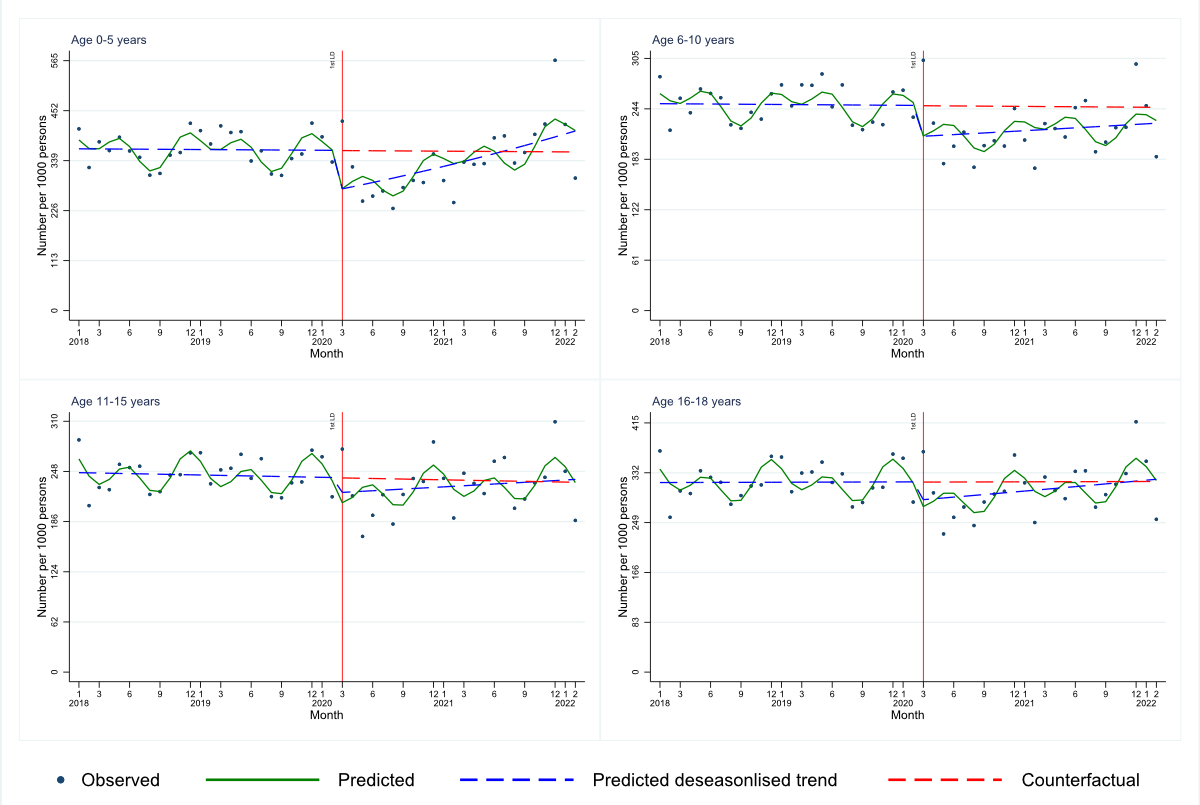
Figure 1Interrupted time series for consultations by age categories (TARMED position: 00.0010).
DOI: https://doi.org/https://doi.org/10.57187/s.3899
The World Health Organization (WHO) officially declared COVID-19 a pandemic on 11 March 2020. Up to March 2023, 760,360,956 COVID-19 cases were confirmed worldwide, including 6,873,477 deaths [1], with a higher risk for severe outcomes in people with particular pre-existing conditions [2] and in the elderly [3]. COVID-related mortality and morbidity were much lower in children and adolescents [4, 5] and this age group was therefore not considered a risk group. However, indirect effects of the pandemic and the measures introduced to curb the local epidemics might (have) impact(ed) young people’s health in the short and long term [5].
Declines, delays or interruptions in the coverage of vaccines during the pandemic were found worldwide [6]. The WHO estimated that 25 million children aged below one year did not receive basic vaccines in 2021 [7]. Further studies found lower levels of utilisation of well-child visits and/or ambulatory paediatric health services more generally in the pandemic phase than in the pre-pandemic phase (e.g. [8–14]). Despite this generally lower utilisation of paediatric health services in the pandemic, some studies also indicate that outpatient visits only fell markedly for some health conditions (e.g. infectious diseases, such as respiratory tract infection or gastroenteritis), but not (as markedly) for others (e.g. eczema, atopic dermatitis, diabetes) [11, 15, 16]. Furthermore, some studies have shown that an initial decrease in utilisation of primary paediatric health services was often followed by a certain recovery over the pandemic phase, at least for some primary health services [10, 16–18]. Lastly, the general pattern of lower utilisation during the pandemic did not seem to be confirmed for all health services. The utilisation of telemedicine consultations, for instance, increased when more stringent measures (e.g. lockdowns) were put in place [12, 18–20].
The following evidence gaps regarding changes in primary paediatric healthcare utilisation during the COVID-19 pandemic stand out. Firstly, most publications did not distinguish between different primary healthcare services, e.g. between well-child visits and primary urgent or regular consultations. Secondly, many studies did not use longitudinal analytical approaches. Such studies are limited because they cannot account for trends that already emerged in the pre-pandemic period (e.g. [21]) or trends across the pandemic phase. In terms of existing longitudinal research, there is a lack of studies that analysed data beyond the initial pandemic year. Therefore, analyses on how utilisation normalised over a longer time period are lacking. Lastly, relatively few Swiss studies have compared objective and representative data on pre-pandemic and pandemic utilisation of primary health services. Rather, existing studies often relied on self-reported data (e.g. [22]) or data that might have been affected by selection bias (e.g. [23]). We are only aware of one recent Swiss study that used objective health insurance data [24] – however this study focused solely on mental healthcare utilisation and therefore does not provide insights into other primary health services that are particularly relevant for paediatric populations (e.g. well-child visits).
Based on existing research gaps, we studied the pandemic’s effects on the utilisation of primary paediatric health services longitudinally using health insurance data. A horizon beyond the initial pandemic year was considered, comparing the 2-year period before the first lockdown in Switzerland (January 2018 – March 2020) with the pandemic period (March 2020 – March 2022) separately for different primary paediatric health services. Besides studying the main effect of the pandemic, pre-pandemic and pandemic trends were also addressed.
Prompted by a scenario of exponential epidemic development and an overburdened health system, the Swiss government introduced various public health measures to decrease the transmission of COVID-19. On 13 March 2020, all schools were closed and the provision of elective and non-urgent medical care was restricted for all health professions and levels of care, including paediatric healthcare. On 16 March, the most stringent measure – a national lockdown – was announced. The restriction on elective and non-urgent medical care as well as the lockdown lasted until 27 May 2020. However, even before the easing of the introduced measures, the Federal Office of Public Health (FOPH), the Federal Commission on Immunization and the Swiss Society of Paediatrics communicated an exception to the restriction on elective and non-urgent medical care for 0–2-year-olds. More specifically, parents were advised on 16 March 2020 that children aged up to 2 years should adhere to recommended well-child and vaccination visits. Furthermore, the vaccination schedules of 2021 and 2022 emphasised the importance of carrying out all recommended vaccinations in a timely manner despite the COVID-19 pandemic [25, 26].
Insurance data (i.e. TARMED positions [TARMED = tariff for outpatient medical services in Switzerland]) and billing codes for vaccinations (i.e. the Anatomical Therapeutical Chemical [ATC] classification) were used. SASIS AG receives these data from almost all Swiss health insurers. Consequently, the SASIS dataset covers 96% of the insured paediatric population in Switzerland at any given time point. For the current publication, SASIS data on the utilisation of specific paediatric health services were requested for the time period between January 2018 and March 2022 for the age group of 0–18-year-olds. The requested TARMED positions and ATC codes were provided per month and aggregated for the age groups 0–5, 6–10, 11–15 and 16–18 years. The data that we received from SASIS on 13 October 2022 did not include any information that could identify individuals. Hence, individual children could not be followed for the purpose of identifying repeat visits or changes from one type of visit to another. Approval from an Ethics Committee was not required for these secondary data analyses and no protocol was written for this publication project.
The following TARMED positions, which are mutually exclusive, were selected for the current publication (for more details, see appendix table S1):
Besides TARMED positions, basic vaccinations were included in the current paper – i.e. vaccinations that were officially recommended by the Federal Office of Public Health during the study period because of their relevance for the health of individuals and the population [25, 26, 28–30]. Vaccinations against diphtheria, tetanus, pertussis, polio, Haemophilus influenzae type b (Hib) infection, hepatitis B, measles, mumps, rubella and pneumococcus were considered. The following ATC codes were grouped together because of the polyvalent vaccines that are used in daily practice (details can be found in table S1 in the appendix):
Given that initial vaccination shots against the mentioned diseases should mainly occur within the first year of a child’s life, changes in vaccination rates were only analysed for 0–5-year-olds. The following two major changes in the vaccination schedules must be mentioned. Firstly, hepatitis B was recommended for 11–14-year-olds in 2018 [28], then recommended for the first year of life from 2019 onwards [29]. Secondly, the pneumococcus vaccination was recommended as a basic rather than a supplementary vaccination from 2019 onwards [29].
The age-specific average yearly permanent resident population of Switzerland (as reported by the Swiss Federal Statistical Office [SFSO]) was weighted by a factor of 0.96 to estimate the study population (i.e. insured individuals) since SASIS data represent 96% of all insured people. To determine the potential effects of the pandemic, an interrupted time-series (ITS) model with offset (number of insured individuals) allowing for overdispersion and adjusting for seasonality by including two Fourier terms was used. The models include a time effect (changes in the pre-pandemic phase), a pandemic effect (pre-pandemic versus pandemic period) and an interaction effect (time × pandemic) that assesses changes in the trend between the pre-pandemic and the pandemic period. The month in which the first lockdown began (March 2020) was chosen as the indicator month discriminating between pre-pandemic and pandemic periods. Incident rate ratios (IRR) with corresponding 95% confidence interval (CI) are reported. Graphical representations of interrupted time-series analyses show the predicted trend over the observation period (green line), a deseasonalised trend (blue line) – allowing for a better assessment of pandemic effects – and a counterfactual trend (i.e. the trajectory if the pre-pandemic trend had continued over the entire observation period; red line). Statistical significance was set at p <0.05. All analyses were conducted using Stata 17.0 [31]. The Stata package circular was used to establish the Fourier terms.
Table 1 presents details on average yearly insured subjects.
Table 1Average yearly insured subjects by age, SASIS.
| Estimated number of insured subjects | ||
| Age group | Number | Percent |
| 0–5 years | 505,623 | 32.1% |
| 6–10 years | 419,825 | 26.7% |
| 11–15 years | 407,171 | 25.9% |
| 16–18 years | 241,738 | 15.4% |
| Total | 1,574,357 | 100.0% |
Table 2 summarises the findings regarding pandemic effects as well as pre-pandemic and pandemic trends for regular and urgent consultations, well-child visits and telephone consultations. The average use of consultations, well-child visits and urgent visits/consultations was statistically significantly lower in the pandemic compared to the pre-pandemic phase in 0–5-year-olds. These level differences were due to an initial drop in utilisation after the lockdown. Subsequently, utilisation increased again over the pandemic phase, as indicated by statistically significant interaction terms (time × pandemic). This pattern is also illustrated in figure 1 for regular consultations and in the supplementary material for well-child-visits (appendix figure S1) and urgent visits/consultations (appendix figure S2). Regarding consultations and urgent visits/consultations, a decreased average utilisation in the pandemic phase compared to the pre-pandemic phase was also observed for 6–10-year-olds. However, in this age group, the interaction terms were not statistically significant, indicating that no or only a very slow recovery occurred over the pandemic phase (figure 1 and figure S2 in the appendix). No statistically significant findings were found for 11–15- or 16–18-year-olds for these health services. In terms of telephone consultations, a statistically significant increased average utilisation in the pandemic compared to the pre-pandemic phase was found for all age groups (figure 2). While the utilisation remained at a heightened level in 0–5- and 11–15-year-olds, it decreased again after an initial rise in 6–10- and 16–18-year-olds as indicated by statistically significant interaction terms.
Table 2Model estimates derived from interrupted time series for paediatric health services. Interrupted time-series Poisson regression allowing for overdispersion, adjusted for seasonality. Coefficients are Incident Rate Ratios (IRR). 95% confidence interval in brackets.
| Age groups | |||||
| 0–5 years | 6–10 years | 11–15 years | 16–18 years | ||
| Consultations | Time | 1.000 (0.993–1.007) | 1.000 (0.994–1.006) | 0.999 (0.993–1.005) | 1.000 (0.995–1.006) |
| Pandemic | 0.760** (0.644–0.896) | 0.850* (0.742–0.974) | 0.925 (0.815–1.049) | 0.906 (0.802–1.024) | |
| Time × Pandemic | 1.017** (1.007–1.028) | 1.003 (0.994–1.013) | 1.004 (0.996–1.012) | 1.005 (0.997–1.013) | |
| Well-child visits up to 5 years | Time | 1.001 (0.995–1.006) | – | – | – |
| Pandemic | 0.871* (0.765–0.992) | ||||
| Time × Pandemic | 1.009* (1.000–1.018) | ||||
| Urgent visits/consultations | Time | 1.002 (0.992–1.013) | 1.000 (0.991–1.008) | 0.997 (0.991–1.004) | 0.997 (0.991–1.004) |
| Pandemic | 0.638*** (0.500–0.813) | 0.810* (0.665–0.985) | 0.951 (0.819–1.103) | 0.913 (0.783–1.064) | |
| Time × Pandemic | 1.023** (1.008–1.040) | 1.002 (0.989–1.015) | 0.997 (0.987–1.007) | 1.001 (0.991–1.011) | |
| Telephone consultations | Time | 1.002 (0.995–1.008) | 1.003 (0.997–1.008) | 1.001 (0.996–1.006) | 1.004 (0.998–1.010) |
| Pandemic | 1.394*** (1.218–1.594) | 1.547*** (1.387–1.726) | 1.578*** (1.430–1.741) | 1.831*** (1.614–2.076) | |
| Time × Pandemic | 1.002 (0.993–1.011) | 0.989** (0.982–0.996) | 0.995 (0.989–1.002) | 0.988** (0.979–0.996) | |
* p <0.05, ** p <0.01, *** p <0.001; interpretation of the different estimates:
(1) Time: Statistically significant estimate <1.0 → utilisation rates decreased in the pre-pandemic period. Statistically significant estimate >1.0 → utilisation increased over the pre-pandemic period. Estimate = 1.0 → utilisation did not change in the pre-pandemic phase.
(2) Pandemic: Statistically significant estimate <1.0 → average utilisation rate was lower in the pandemic than in the pre-pandemic period. Statistically significant estimate >1.0 → average rates were higher in the pandemic vs pre-pandemic period. Estimate = 1.0 → average rates did not differ between the pandemic and pre-pandemic periods.
(3) Time × pandemic: A significant interaction term indicates that the trend in the pandemic period differs from the one in the pre-pandemic phase. Statistically significant estimate >1.0 → utilisation rates increased again in the pandemic period. Statistically significant estimate <1.0 → decrease in the utilisation rates in the pandemic period. Estimate = 1.0 → utilisation remained similar in the pandemic period.
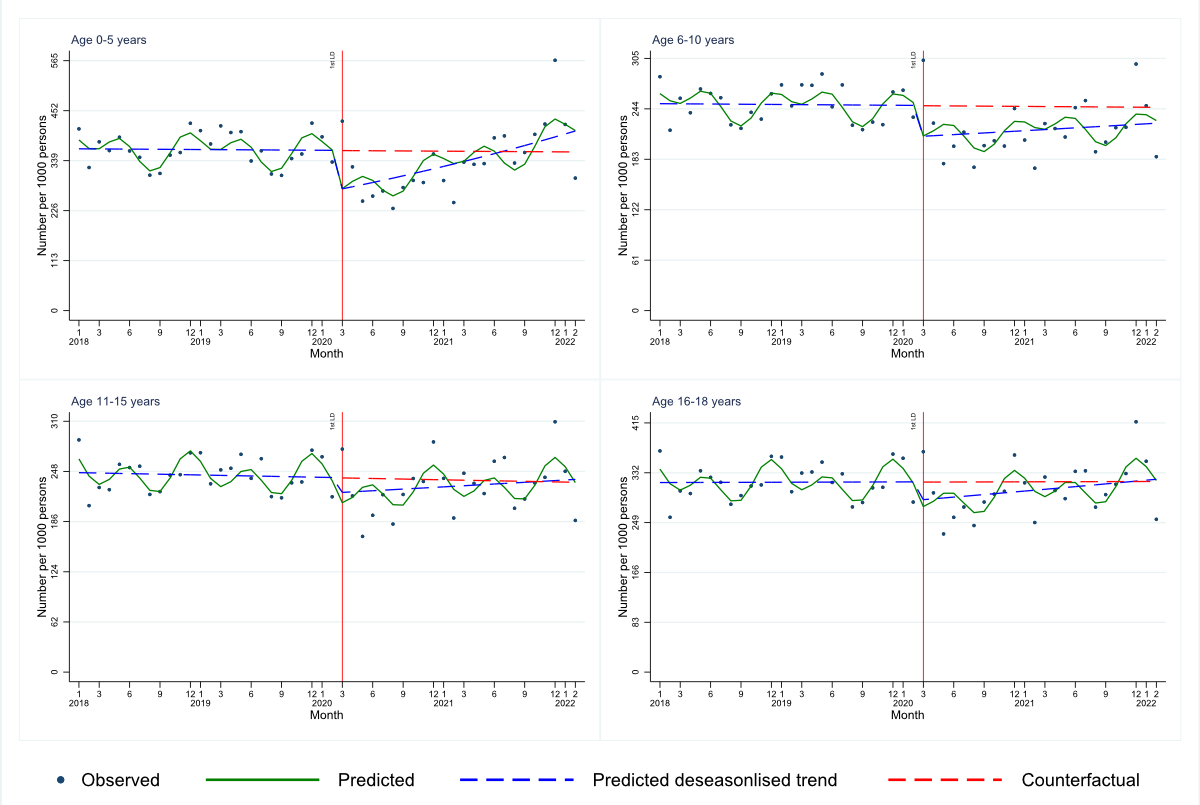
Figure 1Interrupted time series for consultations by age categories (TARMED position: 00.0010).
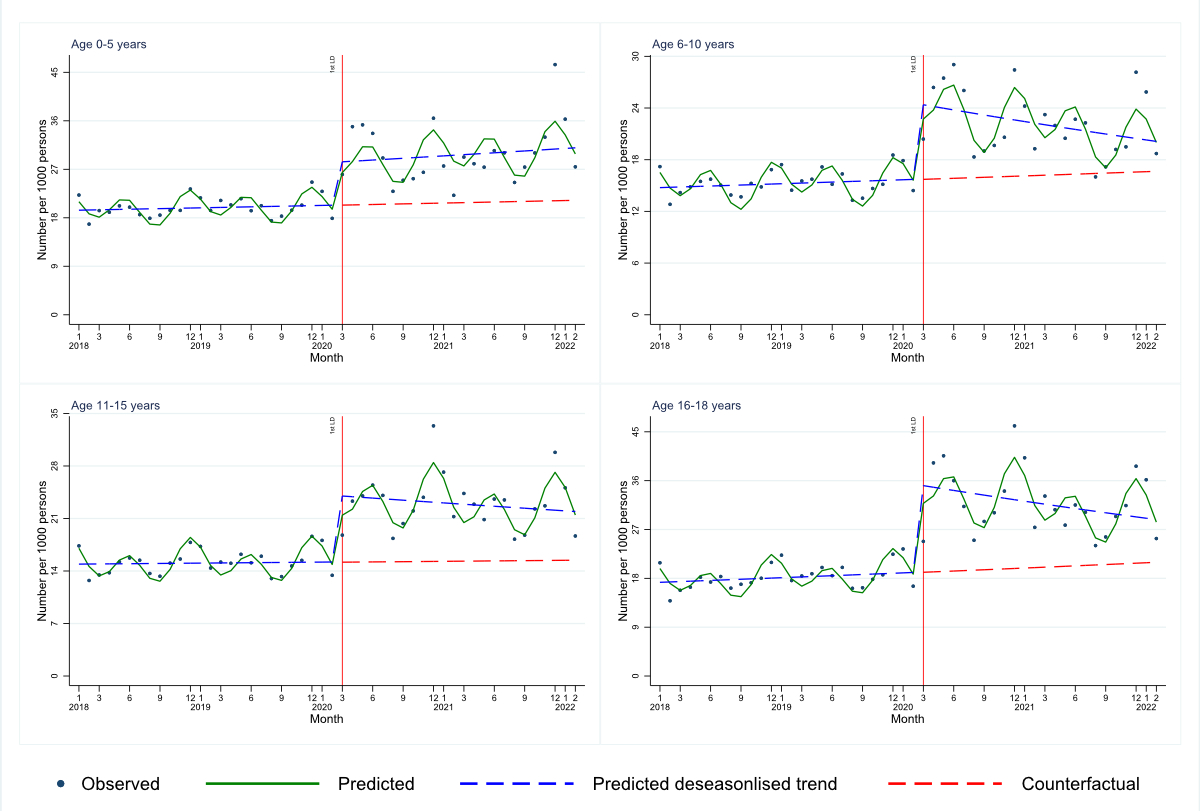
Figure 2Interrupted time series for telephone consultations by age categories (TARMED position: 00.0110).
The MMR vaccination rate changed over the observation period (see table 3): It increased during the pre-pandemic period, was – on average – statistically significantly lower in the pandemic compared to the pre-pandemic period and further decreased during the pandemic phase. Vaccination rates against diphtheria / tetanus / pertussis / polio / Hib infection / hepatitis statistically significantly decreased in the pre-pandemic phase, but were not affected by the pandemic or during the pandemic period. No statistically significant results were found regarding vaccinations against pneumococcus. The results regarding vaccinations are also illustrated in figures S3–S5 (in the appendix).
Table 3Model estimates derived from interrupted time series for basic vaccinations in 0–5-year-olds. Interrupted time-series Poisson regression allowing for overdispersion, adjusted for seasonality. Coefficients are Incident Rate Ratios (IRR). 95% confidence intervals in brackets.
| Vaccination against… | 0–5 years | |
| …measles/mumps/rubella | Time | 1.011** (1.004–1.017) |
| Pandemic | 0.841* (0.729–0.971) | |
| Time × Pandemic | 0.988* (0.977–0.998) | |
| …diphtheria / tetanus / pertussis / polio / Haemophilus influenzae type b infection / hepatitis | Time | 0.993* (0.987–0.999) |
| Pandemic | 0.972 (0.848–1.112) | |
| Time × Pandemic | 1.003 (0.994–1.013) | |
| …pneumococcus | Time | 1.002 (0.996–1.007) |
| Pandemic | 1.002 (0.887–1.132) | |
| Time × Pandemic | 1.001 (0.992–1.009) |
* p <0.05, ** p <0.01, *** p <0.001; interpretation of the different estimates:
(1) Time: Statistically significant estimate <1.0 → utilisation rates decreased in the pre-pandemic period. Statistically significant estimate >1.0 → utilisation increased over the pre-pandemic period. Estimate = 1.0 → utilisation did not change in the pre-pandemic phase.
(2) Pandemic: Statistically significant estimate <1.0 → average utilisation rate was lower in the pandemic than in the pre-pandemic period. Statistically significant estimate >1.0 → average rates were higher in the pandemic vs pre-pandemic period. Estimate = 1.0 → average rates did not differ between the pandemic and pre-pandemic periods.
(3) Time × pandemic: A significant interaction term indicates that the trend in the pandemic period differs from the one in the pre-pandemic phase. Statistically significant estimate >1.0 → utilisation rates increased again in the pandemic period. Statistically significant estimate <1.0 → decrease in the utilisation rates in the pandemic period. Estimate = 1.0 → utilisation remained similar in the pandemic period.
Our study provides new insights because – in contrast to most previous research – it considered a time frame beyond the initial COVID-19 pandemic year and applied longitudinal analytical methods. This allowed us to uncover potential normalisation processes over the pandemic period. Furthermore, the detailed analytical approach allowed us to identify diverging patterns for different paediatric health services and for different age groups.
Our analyses indicate that the utilisation of some primary paediatric health services was statistically significantly affected by the COVID-19 pandemic in Switzerland. In line with previous international research (e.g. [8–14]), a decreased average utilisation in the pandemic compared to the pre-pandemic phase was found for well-child visits among 0–5-year-olds (analyses were limited to this age group) as well as for regular and urgent visits/consultations among 0–5-year- and 6–10-year-olds. Furthermore, the present study found decreased MMR vaccination rates during the pandemic vs the pre-pandemic period in 0–5-year-olds, which corresponds to the pattern of declined, delayed or interrupted vaccinations that was described worldwide [6]. Lastly, our study yielded higher average utilisation rates regarding telephone consultations during the pandemic compared to the pre-pandemic phase in all age groups, confirming previous research [12, 18–20, 32].
In our study, the reduced average rates of well-child visits during the pandemic were not due to a change in need for such services, because the paediatric indication for well-child visits at specific time points in a child’s life are preventive in nature. Missed or delayed well-child visits are problematic because they are important for early detection of certain abnormalities in the child’s development [33] and are associated with some favourable outcomes, including better parenting skills, improved prevention of accidents and better language development of the child [33, 34]. Parents might have viewed well-child visits as less relevant in view of the overall health crisis and possibly were reluctant to seek preventive care for their child due to concerns about being exposed to the virus in the paediatrician’s practice [35]. Furthermore, communications by paediatric associations and the Federal Office of Public Health about the importance of attending preventive visits might not have reached parents initially.
However, because the rates of well-child visits increased again over the pandemic phase, it is possible that some of the visits were caught up. Figure S1 (in the appendix) shows that rates of well-child visits exceeded the counterfactual estimates. This implies that catch-up visits started from mid-2021. An initial drop in well-child visits and later catch-up was seen in other studies too, but none could show a full recovery [16, 18], potentially due to the studied time frame being too short.
In contrast to well-child visits, reduced average utilisation of regular and urgent visits/consultations during the pandemic might have been partly caused by a decreased need for care. Accordingly, studies showed that certain infectious diseases known to be common reasons for visits to a paediatrician (e.g. infections with the respiratory syncytial virus) were reduced during the pandemic [36]. Reduced infection rates might have had a particularly strong effect on the health care utilisation of the youngest age group, as confirmed by our analyses, because very young children are more likely to be severely affected by these infectious diseases [37]. A decrease in accidents overall during the pandemic might also have contributed to a decreased need for urgent visits. Indirect evidence for this stems from research that was carried out in emergency department settings. One systematic review, for instance, showed that about half of the included studies mentioned a decline in trauma cases in the emergency department during the pandemic that might have been due to various implemented changes (e.g. cancellation of sporting events, closure of playgrounds) [38].
Besides a reduced need, the observed pandemic effect might also have been caused by parents’ delay in the decision to seek professional care due to fear of contracting COVID-19 in paediatricians’ practices [39]. Handling the child’s health issue without professional support may have worked out well for objectively mild health issues, whereas it may have worsened the child’s health status for objectively severe conditions. A simultaneous increase in urgent visits (in parallel to the decrease in the utilisation of regular consultations) could not be observed in our study. However, parents might have presented their child to the secondary or tertiary health system.
In the youngest age group (0–5-year-olds), utilisation of regular and urgent consultations increased again over the pandemic period and reached pre-pandemic rates in the fourth quarter of 2021. In contrast, no statistically significant recovery emerged for 6–10-year-olds. The fact that a statistically significant normalisation of the utilisation pattern was limited to the youngest age group might be due, at least partly, to parents’ and/or paediatricians’ higher need for a face-to-face visit when the child is still very young (due to the health issues of young children and due to parental insecurities in this regard).
It is likely that telephone consultations at least partly substituted face-to-face visits in the youngest age groups for which reduced in-person visits (regular and urgent) were found in the present study. Hence, telephone services might have allowed access to professional paediatric care to be maintained while introduced measures (e.g. physical distancing) were adhered to. In the youngest age group (0–5 years), the utilisation of telephone consultations remained at a high level over the pandemic phase, even though utilisation of face-to-face regular and urgent consultations increased again. Hence, the total utilisation of paediatric health services seemed to have increased in the pandemic phase in this age group. For 6–10-year-olds, a partial substitution of face-to-face by telephone consultations seemed to have been limited to the initial phase of the pandemic. Accordingly, utilisation rates for telephone consultations decreased again over the pandemic phase despite persistently reduced utilisation rates regarding regular and urgent consultations.
In contrast, average utilisation rates of telephone services increased statistically significantly in the pandemic in the two oldest groups (11–15 and 16–18 years). Given that the patterns of regular and urgent consultations were not statistically significantly affected by the pandemic, this increase in average telephone consultations implies an increased healthcare need in these age groups during the pandemic. Parents or adolescents might have been in need of reassurance and guidance from paediatricians (e.g. regarding potential COVID-19-infections). Alternatively, consultations might have been about emerging mental health difficulties which were more prevalent in older compared to younger children [40, 41].
Compared to other consultation types, the utilisation of telephone consultations remained at a high level in some age groups. This possibly indicates a reduced scepticism against and increased appreciation of such services. Accordingly, previous international research has shown that healthcare providers and families (parents and children/adolescents) generally reported high satisfaction and usability of such telephone services [32, 42, 43].
In our study, MMR vaccination rates increased in the pre-pandemic phase, which corresponds to findings from earlier studies from Switzerland showing increasing coverage of measles vaccinations [44, 45], decreasing measles incidences [44] and an interruption of endemic transmissions of measles since 2016 [46]. Due to this pre-pandemic trend, the drop in measles vaccinations and the resulting differences in average MMR vaccination rates in the pre-pandemic and the pandemic phase is particularly pronounced in our study. This is regrettable, since a considerable number of children were – and possibly still are – unprotected.
Missed vaccinations increase the likelihood of outbreaks, particularly since there was no indication of a recovery over the pandemic period. The current study only found reduced average vaccination rates during the pandemic for the routine MMR vaccination. This is in line with previous findings from Switzerland showing that the MMR vaccination is the most frequently postponed basic vaccination [47]. However, it must also be noted that our findings contradict a recent statement by the Federal Office of Public Health that the pandemic did not have a negative impact on routine vaccinations [23]. This discrepancy might be due to a potential selection bias in the study that the Federal Office of Public Health statement is based on, which might have led to an overestimation of the actual vaccination coverage. Furthermore, the discrepancy might have arisen due to the longer observation period in the mentioned study (up to December 2022) with the potential to detect normalisation processes that occurred after the end point of our study (March 2022).
Despite the advantages of the current study, the following limitations must be considered. Most importantly, SASIS data are aggregated and do not allow us to investigate utilisation by individual children. Thus, catch-up visits or an increased healthcare need in individuals could not be investigated. Similarly, no data were available about the diagnoses or health issues for which particular health services were utilised. Thus, we cannot evaluate the short-term gravity or long-term impact of the change in utilisation on the health of children. To gain a deeper understanding on the impacts of delayed or missed regular and urgent healthcare visits, it will be essential to consult further data, including data from hospitals. Furthermore, it is crucial to also monitor utilisation and health endpoints after the pandemic period. Lastly, we can only hypothesise why utilisation rates of some health services have (not) changed as an effect of the pandemic or over the pre-pandemic or pandemic period.
In conclusion, the analyses clearly showed an impact of the pandemic on the utilisation of paediatric health services and a slow recovery in Switzerland into the second year of the pandemic. Partly we saw age-dependent changes. The age group of 0–5-year-olds showed the strongest reduction of almost all consultation types early but also throughout the pandemic. Regarding this age group, it is of utmost importance to follow up children who might still not have caught up their well-child visits. Furthermore, efforts are needed to ensure timely catch-ups of MMR vaccinations.
Our analyses also indicated that the pandemic increased the relevance of telephone consultations in all age groups, a pattern that was potentially maintained beyond the pandemic. Despite the advantages of such services, Switzerland is not yet equipped to expand and provide a sustainable telemedicine service. Furthermore, the long-term benefits and drawbacks of telemedical services need to be evaluated further and separately for different services.
Our analyses show that for future pandemics or other health crises, it is important to monitor utilisation and other relevant health indicators. This ensures a timely assessment of the effects that, for instance, a shift in utilisation (e.g. from face-to-face to telephone consultations) or an underutilisation of health services might have on the health of children and adolescents. Furthermore, the results highlight that the communication by health authorities on the importance of adhering to certain recommendations might not be sufficient to bring about an immediate change in behaviour. Tailoring such messages more specifically to the target group (e.g. by addressing existing concerns) might make them more effective.
For contractual reasons, SASIS data cannot be publicly shared; however they can be requested from SASIS directly (contact via https://www.sasis.ch/).
We would like to thank Sibylle Juvalta for her support in revising the manuscript.
The PedCov Consortium consists of the ZHAW Institute of Public Health: Julia Dratva (Principal Investigator); Michelle Dey; Szilvia Altwicker-Hámori; Thomas Volken; Frank Wieber; University Children’s Hospital Zurich (KiSpi Zürich): Michelle Seiler (Principal Investigator); Michael von Rhein; Aziz Chaouch; Clinical partners: Gianluca Gualco, Paediatric Emergency Department, Institute of Paediatrics of Southern Switzerland, EOC, Bellinzona; Sergio Manzano, Department of Paediatric Emergency Medicine, Geneva Children’s Hospital, Geneva University Hospitals, and Faculty of Medicine, University of Geneva; and the Professional Association of Swiss Paediatricians in Private Practice (Kinderärzte Schweiz): Ursula Laasner; Marc Sidler.
The PedCov project was partly funded by the Swiss Federal Office of Public Health (FOPH) (https://www.bag.admin.ch/bag) (number: 142005474; Principal Investigators: JD, MS) and partly through institutional contributions of the ZHAW and University Children’s Hospital Zurich. The FOPH had no role in study design, data collection and analysis, the decision to publish or in the preparation of the manuscript.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. WHO. WHO Coronavirus (COVID-19) Dashboard. 2023. Available from: https://covid19.who.int/
2. Treskova-Schwarzbach M, Haas L, Reda S, Pilic A, Borodova A, Karimi K, et al. Pre-existing health conditions and severe COVID-19 outcomes: an umbrella review approach and meta-analysis of global evidence. BMC Med. 2021 Aug;19(1):212. doi: https://doi.org/10.1186/s12916-021-02058-6
3. Cohen JF, Korevaar DA, Matczak S, Chalumeau M, Allali S, Toubiana J. COVID-19-Related Fatalities and Intensive-Care-Unit Admissions by Age Groups in Europe: A Meta-Analysis. Front Med (Lausanne). 2021 Jan;7:560685. doi: https://doi.org/10.3389/fmed.2020.560685
4. Mehraeen E, Oliaei S, SeyedAlinaghi S, Karimi A, Mirzapour P, Afsahi AM, et al. COVID-19 in pediatrics: a systematic review of current knowledge and practice. IDDT. 2022 Aug;22(5):e290921196908.
5. Huss G, Magendie C, Pettoello-Mantovani M, Jaeger-Roman E. Implications of the COVID-19 Pandemic for Pediatric Primary Care Practice in Europe. J Pediatr. 2021 Jun;233:290–291.e2. doi: https://doi.org/10.1016/j.jpeds.2021.03.004
6. Locke J, Marinkovic A, Hamdy K, Balendra V, Sanyaolu A. Routine pediatric vaccinations during the COVID-19 pandemic: A review of the global impact. World J Virol. 2023 Dec;12(5):256–61. doi: https://doi.org/10.5501/wjv.v12.i5.256
7. Immunization coverage. WHO; Available from: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage
8. Lebrun-Harris LA, Sappenfield OR, Warren MD. Missed and delayed preventive health care visits among US children due to the COVID-19 pandemic. Public Health Rep. 2022;137(2):336–43. doi: https://doi.org/10.1177/00333549211061322
9. Vogel M, Beger C, Gausche R, Jurkutat A, Pfaeffle R, Körner A, et al. COVID-19 pandemic and families’ utilization of well-child clinics and pediatric practices attendance in Germany. BMC Res Notes. 2021 Apr;14(1):140. doi: https://doi.org/10.1186/s13104-021-05562-3
10. Siedner MJ, Kraemer JD, Meyer MJ, Harling G, Mngomezulu T, Gabela P, et al. Access to primary healthcare during lockdown measures for COVID-19 in rural South Africa: an interrupted time series analysis. BMJ Open. 2020 Oct;10(10):e043763. doi: https://doi.org/10.1136/bmjopen-2020-043763
11. Li H, Yu G, Duan H, Fu J, Shu Q. Changes in Children’s Healthcare Visits During Coronavirus Disease-2019 Pandemic in Hangzhou, China. J Pediatr. 2020/05/19 ed. 2020 Sep;224:146–9.
12. Brown CL, Montez K, Amati JB, Simeonsson K, Townsend JD, Orr CJ, et al. Impact of COVID-19 on pediatric primary care visits at four academic institutions in the Carolinas. Int J Environ Res Public Health. 2021 May;18(11):5734. doi: https://doi.org/10.3390/ijerph18115734
13. Thakkar PV, Scott Z, Hoffman M, Delarosa J, Hickerson J, Boutzoukas AE, et al. Impact of the COVID-19 Pandemic on Pediatric Preventive Health Care Among North Carolina Children Enrolled in Medicaid. J Pediatric Infect Dis Soc. 2023 Dec;12 Supplement_2:S14–9. doi: https://doi.org/10.1093/jpids/piad061
14. Evans A, Mahar AL, Deb B, Boblitz A, Brownell M, Guttmann A, et al. Gaps in childhood immunizations and preventive care visits during the COVID-19 pandemic: a population-based cohort study of children in Ontario and Manitoba, Canada, 2016-2021. Can J Public Health. 2023 Oct;114(5):774–86. doi: https://doi.org/10.17269/s41997-023-00797-y
15. Barschkett M, Koletzko B, Spiess CK. COVID-19 associated contact restrictions in Germany: marked decline in children’s outpatient visits for infectious diseases without increasing visits for mental health disorders. Children (Basel). 2021 Aug;8(9):728. doi: https://doi.org/10.3390/children8090728
16. Schweiberger K, Patel SY, Mehrotra A, Ray KN. Trends in Pediatric Primary Care Visits During the Coronavirus Disease of 2019 Pandemic. Acad Pediatr. 2021;21(8):1426–33. doi: https://doi.org/10.1016/j.acap.2021.04.031
17. Schmid-Küpke NK, Matysiak-Klose D, Siedler A, Felgendreff L, Wieler L, Thaiss HM, et al. Cancelled routine vaccination appointments due to COVID-19 pandemic in Germany. Vaccine X. 2021 Aug;8:100094. doi: https://doi.org/10.1016/j.jvacx.2021.100094
18. Macy ML, Huetteman P, Kan K. Changes in primary care visits in the 24 weeks after COVID-19 stay-at-home orders relative to the comparable time Period in 2019 in Metropolitan Chicago and Northern Illinois. J Prim Care Community Health. 2020;11:2150132720969557. doi: https://doi.org/10.1177/2150132720969557
19. Grossman Z, Chodick G, Reingold SM, Chapnick G, Ashkenazi S. The future of telemedicine visits after COVID-19: perceptions of primary care pediatricians. Isr J Health Policy Res. 2020 Oct;9(1):53. doi: https://doi.org/10.1186/s13584-020-00414-0
20. Taquechel K, Diwadkar AR, Sayed S, Dudley JW, Grundmeier RW, Kenyon CC, et al. Pediatric Asthma Health Care Utilization, Viral Testing, and Air Pollution Changes During the COVID-19 Pandemic. J Allergy Clin Immunol Pract. 2020;8(10):3378–3387.e11. doi: https://doi.org/10.1016/j.jaip.2020.07.057
21. Castrejon MM, Leal I, de Jesus Pereira Pinto T, Guzmán-Holst A. The impact of COVID-19 and catch-up strategies on routine childhood vaccine coverage trends in Latin America: A systematic literature review and database analysis. Hum Vaccin Immunother. 2022 Nov;18(6):2102353. doi: https://doi.org/10.1080/21645515.2022.2102353
22. Seiler M, Goldman RD, Staubli G, Hoeffe J, Gualco G, Manzano S; Swiss Medical Weekly. Parents’ intent to vaccinate against influenza during the COVID-19 pandemic im two regions in Switzerland. Swiss Med Wkly. 2021 May;151(1920):w20508. doi: https://doi.org/10.4414/smw.2021.20508
23. FOPH. Kantonales Durchimpfungsmonitoring Schweiz. Available from: https://www.bag.admin.ch/bag/de/home/gesund-leben/gesundheitsfoerderung-und-praevention/impfungen-prophylaxe/informationen-fachleute-gesundheitspersonal/durchimpfung.html
24. Rachamin Y, Jäger L, Schweighoffer R, Signorell A, Bähler C, Huber CA, et al. The Impact of COVID-19 on Mental Healthcare Utilization in Switzerland Was Strongest Among Young Females-Retrospective Study in 2018-2020. Int J Public Health. 2023 May;68:1605839. doi: https://doi.org/10.3389/ijph.2023.1605839
25. Schweizerischer Impfplan 2022. Richtlinien und Empfehlungen. Bundesamt für Gesundheit und Eidgenössische Kommission für Impffragen; 2022.
26. Schweizerischer Impfplan 2021. Richtlinien und Empfehlungen. Bundesamt für Gesundheit und Eidgenössische Kommission für Impffragen; 2021.
27. Ambühl D, Bächler A, Baumann T, Jenni O, Leuchter Ha-Vinh R, Lips U, et al. Checklisten für die Vorsorgeuntersuchungen nach den Empfehlungen der Schweizerischen Gesellschaft für Pädiatrie. Arbeitsgruppe der SGP; 2012.
28. Schweizerischer Impfplan 2018. Richtlinien und Empfehlungen. Bundesamt für Gesundheit und Eidgenössische Kommission für Impffragen; 2018.
29. Schweizerischer Impfplan 2019. Richtlinien und Empfehlungen. Bundesamt für Gesundheit und Eidgenössische Kommission für Impffragen; 2019.
30. Schweizerischer Impfplan 2020. Richtlinien und Empfehlungen. Bundesamt für Gesundheit und Eidgenössische Kommission für Impffragen; 2020.
31. StataCorp. Stata Statistical Software: Release 17.0. College Station (TX): StataCorp LLC; 2021.
32. Kirkland DA, Svynarenko R, Lindley LC. Scoping Review: Telehealth During the Coronavirus Disease 2019 Pandemic for Pediatric Populations. J Nurse Pract. 2024 Feb;20(2):104884. doi: https://doi.org/10.1016/j.nurpra.2023.104884
33. Weber P, Jenni O. Screening in child health - studies of the efficacy and relevance of preventive care practices. Deutsches Ärzteblatt international. 2012 Jun 15; Available from: https://www.aerzteblatt.de/10.3238/arztebl.2012.0431
34. Nelson CS, Wissow LS, Cheng TL. Effectiveness of anticipatory guidance: recent developments. Curr Opin Pediatr. 2003 Dec;15(6):630–5. doi: https://doi.org/10.1097/00008480-200312000-00015
35. Weisz J, Krueger J, Henriques J, Lacy M, Gai J, Boogaard C. Barriers to Infant Preventive Care During the COVID-19 Pandemic. Clin Pediatr (Phila). 2022 Jan;61(1):17–21. doi: https://doi.org/10.1177/00099228211050476
36. Di Mattia G, Nenna R, Mancino E, Rizzo V, Pierangeli A, Villani A, et al. During the COVID-19 pandemic where has respiratory syncytial virus gone? Pediatr Pulmonol. 2021 Oct;56(10):3106–9. doi: https://doi.org/10.1002/ppul.25582
37. Law BJ, Carbonell-Estrany X, Simoes EA. An update on respiratory syncytial virus epidemiology: a developed country perspective. Respir Med. 2002 Apr;96 Suppl B:S1–7. doi: https://doi.org/10.1053/rmed.2002.1294
38. Cheng CW, Huang YB, Chao HY, Ng CJ, Chen SY. Impact of the COVID-19 Pandemic on Pediatric Emergency Medicine: A Systematic Review. Medicina (Kaunas). 2022 Aug;58(8):1112. doi: https://doi.org/10.3390/medicina58081112
39. Watson G, Pickard L, Williams B, Hargreaves D, Blair M. ‘Do I, don’t I?’ A qualitative study addressing parental perceptions about seeking healthcare during the COVID-19 pandemic. Arch Dis Child. 2021 Nov;106(11):1118–24. doi: https://doi.org/10.1136/archdischild-2020-321260
40. Panchal U, Salazar de Pablo G, Franco M, Moreno C, Parellada M, Arango C, et al. The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur Child Adolesc Psychiatry. 2023 Jul;32(7):1151–77.
41. Samji H, Wu J, Ladak A, Vossen C, Stewart E, Dove N, et al. Review: mental health impacts of the COVID-19 pandemic on children and youth - a systematic review. Child Adolesc Ment Health. 2022 May;27(2):173–89. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/camh.12501
42. Kodjebacheva GD, Culinski T, Kawser B, Amin S. Satisfaction with pediatric telehealth according to the opinions of children and adolescents during the COVID-19 pandemic: A literature review. Front Public Health. 2023 Apr;11:1145486. doi: https://doi.org/10.3389/fpubh.2023.1145486
43. Tully L, Case L, Arthurs N, Sorensen J, Marcin JP, O’Malley G. Barriers and Facilitators for Implementing Paediatric Telemedicine: Rapid Review of User Perspectives. Front Pediatr. 2021 Mar;9:630365. doi: https://doi.org/10.3389/fped.2021.630365
44. Richard JL, Mäusezahl M, Basler S, Eckert N. Approaching measles elimination in Switzerland: changing epidemiology 2007-2018. Swiss Med Wkly. 2019 Jun;149:w20102.
45. Baroutsou V, Wymann M, Zens K, Sinniger P, Fehr J, Lang P. National and regional variations in timely adherence to recommended measles vaccination scheme in 2-years old in Switzerland, 2005-2019. Vaccine. 2022 May;40(22):3055–63. doi: https://doi.org/10.1016/j.vaccine.2022.04.008
46. 8th meeting of the European regional verification commission for measles and rubella elimination (RVC). Warsaw, Poland: WHO, regional office for Europe; Available from: https://www.who.int/europe/publications/i/item/WHO-EURO-2019-3623-43382-60860
47. Schneider R, Reinau D, Schur N, Blozik E, Früh M, Signorell A, et al. Coverage rates and timeliness of nationally recommended vaccinations in Swiss preschool children: A descriptive analysis using claims data. Vaccine. 2020 Feb;38(6):1551–8. doi: https://doi.org/10.1016/j.vaccine.2019.11.057
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.3899.