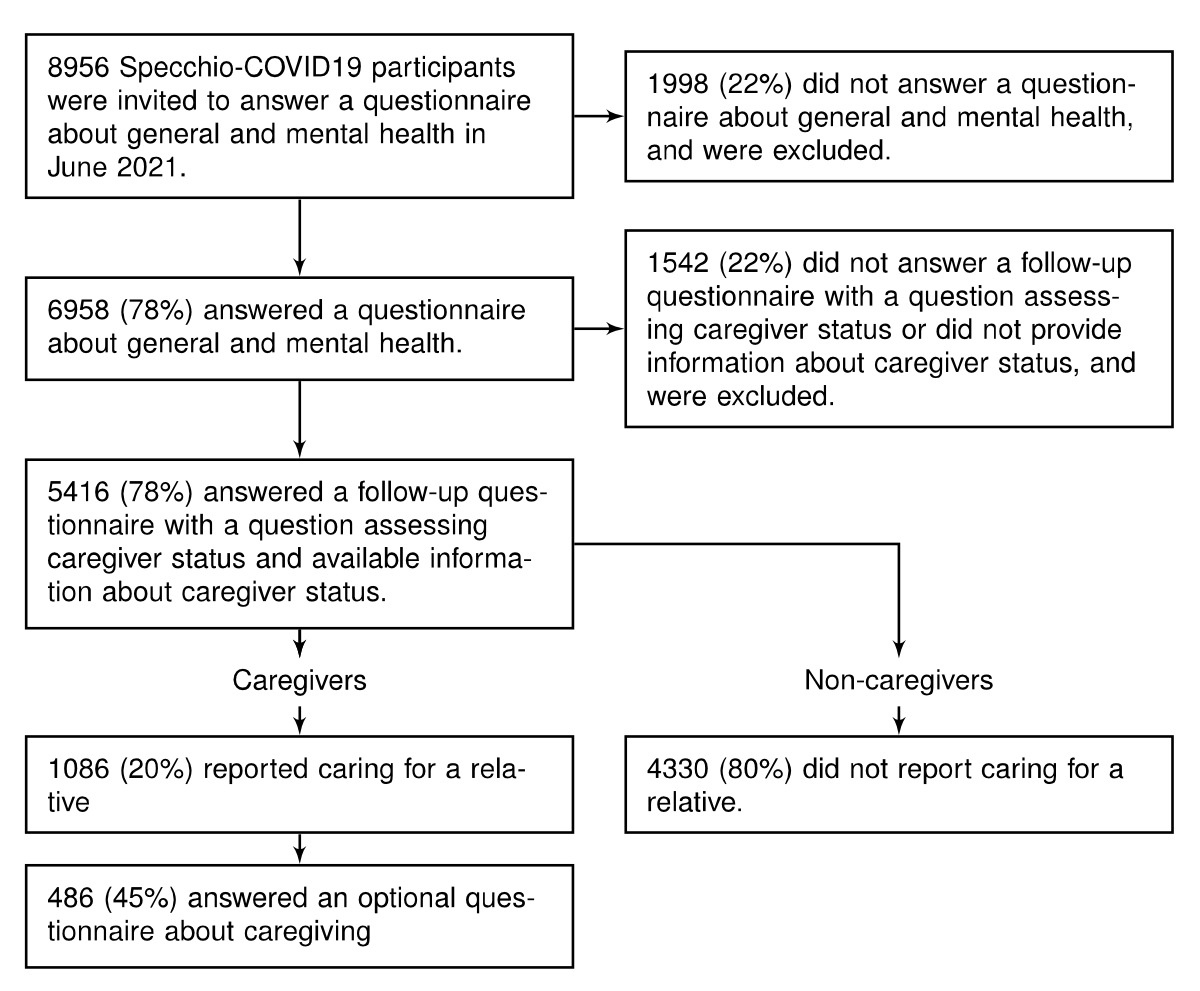
Figure 1Flowchart.
DOI: https://doi.org/https://doi.org/10.57187/s.3884
General Health Questionnaire – 12-item
Oslo Social Support Scale – 3-item
Polymerase chain reaction
Perceived Stress Scale – 10-item
Severe acute respiratory syndrome-coronavirus 2
UCLA Loneliness Scale – 3-item
World Health Organisation Well-being Index – 5-item
The COVID-19 pandemic and its associated public health measures disrupted health and care systems [1], impacting clinically vulnerable people and their informal caregivers [2–6]. Informal caregivers (hereafter used interchangeably with caregivers) are family or friends who provide non-professional care. They represent a sizeable part of the general population (5% to 44% of adults across different European countries) [7–11] and are integral to health and care systems [12, 13]. It is well known from pre-pandemic data that the caregiving burden is associated with poorer mental health outcomes [14, 15]. The pandemic unsettled nearly every aspect of informal caregivers’ lives and caregiving routines with new challenges such as lockdown, fear of transmitting the virus and restricted access to human and material resources that assist with caregiving. Moreover, caregivers may have taken additional professional adjustments and preventive measures, such as limiting social contacts to avoid transmitting the virus, leading to potential financial consequences, social isolation and a negative impact on their well-being and mental health [5, 6, 16, 17]. The pandemic may have also pushed previously non-caregivers to become new caregivers for their relatives or friends who could no longer assume some of the tasks they used to handle due to restrictions and vulnerability factors. All these factors may have exacerbated the impact of providing care on caregivers’ mental health.
During the first few months of the pandemic, informal caregivers reported poorer mental and physical health and an overall lower quality of life than non-caregivers [4, 18–24]. A few studies have examined caregivers’ mental and physical health levels compared to pre-pandemic levels. Some highlighted an increase in stress, anxiety, depression, and caregiving burden during the early phases of the pandemic, while others suggested comparable or better caregiver mental health [25, 26]. Caregiving conditions and caregivers’ health could widely vary depending on local policies and public health measures.
In Switzerland, caregivers’ mental health during the pandemic remains underexplored. Therefore, the purposes of this study were (a) to determine the prevalence of mental distress among caregivers and non-caregivers, (b) to describe the perceived evolution of the caregiving roles and burden during the COVID-19 pandemic and (c) to identify protective and risk factors for mental distress in caregivers in the context of the COVID-19 pandemic.
Data were drawn from the Specchio-COVID19 cohort study, initiated in December 2020 to follow adults (≥18 years old) who participated in successive SARS-CoV-2 serosurveys between April 2020 and June 2021 [27–31]. Serosurvey participants were randomly selected from the Bus Santé population-based study, from Geneva registries provided by the Swiss Federal Office of Statistics or the Cantonal Office for Population and Migration, and from a convenience sample of essential workers (i.e. those employed in roles considered critical for delivering vital services such as healthcare, transportation, food production and social work, among others) living or working in Geneva [27]. After a serology, they were invited to join the cohort. Participants’ sociodemographic, health and lifestyle characteristics were assessed at inclusion in the cohort, and thematic and follow-up health questionnaires were offered regularly through an online digital platform (www.specchio-hub.ch). All participants in the Specchio-COVID19 study provided informed and written consent upon study enrolment.
This study used data from an inclusion questionnaire (completed between December 2020 and June 2021) and four additional questionnaires administered between June and July 2021. The first focused on general and mental health and included the 12-item General Health Questionnaire (GHQ-12). The second centred on well-being and mental health, including measures of stress, depression, and social support; its completion was optional for inclusion in this study. The third included a question assessing caregiver status. Finally, the fourth was exclusively sent to caregivers and explored their caregiving responsibilities and the characteristics of their care recipients. The latest included variables were selected as candidate risk and protective factors for mental distress in caregivers based on existing research and practical considerations from experts in the field. The variables collected in each questionnaire are detailed in table S1 in the appendix.
Participants in the Specchio-COVID19 study were eligible for this analysis if they had completed (a) a questionnaire about general and mental health and (b) a follow-up questionnaire with a question assessing caregiver status (figure 1).
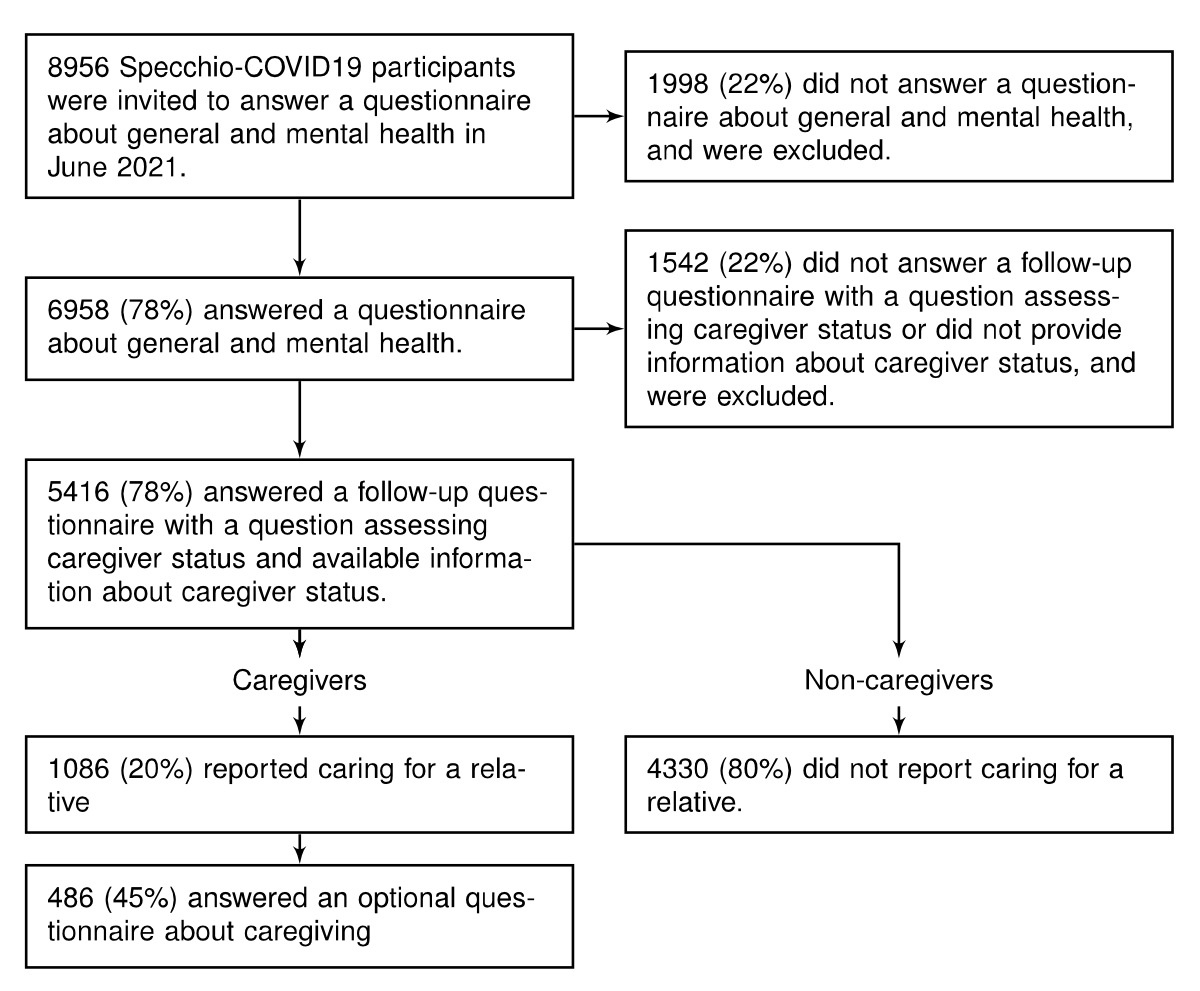
Figure 1Flowchart.
Caregiving status was the main exposure of this study. Individuals who answered affirmatively to the question “Since the start of the pandemic, have you regularly helped (in a non-professional role) a person close to you (dependent, elderly, ill or disabled person) with the tasks of daily living (for example, washing or shopping, meals, housework)?” in June 2021 were categorised as informal caregivers.
The primary outcome was mental distress, measured by the 12-item General Health Questionnaire. This internationally validated scale comprises 12 mental health questions (e.g. concentration, sleep loss, stress, confidence), including six positively and six negatively worded questions. Each item is scored on a four-point Likert system ranging from zero to three points. Its maximum total score is 36 points, with a higher score indicating greater distress. Mental distress was defined as a score of ≥12 points [32, 33].
Additional mental health measures included well-being as measured by the WHO-5 Well-being Index (WHO-5), loneliness as measured by the UCLA Loneliness Scale (UCLA-3), and perceived stress as measured by the 10-item Perceived Stress Scale (PSS-10), with the definitions provided in appendix table S1.
The covariates included caregivers’ demographics (e.g. age, sex, birth country, and education) and pre-existing mental and physical health, assessed at inclusion in the cohort. A previous SARS-CoV-2 infection was defined as either (a) a positive serological, antigenic or polymerase chain reaction (PCR) test self-reported at inclusion or in a follow-up questionnaire, (b) a positive serology indicating natural infection (presence of anti-nucleocapsid antibodies) or (c) a positive PCR test according to a database established by regional public health authorities before 1 June 2021 [34].
Potential risk and protective factors for distress among caregivers were assessed at inclusion in the cohort (e.g. demographics), in a questionnaire about well-being and mental health (e.g. social support) and in an optional questionnaire about caregiving responsibilities and care recipient’s characteristics. They are defined in table S1 in the appendix and can be summarised as follows: (a) factors related to the caregiver (e.g. age, sex, and pre-existing conditions), (b) factors related to caregiving (e.g. frequency, distance from caregiver to care recipient, type of care, such as help with activities of daily living, and age of the care recipient) and (c) factors related to the COVID-19 pandemic (e.g. increase in caregiving burden and availability of healthcare professionals). If a caregiver cared for more than one individual, the participant was asked to answer a set of questions on caregiving specific to each person (e.g. care recipient’s age, reason for care, relationship, distance, and frequency and type of care). For care recipient-related variables, the data was derived from the first reported care recipient unless otherwise specified.
Baseline sociodemographic and mental health characteristics were compared between caregivers and non-caregivers and between caregivers with and without mental distress. Risk and protective factors for mental distress in caregivers were also assessed. All descriptive analyses included absolute numbers with relative percentages for categorical variables and means and standard deviations or medians with interquartile ranges for continuous variables. Hypotheses were tested using the chi-squared tests, Welch’s two-sample t-test or the Wilcoxon-Mann-Whitney test, as appropriate. The significance level was set at p<0.05.
The prevalence of distress was adjusted for confounders and compared among caregivers and non-caregivers. Based on existing literature, potential confounders of the association between caregiver status and mental distress were identified using a directed acyclic graph: sex, age and country of birth (figure S1 in the appendix). The adjusted prevalence of distress was calculated using average adjusted predictions. First, a linear regression model was fitted, including caregiver status as the primary predictor and confounders as covariates, including age, sex and birth country. Then, predictions were made for each individual in the dataset using their observed values for all covariates and averaged within caregiver and non-caregiver groups. This approach estimates the expected prevalence of distress, adjusted for the distribution of other confounders in the study population. A sensitivity analysis was conducted on a subsample of participants exclusively drawn from random samples of the general population (i.e. excluding essential workers).
The risk and protective factors for mental distress in caregivers were assessed using unadjusted and adjusted logistic regressions. The adjustment set included sex, age, education, social support, pre-existing mental condition and pre-existing physical condition. The results are reported as odds ratios (ORs) with 95% confidence intervals (CIs). Sensitivity analyses were conducted to test the robustness of the observed associations. First, the same models were run in a subsample of the caregivers from the general population (i.e. excluding essential workers). Then, when a caregiver reported caring for multiple care recipients, the data relative to the first care recipient was replaced with the data for the second care recipient. This approach allowed for an examination of whether the results were influenced by the characteristics of the care recipient in cases where a caregiver cared for multiple care recipients.
Missing data ranged from 0 to 20% per variable. Multiple imputation by chained equations (MICE) with predictive mean matching was used to treat missing data in all models [35].
All analyses were conducted using R (v.4.1.2; R Foundation for Statistical Computing, Vienna, Austria) with packages including dplyr (v.1.1.4), tidyverse (v.2.0), gtsummary (v.1.7.2), marginaleffects (v.0.17), mice (v.3.16), ggplot2 (v.3.4.4), and likert (v.1.3.5). The code is available at: https://gist.github.com/cedricfollonier/052233eb0bb4c8025f400c8fc1289a3e.
Participants were not involved in setting the research questions or outcome measures or designing the study. However, they showed overwhelming support for the study through continuing attendance for follow-up.
Among the Specchio-COVID19 participants eligible for this study, 1086 (20%) declared being caregivers (figure 1). Table 1 presents the characteristics of caregivers and non-caregivers. Overall, their mean age was 51 years, 56% were female, and 52% had completed tertiary education. Caregivers were more often female (60% vs 55%, p = 0.002), born in Switzerland (70% vs 59%, p <0.001), and had lower household income (p = 0.002) than non-caregivers.
Table 1Demographics, physical and mental health of non-caregivers and caregivers.
| Overall, N = 5416* | Non-caregivers, N = 4330* | Caregivers, N = 1086* | |||
| n / N (%) | n / N (%) | n / N (%) | p-value** | ||
| Sociodemographic characteristics | |||||
| Female sex | 3052 / 5416 (56%) | 2395 / 4330 (55%) | 657 / 1086 (60%) | 0.002 | |
| Age (years), mean (SD) | 51 (13) | 51 (14) | 52 (12) | 0.001 | |
| In a relationship | 4004 / 5414 (74%) | 3217 / 4329 (74%) | 787 / 1085 (73%) | 0.248 | |
| Born in Switzerland | 3335 / 5416 (62%) | 2574 / 4330 (59%) | 761 / 1086 (70%) | <0.001 | |
| Education | 0.183 | ||||
| Primary | 179 / 5414 (3.3%) | 145 / 4328 (3.4%) | 34 / 1086 (3.1%) | ||
| Secondary | 2423 / 5414 (45%) | 1910 / 4328 (44%) | 513 / 1086 (47%) | ||
| Tertiary | 2812 / 5414 (52%) | 2273 / 4328 (53%) | 539 / 1086 (50%) | ||
| Professionally active | 4023 / 5413 (74%) | 3199 / 4328 (74%) | 824 / 1085 (76%) | 0.183 | |
| Household income | 0.002 | ||||
| Low | 707 / 4322 (16%) | 540 / 3446 (16%) | 167 / 876 (19%) | ||
| Medium | 2863 / 4322 (66%) | 2276 / 3446 (66%) | 587 / 876 (67%) | ||
| High | 752 / 4322 (17%) | 630 / 3446 (18%) | 122 / 876 (14%) | ||
| Limited social support (OSSS-3)*** | 735 / 4642 (16%) | 589 / 3698 (16%) | 146 / 944 (15%) | 0.767 | |
| Pre-existing physical condition | 1214 / 5416 (22%) | 957 / 4330 (22%) | 257 / 1086 (24%) | 0.287 | |
| Pre-existing mental condition | 110 / 5416 (2.0%) | 86 / 4330 (2.0%) | 24 / 1086 (2.2%) | 0.728 | |
| Physical health | |||||
| Self-perceived health status | 0.062 | ||||
| Good or very good | 4849 / 5416 (90%) | 3891 /4330 (90%) | 958 / 1086 (88%) | ||
| Average | 517 / 5416 (9.5%) | 405 / 4330 (9.4%) | 112 / 1086 (10%) | ||
| Poor or very poor | 50 / 5416 (0.9%) | 34 / 4330 (0.8%) | 16 / 1086 (1.5%) | ||
| Previous SARS-CoV-2 infection | 1610 / 5416 (30%) | 1282 / 4330 (30%) | 328 / 1086 (30%) | 0.729 | |
| Mental health*** | |||||
| Self-perceived mental health status | 0.726 | ||||
| Good or very good | 4247 / 5416 (78%) | 3404 /4330 (79%) | 843 / 1086 (78%) | ||
| Average | 1009 / 5416 (19%) | 801 / 4330 (18%) | 208 / 1086 (19%) | ||
| Poor or very poor | 160 / 5416 (3.0%) | 125 / 4330 (2.9%) | 35 / 1086 (3.2%) | ||
| Well-being index (WHO-5), median (IQR) | 68 (48–80) | 68 (48–80) | 64 (48–80) | 0.048 | |
| Well-being index (WHO-5) | 0.627 | ||||
| Well-being (WHO-5 = >50) | 3393 / 4642 (73%) | 2711 / 3698 (73%) | 682 / 944 (72%) | ||
| Poor well-being (WHO-5 = 29–50) | 821 / 4642 (18%) | 644 / 3698 (17%) | 177 / 944 (19%) | ||
| Depression (WHO-5 = ≤28) | 428 / 4642 (9.2%) | 343 / 3698 (9.3%) | 85 / 944 (9.0%) | ||
| Loneliness (UCLA-3) | 584 / 4642 (13%) | 464 / 3698 (13%) | 120 / 944 (13%) | 0.905 | |
| Perceived stress (PSS-10),median (IQR) | 22 (17–28) | 22 (17–27) | 23 (18–28) | <0.001 | |
| Mental distress (GHQ-12), median (IQR) | 10 (8–13) | 10 (8–13) | 10 (8–14) | <0.001 | |
| Mental distress (GHQ-12 ≥12), observed prevalence (95% CI) | 2044 / 5416 (38% [36–39]) | 1597 / 4330 (37% [35–38]) | 447 / 1086 (41% [38–44]) | 0.010 | |
| Mental distress (GHQ-12 ≥12), adjusted prevalence**** (95% CI) | 36% (35–38) | 41% (38–44) | 0.004 | ||
GHQ-12: General Health Questionnaire – 12-item; IQR: interquartile range; OSSS-3: Oslo Social Support Scale – 3-item; PSS-10: Perceived Stress Scale – 10-item; SD: standard deviation; UCLA-3: UCLA Loneliness Scale – 3-item; WHO-5: World Health Organisation Well-being Index – 5-item (WHO-5).
* Data are presented as n / N (%), mean (SD) or median (IQR).
** P-values were calculated using Pearson’s Chi-squared test, Welch’s two-sample t-test or the Wilcoxon rank sum test.
*** Secondary mental health measures (i.e. social support [OSSS-3], well-being index [WHO-5], loneliness [UCLA-3], and perceived stress [PSS-10]) were assessed in an additional and optional well-being and mental health questionnaire; they were missing for 774 participants who did not answer the latter.
**** Adjusted prevalences are expressed as percentages and were calculated as means of each level of distress status averaged across each level of covariates, including sex, age and birth country.
The overall observed prevalence of mental distress (GHQ-12 score ≥12 points) was 38% (95% CI: 36–39%) as of June 2021. Caregivers were more frequently affected than non-caregivers (41% vs 37%, p = 0.009), even after adjusting for age, sex and country of birth (41% vs 36%, p = 0.004). In both groups, the most frequently reported items of the GHQ-12 were feeling under stress and losing sleep (figures S2 and S3). In addition, caregivers reported slightly poorer well-being (64 vs 68 points, p = 0.048) and higher levels of perceived stress (23 vs 22 points, p <0.001). There was no significant difference in the prevalence of loneliness (13% vs 13%, p = 0.905). The unadjusted and adjusted prevalence of distress remained similar and significantly more frequent among caregivers in a sensitivity analysis conducted on a subsample representative of the general population (appendix table S2).
The characteristics of the responding and non-responding caregivers are detailed in table S3 in the appendix: respondents were older (54 vs 50 years, p <0.001) and more often female (64% vs 58%, p = 0.040).
Among caregivers, 7% of the care recipients were spouses or partners, and 64% were first-degree relatives (table 2). Most caregivers cared for a single person (66%, figure S4 in the appendix). When caregivers cared for more than one person, the characteristics of the first and second care recipients they reported are shown in table S4 in the appendix. Care recipients often lived separately from their caregivers but within a 10 km distance. Ageing (78%) was the predominant reason for caregiving, with 63% of care recipients aged 80 years old or above (appendix figure S5). Help with instrumental activities of daily living (96%) and social support (66%) were frequent. Most caregivers (78%) received additional support from another informal (e.g. another caregiver or a volunteer) or formal (e.g. a home care nurse) source (appendix figure S6).
Table 2Association of factors related to the caregiver with mental distress in a subsample of 486 informal caregivers who completed an additional questionnaire about caregiving.
| Descriptive | Unadjusted | Adjusted# | ||||||||
| Overall, N = 486* | No mental distress, N = 284* | Mental distress, N = 202* | Mental distress vs no distress | Mental distress vs no distress | ||||||
| n / N (%) | n / N (%) | n / N (%) | p-value** | OR | 95% CI | p-value*** | aOR | 95% CI | p-value*** | |
| Female sex (ref. male sex) | 311 / 486 (64%) | 176 / 284 (62%) | 135 / 202 (67%) | 0.315 | 1.24 | 0.85, 1.81 | 0.272 | 1.05 | 0.96, 1.15 | 0.263 |
| Age (per 5 years)##, mean (SD) | 54 (11) | 55 (11) | 53 (12) | 0.055 | 0.92 | 0.85, 1.00 | 0.053 | 0.98 | 0.96, 1.00 | 0.034 |
| In a relationship (ref. not in a relationship) | 348 / 486 (72%) | 207 / 284 (73%) | 141 / 202 (70%) | 0.521 | 0.86 | 0.58, 1.28 | 0.458 | 0.96 | 0.87, 1.06 | 0.462 |
| Born in Switzerland (ref. not born in Switzerland) | 355 / 486 (73%) | 207 / 284 (73%) | 148 / 202 (73%) | >0.999 | 1.02 | 0.68, 1.53 | 0.926 | 1.01 | 0.91, 1.11 | 0.861 |
| Completed tertiary education (ref. no tertiary education) | 241 / 486 (50%) | 140 / 284 (49%) | 101 / 202 (50%) | 0.951 | 1.03 | 0.72, 1.48 | 0.878 | 1.02 | 0.94, 1.11 | 0.624 |
| Professionally active (ref. not professionally active) | 361 / 486 (74%) | 206 / 284 (73%) | 155 / 202 (77%) | 0.348 | 1.25 | 0.82, 1.90 | 0.298 | 1.02 | 0.91, 1.15 | 0.681 |
| Low household income (ref. mid or high household income) | 67 / 390 (17%) | 40 / 230 (17%) | 27 / 160 (17%) | >0.999 | 0.99 | 0.59, 1.66 | 0.968 | 0.99 | 0.87, 1.13 | 0.926 |
| Limited social support (OSSS-3) (ref. strong social support) | 68 / 463 (15%) | 27 / 270 (10%) | 41 / 193 (21%) | 0.001 | 2.45 | 1.45, 4.12 | <0.001 | 1.25 | 1.10, 1.42 | <0.001 |
| Pre-existing mental condition (ref. no pre-existing mental condition) | 11 / 486 (2.3%) | 3 / 284 (1.1%) | 8 / 202 (4.0%) | 0.070 | 3.86 | 1.01, 14.8 | 0.049 | 1.30 | 0.97, 1.75 | 0.077 |
| Pre-existing physical condition (ref. no pre-existing physical condition) | 128 / 486 (26%) | 68 / 284 (24%) | 60 / 202 (30%) | 0.188 | 1.34 | 0.89, 2.02 | 0.157 | 1.08 | 0.98, 1.19 | 0.121 |
aOR: adjusted odds ratio; OR: odds ratio; IQR: interquartile range; OSSS-3: Oslo Social Support Scale – 3-item; SD: standard deviation; ref.: reference category.
* Data are presented as n / N (%), mean (SD) or median (IQR).
** P-values were calculated using Pearson’s Chi-squared test or Welch’s two-sample t-test, as appropriate.
*** P-values were calculated for logistic regression coefficients.
# Adjusted for sex, age, education, social support, pre-existing mental condition and pre-existing physical condition.
## Odds ratio for age is presented for each five-year increase.
The pandemic appears to have influenced informal caregiving, with 40% of caregivers experiencing decreased healthcare availability, 61% expressing concerns about being unable to help their care recipient in case of COVID-19 or quarantine, and 24% feeling more isolated in their role since the pandemic onset. Among professionally active caregivers, 13% had to make occupational adaptations to accommodate their caregiving responsibilities, including taking paid leave (38%), work schedule flexibility (31%), reduction in working hours (23%) or resignation (6%) (appendix figure S7). In addition, 47% of caregivers experienced an increase in caregiving burden since the pandemic onset, primarily driven by increased care recipient needs (67%), willingness to limit contacts with the care recipient (61%), and reduced availability of other sources of formal support (34%) (appendix figure S8).
Risk and protective factors for distress in caregivers are presented in tables 2, 3 and 4. Among caregiver-related factors, older caregivers had a lower likelihood of expressing mental distress, while those with limited social support presented a higher likelihood (table 2).
Table 3Association of factors related to the care recipient and the act of caregiving with mental distress in a subsample of 486 informal caregivers who completed an additional questionnaire about caregiving.
| Descriptive | Unadjusted | Adjusted# | |||||||||
| Overall, N = 486* | No mental distress, N = 284* | Mental distress, N = 202* | Mental distress vs no distress | Mental distress vs no distress | |||||||
| n / N (%) | n / N (%) | n / N (%) | p-value** | OR | 95% CI | p-value*** | aOR | 95% CI | p-value*** | ||
| Cared for ≥2 care recipients (ref. 1 care recipient) | 164 / 486 (34%) | 88 / 284 (31%) | 76 / 202 (38%) | 0.153 | 1.34 | 0.92, 1.97 | 0.128 | 1.05 | 0.96, 1.15 | 0.270 | |
| Older care recipient (≥80 years, ref. younger care recipient) | 307 / 485 (63%) | 184 / 284 (65%) | 123 / 201 (61%) | 0.476 | 0.86 | 0.59, 1.26 | 0.441 | 1.01 | 0.92, 1.10 | 0.907 | |
| Condition of the care recipient | Ageing | 380 / 486 (78%) | 224 / 284 (79%) | 156 / 202 (77%) | 0.748 | 0.91 | 0.59, 1.41 | 0.665 | 0.99 | 0.89, 1.10 | 0.823 |
| Physical health condition | 188 / 486 (39%) | 107 / 284 (38%) | 81 / 202 (40%) | 0.656 | 1.11 | 0.76, 1.60 | 0.589 | 1.03 | 0.94, 1.13 | 0.491 | |
| Mental health condition | 46 / 486 (9.5%) | 18 / 284 (6.3%) | 28 / 202 (14%) | 0.008 | 2.38 | 1.27, 4.44 | 0.007 | 1.21 | 1.05, 1.41 | 0.011 | |
| Relationship between the care recipient and caregiver | 0.271 | ||||||||||
| Spouse or partner | 32 / 486 (6.6%) | 23 / 284 (8.1%) | 9 / 202 (4.5%) | — | — | — | — | ||||
| First degree relative | 311 / 486 (64%) | 180 / 284 (63%) | 131 / 202 (65%) | 1.86 | 0.83, 4.16 | 0.130 | 1.13 | 0.94, 1.35 | 0.198 | ||
| Other | 143 / 486 (29%) | 81 / 284 (29%) | 62 / 202 (31%) | 1.96 | 0.84, 4.53 | 0.118 | 1.13 | 0.93, 1.37 | 0.213 | ||
| Duration of the care relation | 0.651 | ||||||||||
| Less than a year | 120 / 485 (25%) | 66 / 284 (23%) | 54 / 201 (27%) | — | — | — | — | ||||
| One to five years | 239 / 485 (49%) | 142 / 284 (50%) | 97 / 201 (48%) | 0.84 | 0.54, 1.30 | 0.431 | 0.99 | 0.89, 1.10 | 0.855 | ||
| More than five years | 126 / 485 (26%) | 76 / 284 (27%) | 50 / 201 (25%) | 0.81 | 0.49, 1.34 | 0.407 | 0.97 | 0.86, 1.10 | 0.654 | ||
| Frequency of care | 0.850 | ||||||||||
| Daily or almost daily | 72 / 440 (16%) | 42 / 256 (16%) | 30 / 184 (16%) | — | — | — | — | ||||
| 3–5 days a week | 46 / 440 (10%) | 24 / 256 (9.4%) | 22 / 184 (12%) | 1.16 | 0.57, 2.35 | 0.678 | 1.01 | 0.85, 1.20 | 0.940 | ||
| 1–2 days a week | 196 / 440 (45%) | 115 / 256 (45%) | 81 / 184 (44%) | 0.92 | 0.55, 1.56 | 0.762 | 0.98 | 0.86, 1.11 | 0.699 | ||
| A few times a month or less | 126 / 440 (29%) | 75 / 256 (29%) | 51 / 184 (28%) | 0.88 | 0.50, 1.54 | 0.649 | 0.96 | 0.83, 1.10 | 0.513 | ||
| Distance between the care recipient and caregiver | 0.161 | ||||||||||
| Same home or building | 104 / 472 (22%) | 68 / 278 (24%) | 36 / 194 (19%) | — | — | — | — | ||||
| 10 km or less | 272 / 472 (58%) | 160 / 278 (58%) | 112 / 194 (58%) | 1.35 | 0.84, 2.16 | 0.212 | 1.06 | 0.95, 1.19 | 0.268 | ||
| More than 10 km | 96 / 472 (20%) | 50 / 278 (18%) | 46 / 194 (24%) | 1.81 | 1.03, 3.20 | 0.040 | 1.17 | 1.02, 1.34 | 0.021 | ||
| Type of care | Social support (ref. no social support) | 323 / 486 (66%) | 186 / 284 (65%) | 137 / 202 (68%) | 0.661 | 1.11 | 0.76, 1.63 | 0.592 | 1.02 | 0.93, 1.12 | 0.622 |
| Help with instrumental activities of daily living (IADL, ref. no help with IADL)## | 468 / 485 (96%) | 274 / 284 (96%) | 194 / 201 (97%) | >0.999 | 1.01 | 0.38, 2.71 | 0.983 | 0.98 | 0.78, 1.25 | 0.895 | |
| Help with activities of daily living (ADL, ref. no help with ADL)### | 53 / 485 (11%) | 26 / 284 (9.2%) | 27 / 201 (13%) | 0.180 | 1.55 | 0.87, 2.74 | 0.136 | 1.15 | 1.00, 1.32 | 0.050 | |
| Other support from formal or informal networks, including other caregivers (ref. no other support from formal or informal networks) | 380 / 485 (78%) | 232 / 284 (82%) | 148 / 201 (74%) | 0.044 | 0.63 | 0.40, 0.97 | 0.035 | 0.91 | 0.82, 1.01 | 0.089 | |
aOR: adjusted odds ratio; IQR: interquartile range; OR: odds ratio; ref.: reference category; SD: standard deviation.
* Data are presented as n / N (%), mean (SD) or median (IQR).
** P-values were calculated using Pearson’s Chi-squared test or Welch’s two-sample t-test, as appropriate.
*** P-values were calculated for logistic regression coefficients.
# Adjusted for sex, age, education, social support, pre-existing mental condition and pre-existing physical condition.
## Instrumental activities of daily living (IADL) consist of tasks allowing an individual to live independently and include using the telephone, managing medications, preparing meals, managing money and bills, shopping for groceries and necessities, cleaning and maintaining the house and using transportation (e.g. using public transport).
### Activities of daily living (ADL) consist of basic self-care tasks and include bathing and showering, maintaining personal hygiene, dressing, toileting, transferring (e.g. moving from the bed to a chair), controlling continence and feeding.
Among caregiving- and care recipient-related factors, caregivers caring for an individual with a mental condition and those living more than 10 km away from the care recipient had about 20% increased odds of suffering from mental distress. The caregiver and care-recipient’s degree of relationship, duration of care relationship, frequency of care, and older age of the care recipient (≥80 years old) were not significantly associated with mental distress, but the confidence intervals were large (table 3).
Among COVID-19 pandemic-related factors, caregivers feeling more isolated in their caregiving role since the pandemic onset, those worrying about the inability to carry the care responsibility due to COVID-19 or quarantine, and those experiencing decreased availability of healthcare workers had significantly higher odds of experiencing mental distress (table 4).
Table 4Association of factors related to the COVID-19 pandemic with mental distress in a subsample of 486 informal caregivers who completed an additional questionnaire about caregiving.
| Descriptive | Unadjusted | Adjusted**** | ||||||||
| Overall, N = 4861 | No mental distress, N = 284* | Mental distress, N = 202* | Mental distress vs no distress | Mental distress vs no distress | ||||||
| n / N (%) | n / N (%) | n / N (%) | p-value** | OR | 95% CI | p-value*** | aOR | 95% CI | p-value*** | |
| Previous SARS-CoV-2 infection (ref. no previous SARS-CoV-2 infection) | 144 / 486 (30%) | 81 / 284 (29%) | 63 / 202 (31%) | 0.593 | 1.14 | 0.77, 1.69 | 0.526 | 1.04 | 0.95, 1.14 | 0.422 |
| Increased caregiving burden (ref. stable or decreased caregiving burden) | 229 / 485 (47%) | 134 / 284 (47%) | 95 / 201 (47%) | >0.999 | 1.00 | 0.69, 1.43 | 0.982 | 0.99 | 0.91, 1.08 | 0.840 |
| Professional adaptations due to caregiver duties (ref. no professional adaptations) | 48 / 376 (13%) | 20 / 216 (9.3%) | 28 / 160 (18%) | 0.027 | 1.86 | 0.98, 3.52 | 0.056 | 1.14 | 0.98, 1.34 | 0.086 |
| Feeling more isolated in one’s caregiving role since the pandemic onset (ref. not feeling more isolated in one’s caregiving role) | 114 / 485 (24%) | 49 / 284 (17%) | 65 / 201 (32%) | <0.001 | 2.29 | 1.49, 3.51 | <0.001 | 1.20 | 1.08, 1.32 | <0.001 |
| Worrying about the inability to care due to COVID-19 or quarantine (ref. not worrying about the inability to care) | 297 / 485 (61%) | 155 / 284 (55%) | 142 / 201 (71%) | <0.001 | 2.01 | 1.37, 2.96 | <0.001 | 1.18 | 1.08, 1.29 | <0.001 |
| Experiencing decreased availability of healthcare professionals (ref. not experiencing decreased availability of healthcare professionals) | 311 / 486 (64%) | 176 / 284 (62%) | 135 / 202 (67%) | 0.315 | 1.68 | 1.16, 2.43 | 0.006 | 1.11 | 1.02, 1.22 | 0.017 |
aOR: adjusted odds ratio; COVID-19: coronavirus disease 2019; OR: odds ratio; ref: reference category; SARS-CoV-2: severe acute respiratory syndrome-coronavirus 2
* Data are presented as n / N (%), mean (SD) or median (IQR).
** P-values were calculated using Pearson’s Chi-squared test or Welch’s two-sample t-test, as appropriate.
*** P-values were calculated for logistic regression coefficients.
**** Adjusted for sex, age, education, social support, pre-existing mental condition and pre-existing physical condition.
Sensitivity analyses showed similar results in direction and magnitude (tables S5 and S6 in the appendix), suggesting that these results may apply to the general population and are robust regardless of whether the caregiver cared for one or more persons.
This study highlights higher mental distress in caregivers compared to non-caregivers 16 months after the onset of the COVID-19 pandemic. Caregivers reported perceiving significant changes in their caregiving responsibilities since the onset of the pandemic, including reduced healthcare access, increased concerns, feelings of isolation, occupational adjustments to meet their caregiving duties, and a greater caregiving burden. Low social support, caring for an individual with a mental condition, living far from the care recipient, feeling more isolated in one’s caregiver role and worrying about the inability to care in case of COVID-19 or quarantine were risk factors for mental distress in caregivers.
The proportion of caregivers varies significantly across countries and its definition tends to be polymorphous. The proportion of caregivers in our sample was 20%, aligning with previous findings in Europe, where between 5% and 44% of the population provide informal care [7–11]. Nonetheless, the open nature of the question used to identify caregivers leaves room for personal interpretation, reflecting each respondent’s own interpretation of their caregiver status. Therefore, it may have favoured the selection of those more deeply engaged in caregiving tasks, such as assistance with bathing or meal preparation, potentially underrepresenting those whose caregiving roles were purely administrative or social.
Both before and during the pandemic, the literature tends to describe poorer mental health in caregivers than in non-caregivers across multiple outcomes such as anxiety, depression, mental distress and suicidal ideation [4, 15, 18–25, 36–39]. These results are nuanced and could be explained by regional, caregiver subgroups (e.g. caregivers of a child with autism or adults with dementia) and measurement variations. In addition, findings in the context of the pandemic emerge from data collected at the beginning and/or at the height of the pandemic, and it remains unknown whether this effect will last over time. In this study, caregivers experienced more instances of mental distress and stress and a slightly lower level of well-being than non-caregivers. This result supports pre-pandemic research showing that caring for someone, while rewarding, can be stressful and burdensome, leading to adverse physical and mental effects, such as increased stress, depression, emotional and cognitive impairments, and decreased subjective well-being [14, 15, 40]. This burden arises from the demanding nature of caregiving responsibilities, which can limit the time caregivers have available to attend to their own health needs and directly affect physical health [41].
Among caregivers, several factors may contribute to depression, stress, and low subjective well-being. Caregiver-related factors such as sex, education or socioeconomic status were not significantly associated with mental distress in this study. This finding is contradictory to previous studies, which showed that females experience more negative impacts of caregiving on their mental health [42, 43]. There were no associations but wide confidence intervals for factors such as the degree of relationship, duration of the care relationship and frequency of care, which had been previously linked with poorer mental health among caregivers [15, 42, 43]. Other factors, including the caregiver’s responsibility for a care recipient with a mental condition and living at a distance, both adding stress and demands, were identified. These results partly support previous studies, which highlighted that mental health was negatively impacted by the presence of cognitive-behavioural disorders in care recipients [15, 42, 43]. Finally, limited social support was shown to be associated with poorer mental health among caregivers, as previously suggested [44].
The COVID-19 pandemic is thought to have exacerbated the regular emotional, physical and financial strains associated with caregiving [45] and introduced a distinct set of challenges for caregivers. Accordingly, in this study, approximately 40% of caregivers experienced a decrease in the availability of healthcare professionals who might have had difficulty maintaining routine health services due to the surge of patients with COVID-19 and restrictive public health measures. Consequently, caregivers had to assume additional responsibilities, including tasks typically performed by professional caregivers, and experienced increased workload, task complexity, and time commitment dedicated to caregiving, with potential financial implications. Given this context, nearly half of the caregivers reported that the burden of care had increased since the onset of the pandemic, primarily due to increased care recipient needs, limited contact with other individuals involved in caregiving and reduced availability of formal support systems. This finding is consistent with a trend reported throughout Europe [38, 46]. Over half of the caregivers reported concerns about being unable to help their care recipient due to COVID-19 or quarantine, and about a quarter felt more isolated in their role; they were more likely to suffer from mental distress, as previously identified [47]. Ultimately, the association between decreasing healthcare professional availability, not receiving any external support during the pandemic, and increased mental distress underscores the importance of formal and informal support networks in the context of caregiving. These networks are essential in preserving caregiver’s well-being and enhancing their capacity for providing optimal care to their recipients.
This study screened mental distress using the GHQ-12, scored with the Likert method (0–1–2–3), considering a threshold of 12 points. This scoring method is more reliable for screening depressive disorders than the binary method, where responses are scored as 0–0–1–1 [48], but results in a higher prevalence of mental distress (38% vs 20% using the binary method) by including individuals with milder symptoms of distress. Nonetheless, the high prevalence of mental distress underscores the difficult times encountered during the study period due to the disruptions caused by the health crisis.
This study identified modifiable risk factors for distress in caregivers during a pandemic. In the event of a future pandemic or any events leading to disruption in healthcare systems, measures should be implemented to ensure that caregivers receive appropriate social support, including from formal and informal support networks. We also highlighted a need for rapidly implementable solutions when regular caregivers temporarily cannot provide care due to unforeseen personal or societal circumstances, including developing contingency plans, such as identifying backup caregivers, arranging temporary home nursing care or utilising temporary placement facilities. These measures would benefit both caregivers, who have particular needs, and their care recipients through continuity of care.
Mental health improved in the general population after the early stages of the pandemic [49]. However, the trajectory of caregiver mental health during the subsequent stages of the pandemic remains unknown, making it challenging to discern whether the impact of the pandemic is transient or long-lasting in this population. Longitudinal investigations are warranted to follow the evolution of informal caregivers’ well-being and mental health and provide insights into the possible lasting consequences of this global health crisis.
This study had several strengths, including comprehensive data regarding sociodemographic status, mental health and caregiving responsibilities during the pandemic, derived from a cohort primarily composed of individuals randomly selected from the general population. While previous studies have mainly focused on specific populations of caregivers and care recipients, often suffering from severe conditions such as autism or dementia, this study included a wide range of caregivers and care recipients and thus might be more representative of real-life caregiving. Indeed, this approach allows the identification of shared characteristics and challenges they might face collectively.
Several limitations should be acknowledged. Including both a population-based sample and a sample of essential workers may have limited the representativeness of our findings. However, the results were similar when the analysis was restricted to participants from the population-based sample. Self-selection bias may have occurred at different levels: older, better-educated, and more health-conscious people are more likely to enrol in research studies and maintain participation over time, as commonly observed in cohort studies [50]. Caregivers may have been both more and less likely to answer the caregiving questionnaire, depending on their willingness to share their experiences and their exhaustion level. Unfortunately, the absence of pre-pandemic data prevented a direct comparison of mental health status and caregiving responsibilities change. Mental distress was measured when public health measures were progressively being eased in Switzerland, and its prevalence may have been lower than during the height of the pandemic but higher than in the post-pandemic period. Finally, caregiving responsibilities are influenced by societal, political, health and care settings, and these results should be generalised cautiously.
Sixteen months after the onset of the COVID-19 pandemic, most caregivers reported an increase in their caregiving burden. Compared to non-caregivers, they faced additional mental health challenges, which could be attributed to increased caregiving responsibilities and reduced support. Public health policies should ensure caregivers receive additional support and resources, such as social support, and continuity of care from formal caregivers, and include rapidly implementable solutions to maintain caregiving continuity, especially during pandemics.
Data will be shared upon reasonable request.
The authors are indebted to the participants of the Specchio-COVID19 cohort for their commitment and cooperation. This study would not have been possible without the instrumental and passionate contribution of the staff in the Unit of Population Epidemiology, Division of Primary Care Medicine, Geneva University Hospitals, Geneva, Switzerland; the professionalism of our partners Médecine & Hygiène and dotBase; and all our colleagues not included in the Specchio-COVID19 study group. We particularly thank the Specchio-COVID19 operational team, who dedicatedly responded to participants’ queries. We also thank the Corona Immunitas digital follow-up group for their help in developing the caregiver questionnaire.
Specchio-COVID19 study group: Isabelle Arm-Vernez, Andrew S. Azman, Delphine Bachmann, Antoine Bal, Jean-François Balavoine, Rémy P. Barbe, Hélène Baysson, Julie Berthelot, Aminata Rosalie Bouhet, Gaëlle Bryand-Rumley, François Chappuis, Prune Collombet, Sophie Coudurier-Boeuf, Delphine S. Courvoisier, Carlos de Mestral, Paola D’ippolito, Richard Dubos, Roxane Dumont, Nacira El Merjani, Antoine Flahault, Natalie Francioli, Clément Graindorge, Idris Guessous, Séverine Harnal, Samia Hurst, Laurent Kaiser, Gabriel Kathari, Omar Kherad, Julien Lamour, Pierre Lescuyer, Arnaud G. L’Huillier, Andrea Jutta Loizeau, Elsa Lorthe, Chantal Martinez, Shannon Mechoullam, Ludovic Metral-Boffod, Mayssam Nehme, Natacha Noël, Francesco Pennacchio, Didier Pittet, Klara M. Posfay-Barbe, Géraldine Poulain, Caroline Pugin, Nick Pullen, Viviane Richard, Déborah Rochat, Khadija Samir, Hugo Santa Ramirez, Etienne Satin, Philippe Schaller, Stephanie Schrempft, Claire Semaani, Silvia Stringhini, Stéphanie Testini, Anshu Uppal, Déborah Urrutia-Rivas, Charlotte Verolet, Pauline Vetter, Jennifer Villers, Guillemette Violot, Nicolas Vuilleumier, Ania Wisniak, Sabine Yerly, and María-Eugenia Zaballa.
Author contributions: CF was involved in conceptualisation, formal analysis, methodology and writing the original draft; NP was involved in conceptualisation, data curation, formal analysis, methodology, supervision, and writing, reviewing and editing the manuscript; HB was involved in investigation, project administration, conceptualisation, and writing, reviewing and editing the manuscript; MEZ was involved in conceptualisation, project administration, and reviewing and editing the manuscript; FP was involved in software implementation, data curation and reviewing and editing the manuscript; SS was involved in investigation and reviewing and editing the manuscript; SL was involved in conceptualisation, investigation, and reviewing and editing the manuscript; MN was involved in reviewing and editing the manuscript; IG was involved in conceptualisation, funding acquisition, project administration, and reviewing and editing the manuscript; SS was involved in conceptualisation, investigation, funding acquisition, project administration, and reviewing and editing the manuscript; EL was involved in conceptualisation, methodology, supervision, writing, and reviewing and editing the manuscript.
Declaration of Generative AI and AI-assisted technologies in the writing process: During the preparation of this work, the authors used AI-assisted technologies to improve readability and language. After using these tools, the authors reviewed and edited the content as needed and take full responsibility for the manuscript’s content.
This work was supported by the Swiss Federal Office of Public Health; the General Directorate of Health of the Department of Safety, Employment and Health of the Canton of Geneva; the Private Foundation of the Geneva University Hospitals; the Swiss School of Public Health (Corona Immunitas Research Programme); and the Fondation des Grangettes. Award/Grant numbers are not applicable.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Parsons S, Maddock J, Di Gessa G, Green MJ, Thompson EJ, Stevenson AJ, et al. Health care disruption inequalities during Covid-19: Evidence from eleven longitudinal studies. European Journal of Public Health. 2021;31(Supplement_3):ckab164.18. DOI:
2. Di Gessa G, Price D. Changes in health and social well-being in the COVID-19 clinically vulnerable older English population during the pandemic. J Epidemiol Community Health. 2021 Nov;75(11):1070–7. doi: https://doi.org/10.1136/jech-2021-216405
3. Vloo A, Alessie RJ, Mierau JO, Boezen MH, Mierau JO, Franke L, et al.; Lifelines Corona Research Initiative. Gender differences in the mental health impact of the COVID-19 lockdown: longitudinal evidence from the Netherlands. SSM Popul Health. 2021 Jul;15:100878. doi: https://doi.org/10.1016/j.ssmph.2021.100878
4. Park SS. Caregivers’ Mental Health and Somatic Symptoms During COVID-19. The Journals of Gerontology: Series B. 2021;76(4):e235-e40.
5. Cohen G, Russo MJ, Campos JA, Allegri RF. Living with dementia: increased level of caregiver stress in times of COVID-19. Int Psychogeriatr. 2020 Nov;32(11):1377–81. doi: https://doi.org/10.1017/S1041610220001593
6. Cona MS, Rulli E, Dalu D, Galli F, Rota S, Ferrario S, et al. The emotional impact of the COVID-19 outbreak on cancer outpatients and their caregivers: results of a survey conducted in the midst of the Italian pandemic. Support Care Cancer. 2022 Feb;30(2):1115–25. doi: https://doi.org/10.1007/s00520-021-06489-y
7. Commission E. Directorate-General for Employment SA, Inclusion, Zigante V. Informal care in Europe : exploring formalisation, availability and quality. Publications Office; 2018.
8. Verbakel E. How to understand informal caregiving patterns in Europe? The role of formal long-term care provisions and family care norms. Scand J Public Health. 2018 Jun;46(4):436–47. doi: https://doi.org/10.1177/1403494817726197
9. Tur-Sinai A, Teti A, Rommel A, Hlebec V, Lamura G. How Many Older Informal Caregivers Are There in Europe? Comparison of Estimates of Their Prevalence from Three European Surveys. Int J Environ Res Public Health. 2020 Dec;17(24):9531. doi: https://doi.org/10.3390/ijerph17249531
10. Verbakel E, Tamlagsrønning S, Winstone L, Fjær EL, Eikemo TA. Informal care in Europe: findings from the European Social Survey (2014) special module on the social determinants of health. Eur J Public Health. 2017 Feb;27 suppl_1:90–5. doi: https://doi.org/10.1093/eurpub/ckw229
11. Guttierrez VB, Clausen F, Chiolero A. Estimating the number of informal caregivers in one region of Switzerland: a population-based study: Arnaud Chiolero. European Journal of Public Health. 2017;27(suppl_3).
12. Chan EY, Gobat N, Kim JH, Newnham EA, Huang Z, Hung H, et al. Informal home care providers: the forgotten health-care workers during the COVID-19 pandemic. Lancet. 2020 Jun;395(10242):1957–9. doi: https://doi.org/10.1016/S0140-6736(20)31254-X
13. State of Caring. A snapshot of unpaid care in the UK. Report. Carers UK, 2019 July 2019. Report No. Available from: https://www.carersuk.org/media/khgkb3fs/state-of-caring-2019-report.pdf
14. Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychol Bull. 2003 Nov;129(6):946–72. doi: https://doi.org/10.1037/0033-2909.129.6.946
15. Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol Aging. 2003 Jun;18(2):250–67. doi: https://doi.org/10.1037/0882-7974.18.2.250
16. Hanff AM, Pauly C, Pauly L, Schröder VE, Hansen M, Meyers GR, et al. Unmet Needs of People With Parkinson’s Disease and Their Caregivers During COVID-19-Related Confinement: An Explorative Secondary Data Analysis. Front Neurol. 2021 Jan;11:615172.
17. Prins M, Willemse B, van der Velden C, Pot AM, van der Roest H. Involvement, worries and loneliness of family caregivers of people with dementia during the COVID-19 visitor ban in long-term care facilities. Geriatr Nurs. 2021;42(6):1474–80. doi: https://doi.org/10.1016/j.gerinurse.2021.10.002
18. Irani E, Niyomyart A, Zauszniewski JA. Caregiving Stress and Self-Rated Health during the COVID-19 Pandemic: The Mediating Role of Resourcefulness. Issues Ment Health Nurs. 2021 Nov;42(11):982–8. doi: https://doi.org/10.1080/01612840.2021.1924324
19. Lightfoot E, Moone R, Suleiman K, Otis J, Yun H, Kutzler C, et al. Concerns of Family Caregivers during COVID-19: The Concerns of Caregivers and the Surprising Silver Linings. J Gerontol Soc Work. 2021 Sep;64(6):656–75. doi: https://doi.org/10.1080/01634372.2021.1898512
20. Darlington AE, Morgan JE, Wagland R, Sodergren SC, Culliford D, Gamble A, et al. COVID-19 and children with cancer: Parents’ experiences, anxieties and support needs. Pediatr Blood Cancer. 2021 Feb;68(2):e28790. doi: https://doi.org/10.1002/pbc.28790
21. Zhao R, Zhou Q, Wang XW, Liu CH, Wang M, Yang Q, et al. COVID-19 Outbreak and Management Approach for Families with Children on Long-Term Kidney Replacement Therapy. Clin J Am Soc Nephrol. 2020 Sep;15(9):1259–66. doi: https://doi.org/10.2215/CJN.03630320
22. Willner P, Rose J, Stenfert Kroese B, Murphy GH, Langdon PE, Clifford C, et al. Effect of the COVID-19 pandemic on the mental health of carers of people with intellectual disabilities. J Appl Res Intellect Disabil. 2020 Nov;33(6):1523–33. doi: https://doi.org/10.1111/jar.12811
23. Beach SR, Schulz R, Donovan H, Rosland AM. Family Caregiving During the COVID-19 Pandemic. Gerontologist. 2021 Jul;61(5):650–60. doi: https://doi.org/10.1093/geront/gnab049
24. Anderson S, Parmar J, Dobbs B, Tian PG. A Tale of Two Solitudes: Loneliness and Anxiety of Family Caregivers Caring in Community Homes and Congregate Care. Int J Environ Res Public Health. 2021 Sep;18(19):10010. doi: https://doi.org/10.3390/ijerph181910010
25. Hughes MC, Liu Y, Baumbach A. Impact of COVID-19 on the Health and Well-being of Informal Caregivers of People with Dementia: A Rapid Systematic Review. Gerontol Geriatr Med. 2021 May;7:23337214211020164. doi: https://doi.org/10.1177/23337214211020164
26. van Gorp M, Maurice-Stam H, Teunissen LC, van de Peppel-van der Meer W, Huussen M, Schouten-van Meeteren AY, et al. No increase in psychosocial stress of Dutch children with cancer and their caregivers during the first months of the COVID-19 pandemic. Pediatr Blood Cancer. 2021 Feb;68(2):e28827. doi: https://doi.org/10.1002/pbc.28827
27. Baysson H, Pennachio F, Wisniak A, Zabella ME, Pullen N, Collombet P, et al.; Specchio-COVID19 study group. Specchio-COVID19 cohort study: a longitudinal follow-up of SARS-CoV-2 serosurvey participants in the canton of Geneva, Switzerland. BMJ Open. 2022 Jan;12(1):e055515. doi: https://doi.org/10.1136/bmjopen-2021-055515
28. Stringhini S, Wisniak A, Piumatti G, Azman AS, Lauer SA, Baysson H, et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): a population-based study. Lancet. 2020 Aug;396(10247):313–9. doi: https://doi.org/10.1016/S0140-6736(20)31304-0
29. Stringhini S, Zaballa ME, Perez-Saez J, Pullen N, de Mestral C, Picazio A, et al.; Specchio-COVID19 Study Group. Seroprevalence of anti-SARS-CoV-2 antibodies after the second pandemic peak. Lancet Infect Dis. 2021 May;21(5):600–1. doi: https://doi.org/10.1016/S1473-3099(21)00054-2
30. West EA, Anker D, Amati R, Richard A, Wisniak A, Butty A, et al.; Corona Immunitas Research Group. Corona Immunitas: study protocol of a nationwide program of SARS-CoV-2 seroprevalence and seroepidemiologic studies in Switzerland. Int J Public Health. 2020 Dec;65(9):1529–48. doi: https://doi.org/10.1007/s00038-020-01494-0
31. Stringhini S, Zaballa ME, Pullen N, de Mestral C, Perez-Saez J, Dumont R, et al.; SEROCoV-WORK + Study Group. Large variation in anti-SARS-CoV-2 antibody prevalence among essential workers in Geneva, Switzerland. Nat Commun. 2021 Jun;12(1):3455. doi: https://doi.org/10.1038/s41467-021-23796-4
32. Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997 Jan;27(1):191–7. doi: https://doi.org/10.1017/S0033291796004242
33. Lundin A, Hallgren M, Theobald H, Hellgren C, Torgén M. Validity of the 12-item version of the General Health Questionnaire in detecting depression in the general population. Public Health. 2016 Jul;136:66–74. doi: https://doi.org/10.1016/j.puhe.2016.03.005
34. Genecand C, Mongin D, Koegler F, Lebowitz D, Regard S, Falcone JL, et al. Cohort profile: Actionable Register of Geneva Outpatients and inpatients with SARS-CoV-2 (ARGOS). BMJ Open. 2021 Nov;11(11):e048946. doi: https://doi.org/10.1136/bmjopen-2021-048946
35. van Buuren S. Flexible Imputation of Missing Data. 2nd ed. Chapman and Hall/CRC; 2018. 444 pp., Available from https://www.taylorfrancis.com/books/edit/10.1201/9780429492259/flexible-imputation-missing-data-second-edition-stef-van-buuren
36. Taniguchi Y, Miyawaki A, Tsugawa Y, Murayama H, Tamiya N, Tabuchi T. Family caregiving and changes in mental health status in Japan during the COVID-19 pandemic. Arch Gerontol Geriatr. 2022;98:104531. doi: https://doi.org/10.1016/j.archger.2021.104531
37. Czeisler MÉ, Drane A, Winnay SS, Capodilupo ER, Czeisler CA, Rajaratnam SM, et al. Mental health, substance use, and suicidal ideation among unpaid caregivers of adults in the United States during the COVID-19 pandemic: relationships to age, race/ethnicity, employment, and caregiver intensity. J Affect Disord. 2021 Dec;295:1259–68. doi: https://doi.org/10.1016/j.jad.2021.08.130
38. Bergmann M, Wagner M. The Impact of COVID-19 on Informal Caregiving and Care Receiving Across Europe During the First Phase of the Pandemic. Front Public Health. 2021 Jun;9(590):673874. doi: https://doi.org/10.3389/fpubh.2021.673874
39. McLennon SM, Lekhak N. “A World Upside Down”: Experiences of Informal Caregivers During the COVID-19 Pandemic. J Gerontol Nurs. 2021 Nov;47(11):11–4. doi: https://doi.org/10.3928/00989134-20211012-02
40. Roth DL, Fredman L, Haley WE. Informal caregiving and its impact on health: a reappraisal from population-based studies. Gerontologist. 2015 Apr;55(2):309–19. doi: https://doi.org/10.1093/geront/gnu177
41. Spillman BC, Wolff J, Freedman VA, Kasper JD. Informal caregiving for older Americans: An analysis of the 2011 National Study of Caregiving. Washington (DC): Office of the Assistant Secretary for Planning and Evaluation; 2014., Available from https://aspe.hhs.gov/reports/informal-caregiving-older-americans-analysis-2011-national-study-caregiving
42. Navaie-Waliser M, Feldman PH, Gould DA, Levine C, Kuerbis AN, Donelan K. When the caregiver needs care: the plight of vulnerable caregivers. Am J Public Health. 2002 Mar;92(3):409–13. doi: https://doi.org/10.2105/AJPH.92.3.409
43. Shikimoto R, Sado M, Ninomiya A, Yoshimura K, Ikeda B, Baba T, et al. Predictive factors associated with psychological distress of caregivers of people with dementia in Japan: a cross-sectional study. Int Psychogeriatr. 2018 Aug;30(8):1089–98. doi: https://doi.org/10.1017/S1041610217002289
44. George ES, Kecmanovic M, Meade T, Kolt GS. Psychological distress among carers and the moderating effects of social support. BMC Psychiatry. 2020 Apr;20(1):154. doi: https://doi.org/10.1186/s12888-020-02571-7
45. Hoffman GJ, Wallace SP. The Cost of Caring: Economic Vulnerability, Serious Emotional Distress, and Poor Health Behaviors Among Paid and Unpaid Family and Friend Caregivers. Res Aging. 2018 Sep;40(8):791–809. doi: https://doi.org/10.1177/0164027517742430
46. UK C. Caring behind closed doors — Forgotten families in the coronavirus outbreak. 2020. Available from : https://www.carersuk.org/reports/caring-behind-closed-doors-forgotten-families-in-the-coronavirus-outbreak/
47. Monteiro S, Fournier M, Favrod J, Drainville AL, Plessis L, Freudiger S, et al. Ability to Care for an Ill Loved One During the First COVID-19 Lockdown: Mediators of Informal Caregivers’ Stress in Europe. Front Psychiatry. 2022 Apr;13:852712. doi: https://doi.org/10.3389/fpsyt.2022.852712
48. Anjara SG, Bonetto C, Van Bortel T, Brayne C. Using the GHQ-12 to screen for mental health problems among primary care patients: psychometrics and practical considerations. Int J Ment Health Syst. 2020 Aug;14(1):62. doi: https://doi.org/10.1186/s13033-020-00397-0
49. Weber M, Burchert S, Sijbrandij M, Patanè M, Pinucci I, Renneberg B, et al. Mental health across two years of the COVID-19 pandemic: a 5-wave longitudinal study in Germany. Front Psychiatry. 2023 Aug;14:1229700. doi: https://doi.org/10.3389/fpsyt.2023.1229700
50. Reinikainen J, Tolonen H, Borodulin K, Härkänen T, Jousilahti P, Karvanen J, et al. Participation rates by educational levels have diverged during 25 years in Finnish health examination surveys. Eur J Public Health. 2018 Apr;28(2):237–43. doi: https://doi.org/10.1093/eurpub/ckx151
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.3884.