat |
26 (36%) |
12 (16%) |
|
|
|
|
|
| Chest and throat |
7 (10%) |
20 (27%) |
|
|
|
|
|
| Respiratory phase (n = 94) |
|
|
|
|
|
|
|
0.13 |
| Inspiration |
47 (50%) |
47 (50%) |
* |
|
|
|
|
| Expiration |
37 (39%) |
5 (5%) |
|
|
|
|
|
| Inspiration and expiration |
10 (11%) |
42 (45%) |
|
|
|
|
|
| Timing of exercise-induced respiratory
symptom onset (n = 66) |
|
|
|
|
|
|
|
0.19 |
| During exercise |
45 (68%) |
55 (83%) |
40 (61%) |
5 (8%) |
15 (23%) |
6 (9%) |
|
| After exercise |
21 (32%) |
11 (17%) |
6 (9%) |
15 (23%) |
5 (8%) |
40 (61%) |
|
| Prior use of bronchodilator for
exercise-induced respiratory symptoms (n = 159) |
|
|
|
|
|
|
|
0.53 |
| Yes |
99 (62%) |
111 (70%) |
88 (55%) |
11 (7%) |
23 (14%) |
37 (23%) |
|
| Effect of bronchodilator (n = 76) |
|
|
|
|
|
|
|
0.27 |
| Exercise-induced respiratory symptoms
disappear |
23 (30%) |
17 (22%) |
* |
|
|
|
|
| Exercise-induced respiratory symptoms reduce |
29 (38%) |
42 (55%) |
|
|
|
|
|
| No difference |
24 (32%) |
17 (22%) |
|
|
|
|
|
The highest
agreement between physicians and parents was found for recording bronchodilator
use (κ = 0.53). The agreement for type of symptom was best for cough (κ = 0.39)
and wheezing (κ = 0.24) and lowest for tingling in lips or fingers (κ = 0.09).
The agreement for exercise-induced respiratory symptom trigger was generally
poor across the different categories of exercise (κ = 0.01–0.14). Perceived location
of exercise-induced respiratory symptoms in the chest or throat (κ = 0.36) had
better agreement than respiratory phase of symptoms (κ = 0.13) and timing of exercise-induced
respiratory symptom onset (κ = 0.19). Agreement between physician-documented and
parent-reported exercise-induced respiratory symptoms differed for single items
depending on who filled in the questionnaire (mother, father, child-assisted),
but overall agreement was not better for one subgroup.
Discussion
This study is
the first to describe characteristics of documentation of exercise-induced
respiratory symptoms by paediatric pulmonologists among children enrolled in a
large paediatric respiratory cohort and referred primarily for exercise-induced
respiratory symptoms. Outpatient clinic letters usually included information
related to specific symptom(s) and bronchodilator use, but less often provided important
additional details such as perceived symptom location, respiratory phase and timing
of onset of exercise-induced respiratory symptoms. These characteristics of exercise-induced
respiratory symptoms have been described as important factors for
differentiating dysfunctional breathing from asthma and other aetiologies [3, 11,
27–29]; however this information was
documented in the outpatient clinic letter of less than half of the children.
There can
be several reasons why physicians documented fewer anamnestic details about exercise-induced
respiratory symptoms in the outpatient clinic letter compared to what parents conveyed
in the standardised questionnaire. Paediatric pulmonologists may have chosen to
document only the most important symptoms in the outpatient clinic report,
where succinct summarisation is an important consideration for both the writer
(treating physician) and reader (referring physician). It is also possible that
physicians verbally enquired about all exercise-induced respiratory symptom
domains but underreported negative responses in the outpatient clinic report. Another
explanation concerns different intrinsic characteristics of the data collection
tools. Whereas medical documentation is usually flexible and unique to each
physician, parental questionnaires relied on a standardised checklist of
specific symptoms and preformulated response choices. In addition, the doctor
may directly explain or display what is meant by the question, an advantage
which is not available in a standardised questionnaire and which can lead to
different answers.
Interestingly,
we observed consistent differences in the extent of exercise-induced
respiratory symptom documentation by physicians, depending on the final
diagnosis. When the final diagnosis was extrathoracic or thoracic dysfunctional
breathing, all exercise-induced respiratory symptom domains (type of symptom,
type of trigger, location, respiratory phase of symptom and timing of exercise-induced
respiratory symptoms) were more frequently documented in the outpatient clinic letter
than when the final diagnosis was asthma. We can speculate that since these
diagnoses are relatively rarer than asthma and are less likely to rely on
objective diagnostic tests, paediatric pulmonologists may have documented more symptom
characteristics to communicate differential diagnosis evaluation and clinical
decision-making to the referring physician.
Agreement on symptom reporting between
physicians and parents varied from poor to moderate. The absence of agreement for
specific exercise-induced
respiratory symptom characteristics was mainly due to parental reporting of
symptoms that were not mentioned in the physician letter; only in a few
instances did the outpatient clinic letter include symptoms that were not
reported in the parental questionnaire. Two studies that investigated agreement
between physician documentation and standardised parent reporting of paediatric
respiratory symptoms, but which were not specifically focused on exercise-induced
respiratory symptoms, similarly found a poor-to-fair agreement. A study using
population-based data from the Dutch Generation R study found that parents more
often reported wheezing than physicians (36% versus 20%, κ = 0.36), in line
with our results [30]. Additionally, the
WHISTLER Birth Cohort (1007 children, age 5 years) reported a κ = 0.07 for
recent wheezing and a κ = 0.12 for ever wheezing [31].
There are
small differences in how single data variables were characterised in the
outpatient clinic letter (physician) versus the parental questionnaire (table
1), most notably for the wording accompanying the timing of exercise-induced
respiratory symptom onset. It follows that the kappa agreement could have been
influenced by misclassification of extracted data on the part of the authors. Misclassification
may also have been introduced by parental interpretation of their child’s
symptoms while filling in the standardised questionnaire and selecting among
dichotomous response options (“Yes” or “No”). Respiratory symptoms,
particularly “wheezing”, can be difficult for parents to distinguish from physiological
“noisy breathing” that accompanies exercise [32].
However this misclassification could arguably have equally affected symptom
history noted by physicians, which was also based on parental reports. Missing
data from physician letters or parental questionnaires may have also affected
kappa agreement, with potential for either weaker or stronger results.
The analysis
of depersonalised health data from a coordinated data infrastructure will be
increasingly important for enhancing the understanding, management and
prevention of disease [16]. In
Switzerland, several projects within the Swiss Personalised Health Network aim
to standardise routine healthcare data and make it more readily available for
research [17, 18]. Enhanced symptom documentation
could improve the capacity for paediatric respiratory research by bolstering
the comprehensiveness of the Swiss data infrastructure. One way to accomplish
this would be through inclusion of a standardised checklist of exercise-induced
respiratory symptom characteristics, to be jointly completed by parents and
patients, and stored in the coordinated data infrastructure. Our study suggests
that questionnaires remain a vital source of information in paediatric research
studies and can effectively complement physician documentation, particularly as
it pertains to detailed recording of symptom characteristics. Questionnaires
should be carefully validated with a diverse population to ensure correct
interpretation of terminology, for example what is meant by “wheezing”, and
generate reproducible data, thus minimising the risk of misinterpretation of
symptoms. Ideally, doctors should also review the questionnaire jointly with
the parent(s) and child before it is stored in the medical record to validate
the answers and further ensure the quality of health repository data. This
offers a solution that does not oblige paediatric pulmonologists to document exercise-induced
respiratory symptoms with lengthy symptom checklists or preformulated templates,
which would elongate and complicate outpatient clinic letters and likely not enhance
physician communication.
This study
is strengthened by the real-world, observational design of the Swiss Paediatric
Airway Cohort, the relatively large size of this cohort and the inclusion of
children from different paediatric respiratory outpatient clinics in
Switzerland. Another strength is the inclusion of children with exercise-induced
respiratory symptoms of different aetiologies, thus allowing a comprehensive
analysis of exercise-induced respiratory symptom documentation which includes
both asthma and rarer diagnoses. A limitation of this study is that it only
represents children referred to participating paediatric respiratory outpatient
clinics in the German-language region of Switzerland. We, however, do not have
reason to suspect that exercise-induced respiratory symptom documentation would
differ systematically in the other Swiss regions.
Conclusion
Characteristics
of paediatric exercise-induced respiratory symptoms are documented differently
by physicians and parents, with a generally low level of agreement when
comparing the outpatient physician letter with a standardised parent
questionnaire. Standardised, parent-completed questionnaires should be viewed
as an important complement to physician letters when considering the
comprehensiveness of the paediatric health data infrastructure. Since comprehensive
documentation of paediatric respiratory symptoms is important when analysing
data exported from coordinated data infrastructures, a structured way of digitally
documenting symptoms could enhance the usability of routine healthcare data in future
paediatric exercise-induced respiratory symptom research
Data access
The dataset
supporting this analysis is not publicly available. The participants of this
study did not give written consent for their data to be published in an open
data repository. Upon reasonable request, the deidentified data that generated
the findings of this study may be shared by the corresponding author (CK).
Acknowledgments
We thank
the families who took part in the Swiss Paediatric Airway Cohort (SPAC) study;
the research assistants (Natalie Messerli, Gia Thu Ly, Labinata Gjokaj, Meret
Ryser, Malui Frei) for helping with data collection and data entry; PedNet Bern
for supporting data collection in Bern; and the members of the SPAC study team.
SPAC study team members include D. Mueller-Suter, P. Eng, B. Kern (Canton
Hospital Aarau, Aarau, Switzerland); U. Frey, J. Hammer, A. Jochmann, D.
Trachsel, A. Oettlin (University Children’s Hospital Basel, Basel,
Switzerland); P. Latzin, C. Casaulta, C. Abbas, M. Bullo, O. Fuchs, E.
Kieninger, I. Korten, L. Krüger, B. Seyfried, S. Yammine, C. de Jong
(University Children’s Hospital Bern, Bern, Switzerland); P. Iseli (Children’s
Hospital Chur, Chur, Switzerland); K. Hoyler (private paediatric pulmonologist,
Horgen, Switzerland); S. Blanchon, S. Guerin, I. Rochat (University Children’s
Hospital Lausanne, Lausanne, Switzerland); N. Regamey, M. Lurà, M. Hitzler, A.
Clavuot, K. Hrup, J. Stritt (Canton Hospital Lucerne, Lucerne, Switzerland); J.
Barben (Children’s Hospital St Gallen, St Gallen, Switzerland); O. Sutter
(private paediatric practice, Worb, Bern, Switzerland); A. Moeller, A. Hector,
K. Heschl, A. Jung, T. Schürmann, L. Thanikkel, J. Usemann (University Children’s
Hospital Zurich, Zurich, Switzerland); C.E. Kuehni, C. Ardura-Garcia, S. Glick,
D. Berger, T. Krasnova, R. Makhoul, M. Ganbat, B. Guerra Buezo, F. Romero, M.C.
Mallet, E.S.L. Pedersen, M. Goutaki (University of Bern, Institute of Social
and Preventive Medicine, Bern, Switzerland).
Claudia E. Kuehni
Institute
of Social and Preventive Medicine
University
of Bern
Mittelstrasse 43
CH-3012 Bern
claudia.kuehni[at]unibe.ch
References
1. Johansson H, Norlander K, Malinovschi A. Increased prevalence of exercise-induced
airway symptoms - A five-year follow-up from adolescence to young adulthood. Respir
Med. 2019;154:76–81. doi: https://doi.org/10.1016/j.rmed.2019.06.011
2. Kenn K, Hess MM. Vocal cord dysfunction: an important differential diagnosis of bronchial
asthma. Dtsch Arztebl Int. 2008 Oct;105(41):699–704.
3. Røksund OD, Heimdal JH, Clemm H, Vollsæter M, Halvorsen T. Exercise inducible laryngeal
obstruction: diagnostics and management. Paediatr Respir Rev. 2017 Jan;21:86–94.
4. Røksund OD, Heimdal JH, Olofsson J, Maat RC, Halvorsen T. Larynx during exercise:
the unexplored bottleneck of the airways. Eur Arch Otorhinolaryngol. 2015 Sep;272(9):2101–9.
doi: https://doi.org/10.1007/s00405-014-3159-3
5. Abu-Hasan M, Tannous B, Weinberger M. Exercise-induced dyspnea in children and adolescents:
if not asthma then what? Ann Allergy Asthma Immunol. 2005 Mar;94(3):366–71. doi: https://doi.org/10.1016/S1081-1206(10)60989-1
6. Barker N, Everard ML. Getting to grips with ‘dysfunctional breathing’. Paediatr Respir
Rev. 2015 Jan;16(1):53–61.
7. Depiazzi J, Everard ML. Dysfunctional breathing and reaching one’s physiological limit
as causes of exercise-induced dyspnoea. Breathe (Sheff). 2016 Jun;12(2):120–9. doi: https://doi.org/10.1183/20734735.007216
8. Pedersen ES, Ardura-Garcia C, de Jong CC, Jochmann A, Moeller A, Mueller-Suter D,
et al. Diagnosis in children with exercise-induced respiratory symptoms: A multi-center
study. Pediatr Pulmonol. 2021 Jan;56(1):217–25. doi: https://doi.org/10.1002/ppul.25126
9. Olin JT. Exercise-Induced Laryngeal Obstruction: When Pediatric Exertional Dyspnea
Does not Respond to Bronchodilators. Front Pediatr. 2019 Mar;7:52. doi: https://doi.org/10.3389/fped.2019.00052
10. Liyanagedera S, McLeod R, Elhassan HA. Exercise induced laryngeal obstruction: a review
of diagnosis and management. Eur Arch Otorhinolaryngol. 2017 Apr;274(4):1781–9. doi: https://doi.org/10.1007/s00405-016-4338-1
11. Pedersen ES, de Jong CC, Ardura-Garcia C, Mallet MC, Barben J, Casaulta C, et al. Reported
Symptoms Differentiate Diagnoses in Children with Exercise-Induced Respiratory Problems:
Findings from the Swiss Paediatric Airway Cohort (SPAC). J Allergy Clin Immunol Pract.
2021 Feb;9(2):881–889.e3. doi: https://doi.org/10.1016/j.jaip.2020.09.012
12. Niggemann B, Evers M, Härtl M. Psychogenic and functional disorders of the respiratory
tract in children and adolescents—a pilot study. Pediatr Allergy Immunol. 2012 Sep;23(6):605–6.
doi: https://doi.org/10.1111/j.1399-3038.2012.01295.x
13. de Groot EP, Duiverman EJ, Brand PL. Dysfunctional breathing in children with asthma:
a rare but relevant comorbidity. Eur Respir J. 2013 May;41(5):1068–73. doi: https://doi.org/10.1183/09031936.00130212
14. Grüber C, Lehmann C, Weiss C, Niggemann B. Somatoform respiratory disorders in children
and adolescents-proposals for a practical approach to definition and classification.
Pediatr Pulmonol. 2012 Feb;47(2):199–205. doi: https://doi.org/10.1002/ppul.21533
15. Martani A, Geneviève LD, Wangmo T, Maurer J, Crameri K, Erard F, et al. Sensing the
(digital) pulse. Future steps for improving the secondary use of data for research
in Switzerland. Digit Health. 2023 Apr;9:20552076231169826. 10.1177/20552076231169826
16. Geneviève LD, Martani A, Mallet MC, Wangmo T, Elger BS. Factors influencing harmonized
health data collection, sharing and linkage in Denmark and Switzerland: A systematic
review. PLoS One. 2019 Dec;14(12):e0226015. doi: https://doi.org/10.1371/journal.pone.0226015
17. Rakic M, Jaboyedoff M, Bachmann S, Berger C, Diezi M, do Canto P, et al. Clinical
data for paediatric research: the Swiss approach : Proceedings of the National Symposium
in Bern, Switzerland, Dec 5-6, 2019. BMC Proc. 2021 Sep 20;15 (Suppl 13):19. 10.1186/s12919-021-00226-3
18. Jaboyedoff M, Rakic M, Bachmann S, Berger C, Diezi M, Fuchs O, et al. SwissPedData:
standardising hospital records for the benefit of paediatric research. Swiss Med Wkly.
2021 Dec;151(5152):w30069. 10.4414/SMW.2021.w30069
19. Pedersen ES, de Jong CC, Ardura-Garcia C, Barben J, Casaulta C, Frey U, et al. The
Swiss Paediatric Airway Cohort (SPAC). ERJ Open Res. 2018 Nov;4(4):00050–02018. 10.1183/23120541.00050-2018
20. de Jong CC, Ardura-Garcia C, Pedersen ES, Mallet MC, Mueller-Suter D, Jochmann A,
et al. Standardization of Reporting Obstructive Airway Disease in Children: A National
Delphi Process. J Allergy Clin Immunol Pract. 2023 Jan;11(1):187–194.e6. doi: https://doi.org/10.1016/j.jaip.2022.08.050
21. Ardura-Garcia C, Mallet MC, Berger DO, Hoyler K, Jochmann A, Kuhn A, et al.; SPAC
Study Team. Predictors of asthma control differ from predictors of asthma attacks
in children: The Swiss Paediatric Airway Cohort. Clin Exp Allergy. 2023 Nov;53(11):1177–86.
doi: https://doi.org/10.1111/cea.14390
22. de Jong CC, Pedersen ES, Mozun R, Müller-Suter D, Jochmann A, Singer F, et al. Diagnosis
of asthma in children: findings from the Swiss Paediatric Airway Cohort. Eur Respir
J. 2020 Nov;56(5):2000132. doi: https://doi.org/10.1183/13993003.00132-2020
23. Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, et al. International
Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir
J. 1995 Mar;8(3):483–91. doi: https://doi.org/10.1183/09031936.95.08030483
24. Kuehni CE, Brooke AM, Strippoli MP, Spycher BD, Davis A, Silverman M. Cohort profile:
the Leicester respiratory cohorts. Int J Epidemiol. 2007 Oct;36(5):977–85. doi: https://doi.org/10.1093/ije/dym090
25. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic
data capture (REDCap)—a metadata-driven methodology and workflow process for providing
translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377–81.
doi: https://doi.org/10.1016/j.jbi.2008.08.010
26. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics.
1977 Mar;33(1):159–74. doi: https://doi.org/10.2307/2529310
27. Smoliga JM, Mohseni ZS, Berwager JD, Hegedus EJ. Common causes of dyspnoea in athletes:
a practical approach for diagnosis and management. Breathe (Sheff). 2016 Jun;12(2):e22–37.
doi: https://doi.org/10.1183/20734735.006416
28. Tilles SA, Ayars AG, Picciano JF, Altman K. Exercise-induced vocal cord dysfunction
and exercise-induced laryngomalacia in children and adolescents: the same clinical
syndrome? Ann Allergy Asthma Immunol. 2013 Nov;111(5):342–346.e1. doi: https://doi.org/10.1016/j.anai.2013.07.025
29. Vollsæter M, Stensrud T, Maat R, Halvorsen T, Røksund OD, Sandnes A, et al. Exercise
Related Respiratory Problems in the Young-Is It Exercise-Induced Bronchoconstriction
or Laryngeal Obstruction? Front Pediatr. 2022 Jan;9:800073. doi: https://doi.org/10.3389/fped.2021.800073
30. Mohangoo AD, de Koning HJ, Hafkamp-de Groen E, van der Wouden JC, Jaddoe VW, Moll HA,
et al. A comparison of parent-reported wheezing or shortness of breath among infants
as assessed by questionnaire and physician-interview: The Generation R study. Pediatr
Pulmonol. 2010 May;45(5):500–7. doi: https://doi.org/10.1002/ppul.21208
31. Korsten K, Naaktgeboren CA, Bont LJ, van der Ent CK, de Hoog ML. Defining asthma in
children: how well do parents, doctors and spirometry agree? ERJ Open Res. 2020 Oct;6(4):00348–02019.
doi: https://doi.org/10.1183/23120541.00348-2019
32. Shanmugam S, Nathan AM, Zaki R, Tan KE, Eg KP, Thavagnanam S, et al. Parents are poor
at labelling wheeze in children: a cross-sectional study. BMC Pediatr. 2016 Jun;16(1):80.
doi: https://doi.org/10.1186/s12887-016-0616-8
Appendix
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.3939.