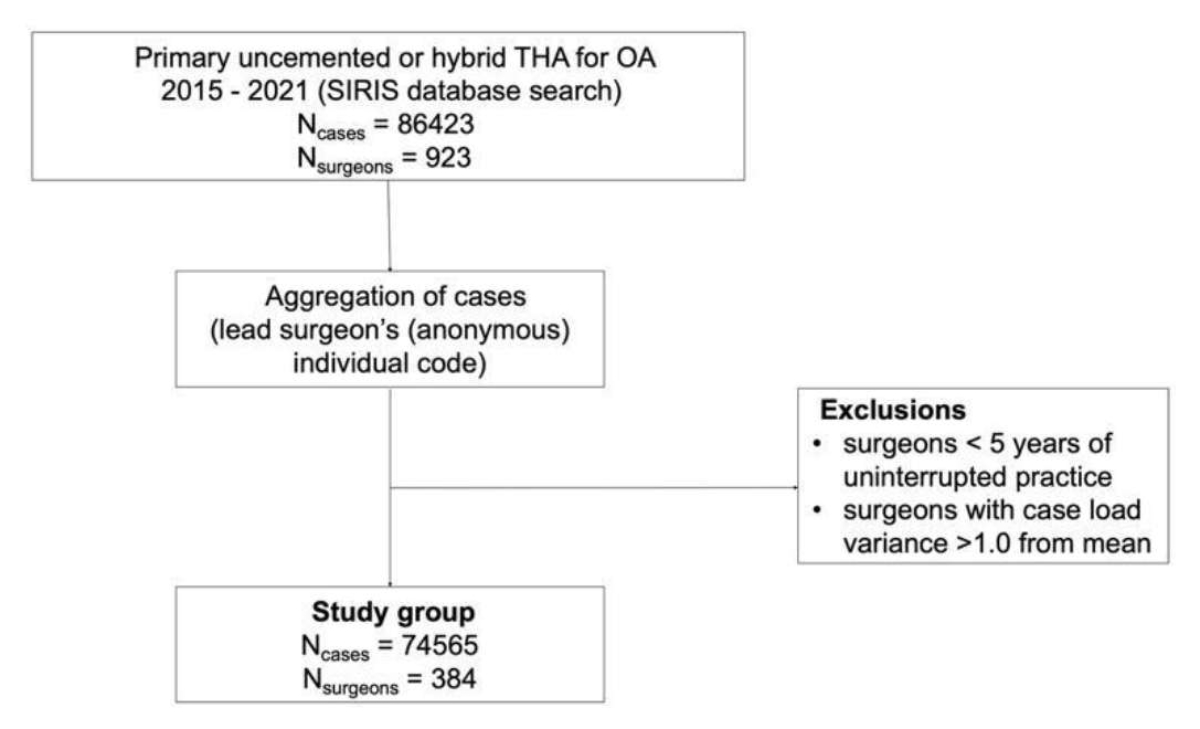
Figure 1Flowchart on data extraction and participant selection. OA: osteoarthritis; THA: total hip arthroplasty.
DOI: https://doi.org/https://doi.org/10.57187/s.3850
Total hip arthroplasty successfully reduces pain and restores joint function in end-stage osteoarthritis [1, 2]. Peri- and postoperative complications such as dislocation, loosening, periprosthetic fracture or infection occur infrequently, yet further reduction of these complications remains an important factor for enhancing patient outcome, reducing revision burden and improving the cost-effectiveness of the procedure [1]. The last point is especially important in light of the considerable healthcare expense associated with the increasing demand for total hip arthroplasty [3, 4].
Higher surgeon volume has been shown to be clearly associated with improved patient outcomes and decreased complications in hip replacement surgery [1, 2, 5–8]. This volume-outcome relationship has induced centralisation in medical care, and the introduction of minimum volume regulations [1, 8–13]. To date, minimum volume standards have been set normatively as a precondition for hospitals to perform procedures and to claim reimbursement in various countries, such as Australia, Canada, England, France, Germany, Italy and the USA [1, 6–8, 14].
Even though minimum volume standards have been proven effective in reducing revision rates following total hip arthroplasty, their strict application is often complicated due to limited practical applicability [1, 9, 15]. Raising the minimum volume standard progressively excludes low-volume surgeons (and low-volume hospitals) from the healthcare supply, which may challenge the ability of the remaining surgeons (or hospitals) to meet treatment need [11, 15]. It also causes a significant patient shift, meaning that patients from low-volume surgeons who may no longer offer certain treatments due to minimum volume standard regulations would need to find a new surgeon (i.e. they need to be reassigned). Hence patients may experience additional stress by having to potentially accept a longer wait or travel a greater distance to access high-volume healthcare providers, which in turn may interfere with the overall patient experience.
Due to large differences between the various national healthcare systems worldwide and differing minimum volume standard regulations, existing international studies may have limited validity and applicability to particular local healthcare environments.
The aim of this registry-based study was to assess the relation of surgeons’ case load (= number of procedures per year) on short-term revision rates (within two years of the index procedure) in patients undergoing primary total hip arthroplasty for hip osteoarthritis in Switzerland. In addition, the effects of increasing minimum volume standard thresholds on the potential reduction of revision burden was simulated.
The hypothesis was that the surgeons’ case load was inversely associated with the revision risk in patients undergoing primary total hip arthroplasty for hip osteoarthritis in Switzerland.
A retrospective study was conducted using data from the Swiss National Implant Registry (SIRIS). The registry was implemented in 2012 and collects data from all primary and revision hip arthroplasty procedures in Switzerland. The dataset includes patient characteristics (sex, age, height, weight, ASA score and Charnley score); diagnosis; type, date and technical aspects (surgical approach and positioning) of the procedure; surgeon; and clinic. The reported nationwide coverage of SIRIS for primary total hip arthroplasty was 98% in 2021 [16]. Consistency and completeness of the data are ascertained through regular validation tests. For this study, an anonymised dataset (irreversibly coded patient, surgeon and hospital identifications) containing information from all primary uncemented or hybrid (i.e. uncemented cup, cemented stem) total hip arthroplasties (equalling 98.5% of all total hip arthroplasties) between 2015 and 2021, was provided to the research group, following a formal request to the scientific advisory board of SIRIS and their approval. This study was approved by the local ethics committee, which issued a waiver because the dataset was anonymised.
The data extraction flowchart is depicted in figure 1. Only adult patients (³18 years) were considered. In order to ensure data consistency, subjects having undergone concomitant interventions at the time of index total hip arthroplasty were excluded, whereas those aged >100 years, those with BMI <12 or >60 or those with an ASA score >4 were removed for plausibility reasons.
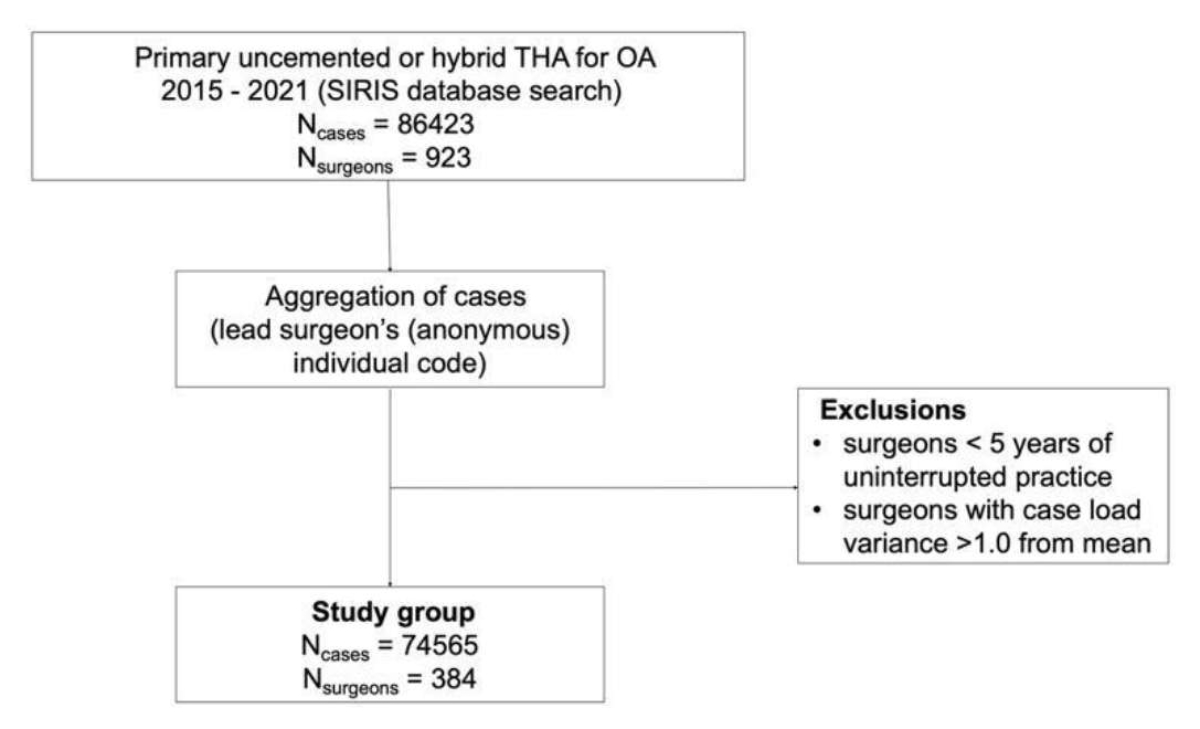
Figure 1Flowchart on data extraction and participant selection. OA: osteoarthritis; THA: total hip arthroplasty.
The surgeon’s case load was added as a numerical variable to each individual case. Surgeons’ case load was defined as the number of primary total hip arthroplasties performed by the individual surgeon per year, and represents the surgeon’s mean annual case load over the observational period. To ensure homogeneous and comparable surgeon case load information, only surgeons with uninterrupted practice of at least 5 years (within an observation period of 7 years) and a case load variance within the observation period of <1.0 were considered. Since this method of assessing surgeons’ case load has not been published before, a sensitivity analysis on the complete dataset was performed post-hoc in order to rule out any selection bias deriving from the application of our surgeon eligibility criteria.
The primary outcome parameter was revision for any reason within two years of the index procedure, and the surgeons’ case load was the main predictor for assessing our primary outcome. The patient’s age and sex, BMI, ASA and the type of implant fixation were co-variates of interest. Secondary outcome parameters were revision for specific reasons, i.e. revision for infection, dislocation, periprosthetic fracture and aseptic loosening, for both the femoral and acetabular components.
All statistical analyses were performed using R (R: A language and environment for statistical computing, R Foundation for Statistical Computing, Vienna, Austria). Descriptive statistics included means, standard deviations, ranges and proportions. Comparative statistics included the t-test and the chi-squared test. The confidence level for rejecting null hypotheses was set at 95% (p-value <0.05). Multiple logistic and bivariate multinomial regressions were employed to model the odds of revision surgery as a function of surgeon case load.
Using a numeric simulation, the effect of discrete minimum volume standard thresholds (i.e. 10, 20 and 50 total hip arthroplasties per surgeon per year) on total hip arthroplasty revision rates within two years of index procedure was explored. The portion of patients below each threshold was given the revision rate of remaining patients above the specific threshold, allowing the calculation and plotting of theoretical differences in revision rates for each particular threshold. As the minimum volume standard rose, low-volume surgeons would progressively lose the licence to perform total hip arthroplasty, and an increasing number of patients would need to find a new surgeon (i.e. they would need to be “reassigned”). In order to put this phenomenon into perspective, the number of patients needing treatment reassignment was calculated for each minimum volume standard threshold.
A total of 74,565 eligible patients with a mean age of 68.8 years was identified (51.2% female). The sensitivity analysis showed that no relevant selection bias had been introduced through application of our surgeon eligibility criteria (figure 2). The surgical procedures in this cohort were performed by 384 surgeons. The mean surgeon case load was 28.7, ranging from 1.8 to 269.1. The mean 2-year revision rate in the cohort was 2.25%. Demographic data are presented in detail in table 1.
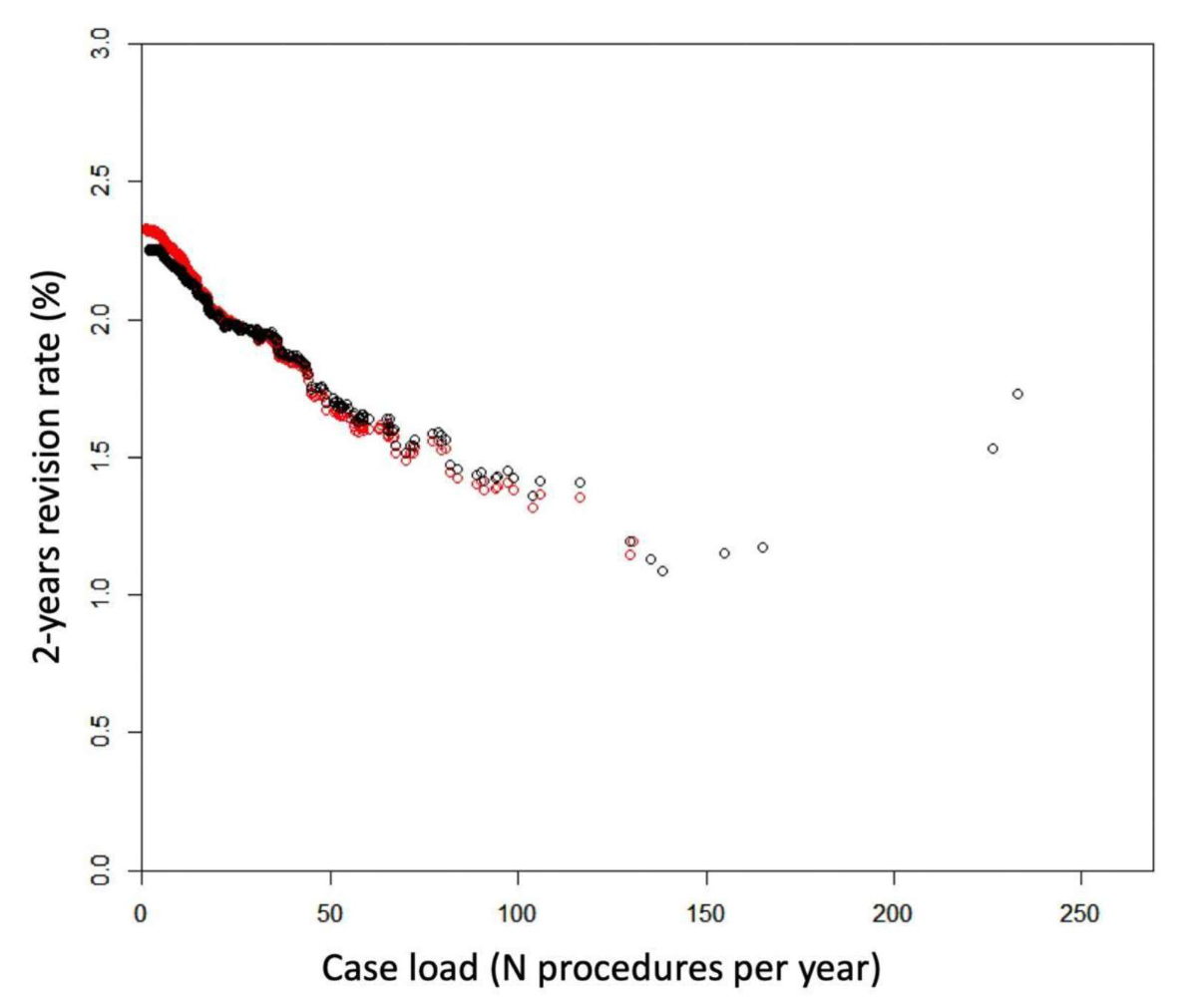
Figure 2Association between surgeon case load and 2-year revision rate, comparing the datasets before (RED) and after (BLACK) application of our surgeon eligibility criteria. The sensitivity analysis shows an association between both graphs, excluding any selection bias from the application of our eligibility criteria.
Table 1Demographics.
| Cases (n) | 74,565 | |
| Female | 38,154 (51.2%) | |
| Male | 36,411 (48.8%) | |
| Age, in years | Mean (range) | 68.8 (18–99) |
| Surgeons (n) | 384 | |
| Surgeon case load | Mean (range) | 28.7 (1.8–269.1) |
| Median | 18.1 | |
| 2-year revision rate | 2.25% | |
Using multiple logistic regression, surgeon case load was identified as a highly significant and independent predictor (p <0.001, odds ratio [OR] 0.995, 95% confidence interval [CI] 0.994–0.996) of any-cause revision in patients undergoing primary total hip arthroplasty for hip osteoarthritis. Higher case load was associated with a lower 2-year revision rate, and a nearly linear correlation was found (figure 3). The patient’s morbidity state (p <0.001, OR 1.293) and BMI (p <0.001, OR 1.047) were identified as additional independent risk factors determining revision within two years, while the patient’s sex, age and the method of femoral fixation (uncemented vs hybrid) were not.
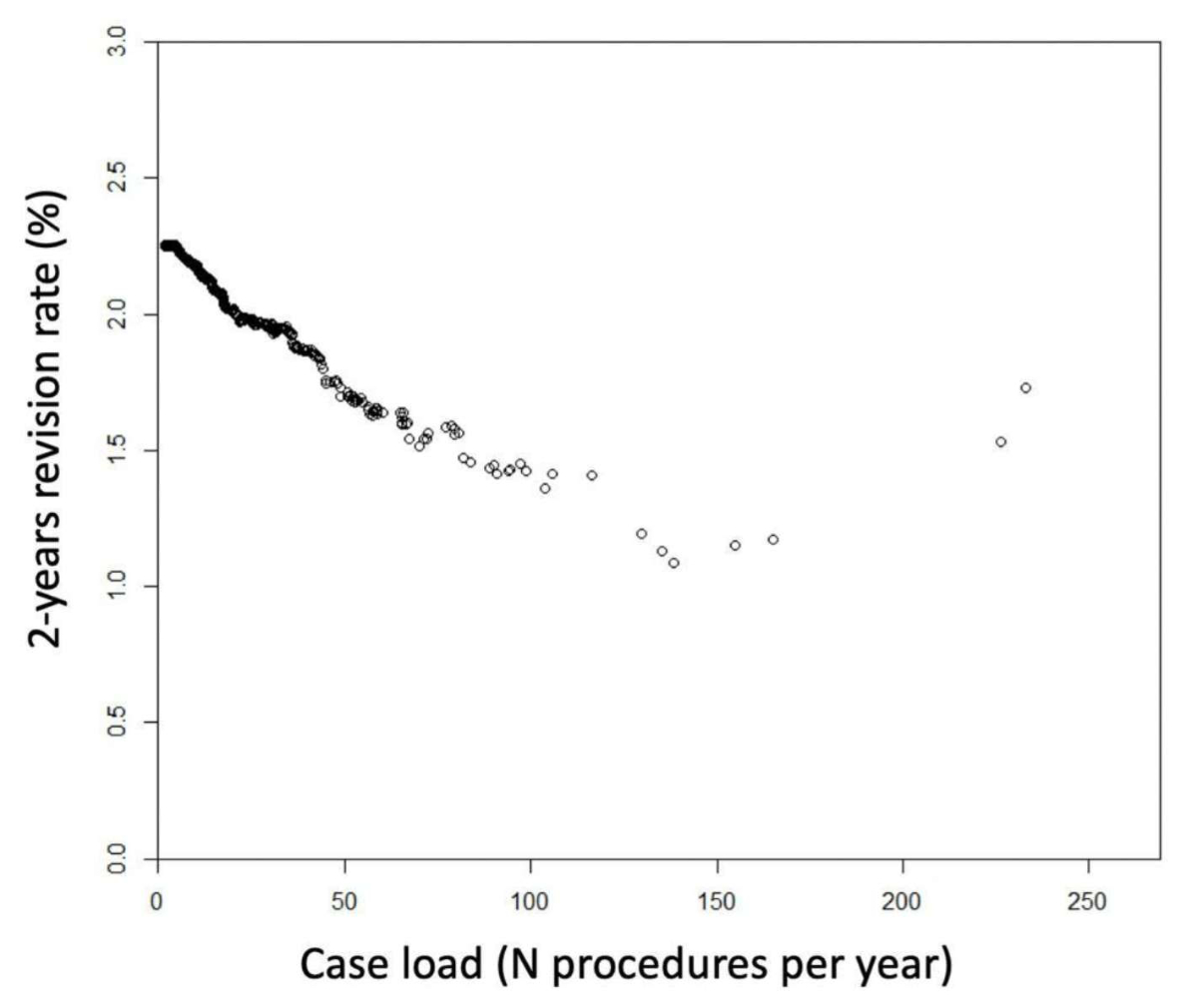
Figure 3Association between surgeon case load and 2-year revision rate.
Multinomial bivariate regression revealed that higher surgeon case load was associated with lower risk of total hip arthroplasty revision due to infection, dislocation and femoral periprosthetic fracture. Revisions for acetabular periprosthetic fractures and loosening of the femoral or acetabular component were not associated with the surgeon case load (table 2).
Table 2Association between surgeon case load and total hip arthroplasty revision (revision for any reason and for infection, dislocation, periprosthetic fracture and aseptic loosening).
| Reason for revision (Base: no revision) | p value (surgeon case load) | Odds ratio (95% CI) |
| Any reason | <0.001 | 0.995 (0.994–0.996) |
| Infection | <0.001 | 0.996 (0.995–0.997) |
| Dislocation | <0.001 | 0.988 (0.986–0.990) |
| Periprosthetic fracture (femoral) | <0.001 | 0.995 (0.994–0.996) |
| Periprosthetic fracture (acetabular) | 0.55 | 0.998 (0.994–1.002) |
| Aseptic loosening (femoral) | 0.78 | 1.000 (0.999–1.001) |
| Aseptic loosening (acetabular) | 0.095 | 0.997 (0.997–0.999) |
CI: confidence interval.
Detailed information on the impact of a potential minimum case load on revision rates, the overall reduction of expected revisions and the number of patients needing treatment reassignment for each minimum volume standard threshold is provided in table 3 and figures 4 and 5. Implementation of a minimum volume standard threshold of 10 total hip arthroplasties / surgeon / year would only have a negligible impact on the 2-year revision rate (reduction from 2.25% to 2.18%) and avoid 3.2% of revisions. This effect was far more pronounced with higher minimum volume standard thresholds. A minimum case load of 50 total hip arthroplasties / surgeon / year would result in a 2-year revision rate of 1.7% (avoiding 23.8% of revisions), but at the cost of 53.8% patients needing treatment reassignment each year.
Table 3Impact of various minimum volume standard thresholds on 2-year revision rate, reduction of revision risk and percentage of patients needing treatment reassignment.
| Minimum volume standard | 2-year revision rate | % reduction of revisions | % patients reassigned |
| 10 | 2.18% | 3.2% | 5.1% |
| 20 | 2.01% | 10.5% | 18.1% |
| 50 | 1.7% | 23.8% | 53.8% |
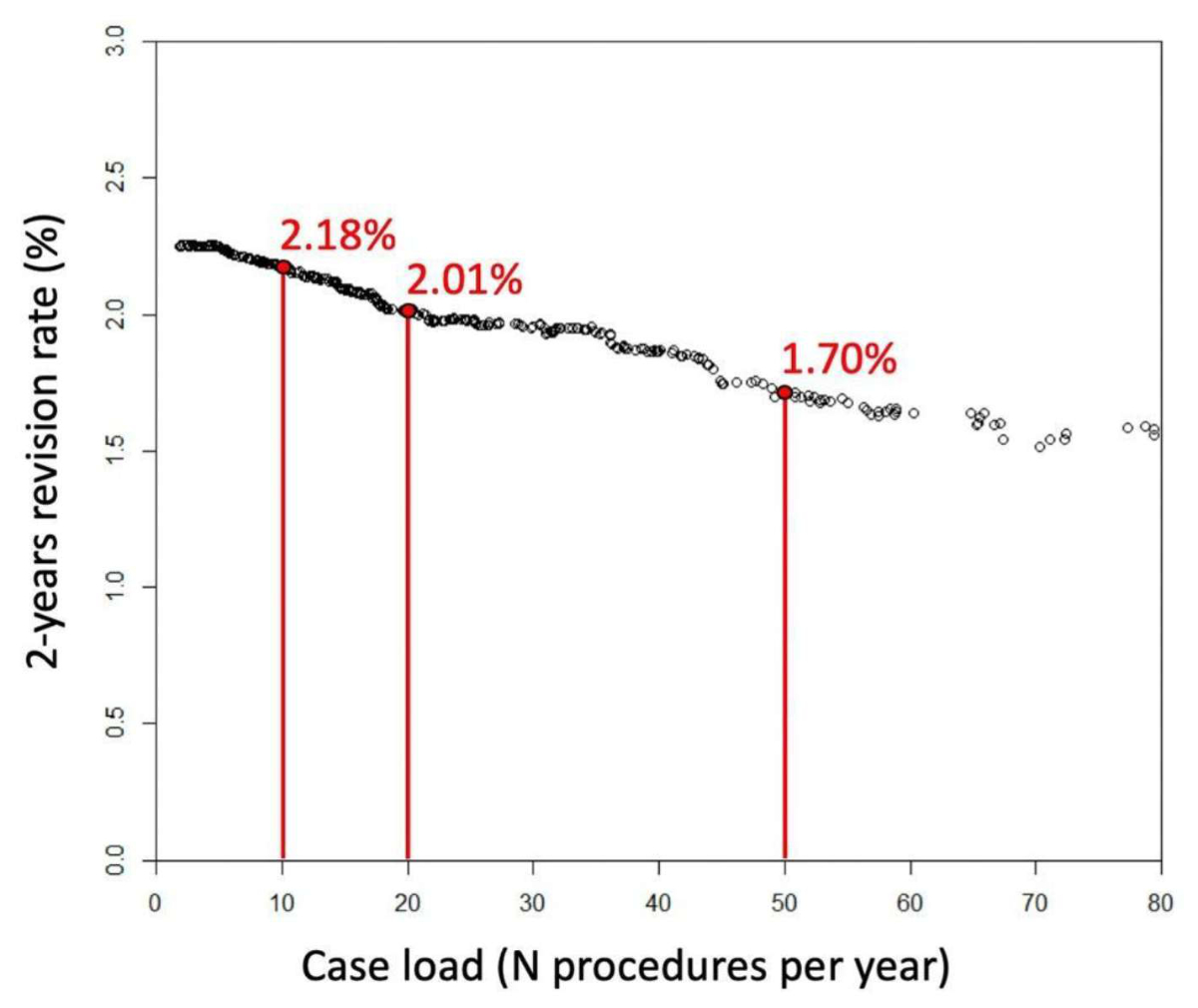
Figure 4Estimated 2-year revision rates on implementation of minimum volume standard thresholds of 10, 20 or 50 total hip arthroplasties / surgeon / year.
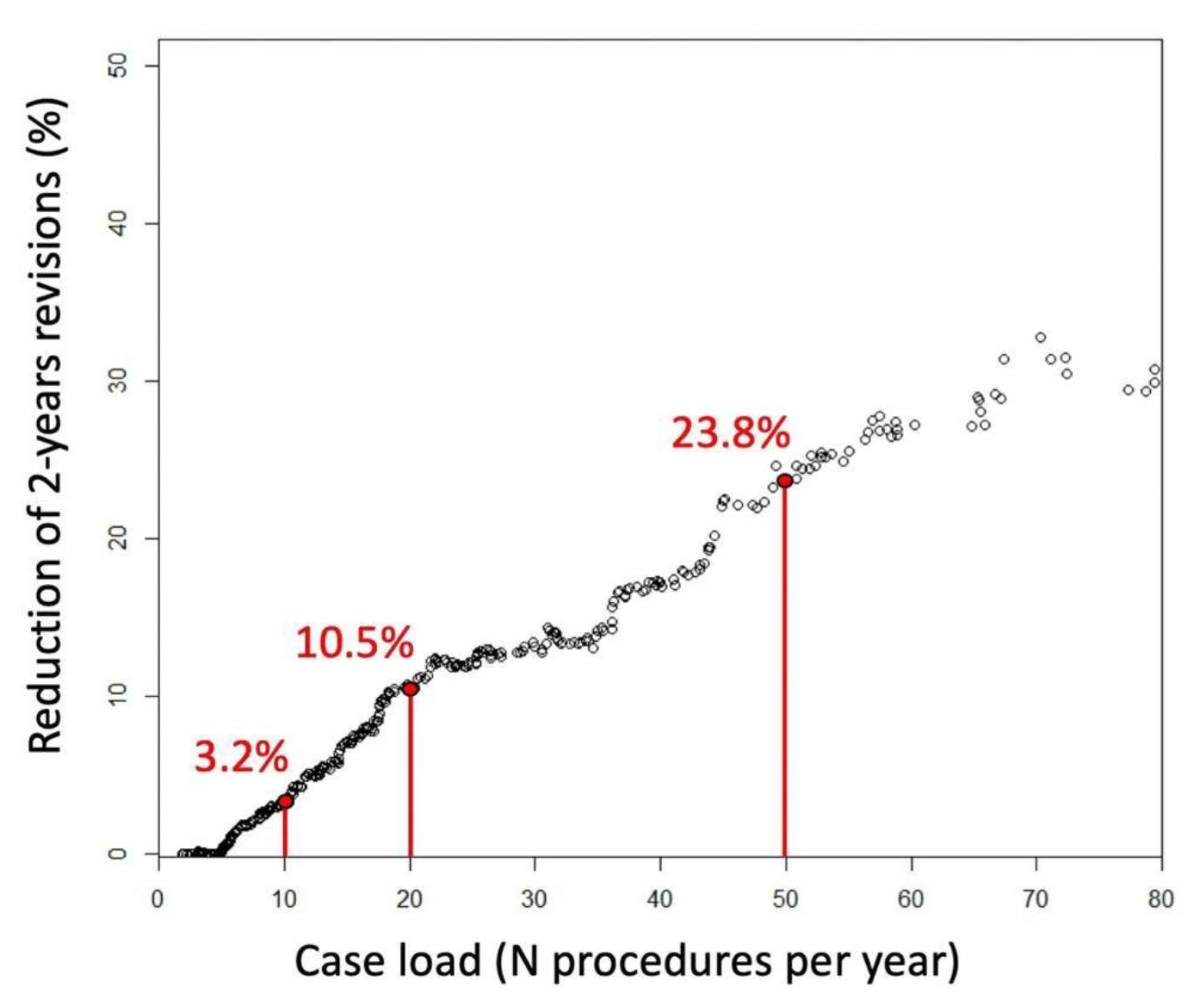
Figure 5Estimated reduction of revision burden following implementation of minimum volume standard thresholds of 10, 20 or 50 total hip arthroplasties / surgeon / year (base: the total number of revisions without minimum volume standard implementation).
The main finding of this study is that higher surgeon case load is associated with a substantially decreased risk of any-cause revision in patients undergoing primary total hip arthroplasty for hip osteoarthritis in Switzerland. The main strengths of the study are the large sample size and virtually complete registry coverage due to nationwide compulsory registration of total hip arthroplasty in the Swiss National Joint Registry (SIRIS). The results are representative of the practice of Swiss orthopaedic surgeons, and may primarily be used for planning or modification of minimum volume standards in Switzerland. However, these findings are probably applicable to other countries with similar healthcare systems. Our finding of a strong volume-outcome relationship in total hip arthroplasty is in line with the current literature [1, 2, 7, 17]. The lower overall revision risk resulted from fewer revisions due to dislocation, infection and femoral periprosthetic fractures. An increased risk of total hip arthroplasty dislocation has been reported in the literature for subjects operated on by low-volume surgeons. Ravi et al. [6] found that dislocation rates within two years of the index procedure were higher in total hip arthroplasty recipients whose surgeons had carried out fewer than 35 procedures per year than in those operated on by surgeons performing more than 35 total hip arthroplasties annually (1.9% vs 1.3%, p=0.006). Similarly, Battaglia et al. [18] summarised in a systematic review that a higher surgeon case load led to lower dislocation rates. Dislocation has been associated with component malpositioning [19, 20], and surgical outliers in implant positioning reportedly occur more commonly in total hip arthroplasties performed by low-volume surgeons [21], leading to the assumption that a higher case load could enable more accurate implant positioning.
Revision due to infection and periprosthetic fractures were also associated with a lower surgeon case load in our study. Mufarrih et al. [17] found a positive association between lower case load and higher risk of infection in total hip arthroplasty, but they had analysed the hospital case load rather than the surgeon case load. Siddiqi et al. [1] stated that low surgeon case load had the greatest link with early revisions due to infection after total hip arthroplasty, irrespective of the hospital volume, which is in line with our findings.
According to our results, implementing a minimum volume standard is a suitable measure for substantially decreasing revision rates following total hip arthroplasty. Unlike previous publications [6, 9], there was no inflection point in the volume / outcome curve in our study, meaning that no optimal threshold could be established to discriminate between low-volume and high-volume surgeons. This is potentially due to a different method of analysis. However, Sayers et al. also reported a linear decrease of the revision rate with increasing case load [11]. The lack of a numerically optimal threshold value was the reason for choosing arbitrary but pragmatic minimum volume standard thresholds in our simulation.
In general, minimum volume standard thresholds should aim to strike a balance, i.e. to achieve clinically meaningful improvements and applicability within a given healthcare environment without substantially interfering with the patients’ demand for geographically close and timely access to medical care. In our analysis, a minimum volume standard threshold of 20 total hip arthroplasties / year would lead to a 10.5% reduction in revisions within two years, which can be regarded as clinically relevant. These calculations do not include the positive effect that each specific minimum volume standard generates by the increased case load of the remaining licensed surgeons. It is of note that 18.1% of patients would need to be reassigned as an effect of this arbitrarily chosen minimum volume standard threshold. In a small country with a high density of orthopaedic surgeons per 1000 inhabitants, travelling distances are likely to remain a minor problem for patients, while the impact of minimum volume standards on the waiting time due to capacity issues of the remaining licensed surgeons warrants further research.
This study has several limitations. From a methodological point of view, the causality between surgeon case load and revision rates is not irrefutably proven. The surgeon case load could be a reflection of each surgeon’s own skills. Potentially, physicians with better outcomes have a higher surgeon case load because patients seek out care at these more reputable surgeons. Inversely, surgeons with increased complication rates could opt to perform fewer total hip arthroplasties in response. It is important to acknowledge that several patient-, hospital- or surgeon-related factors throughout the pre-, peri- and postoperative pathway may interfere with the association found.
The minimum volume standard thresholds analysed in this study (10 / 20 / 50 total hip arthroplasties / year) were chosen arbitrarily. This was deemed adequate since the relationship between surgeon case load and revision rate was linear, and this practice was in line with current literature [22].
Furthermore, the 2-year revision rates analysed here represent only a short period within the expected total survival time, and the effect of surgeon case load on longer-term outcomes is unclear. However, previous research suggests that patients treated by low-volume surgeons are also at higher risk of complications occurring several years after the procedure [23].
Finally, our research focused on revision rates and did not assess other outcome quality indicators, like patient travel time, hospital characteristics (including hospital capacity), waiting times or patient-reported outcome quality indicators. Hence, the results of our study do not necessarily directly translate into an overall improved outcome quality for the patient.
Higher surgeon case load independently predicts a lower overall 2-year revision rate in patients undergoing primary total hip arthroplasty for hip osteoarthritis in Switzerland. Implementation of a minimum volume standard has the potential to reduce 2-year revision rates at the cost of a greater number of patients whose treatment needs to be reassigned.
No direct support for this project was received.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Siddiqi A, Alamanda VK, Barrington JW, Chen AF, De A, Huddleston JI 3rd, et al. Effects of Hospital and Surgeon Volume on Patient Outcomes After Total Joint Arthroplasty: Reported From the American Joint Replacement Registry. J Am Acad Orthop Surg. 2022 Jun;30(11):e811–21.
2. Featherall J, Brigati DP, Faour M, Messner W, Higuera CA. Implementation of a Total Hip Arthroplasty Care Pathway at a High-Volume Health System: Effect on Length of Stay, Discharge Disposition, and 90-Day Complications. J Arthroplasty. 2018 Jun;33(6):1675–80.
3. Schwartz AM, Farley KX, Guild GN, Bradbury TL Jr. Projections and Epidemiology of Revision Hip and Knee Arthroplasty in the United States to 2030. J Arthroplasty. 2020 Jun;35(6 6S):S79–85.
4. Nemes S, Gordon M, Rogmark C, Rolfson O. Projections of total hip replacement in Sweden from 2013 to 2030. Acta Orthop. 2014 Jun;85(3):238–43.
5. Michaëlsson K. Surgeon volume and early complications after primary total hip arthroplasty. BMJ. 2014 May;348(may23 1):g3433.
6. Ravi B, Jenkinson R, Austin PC, Croxford R, Wasserstein D, Escott B, et al. Relation between surgeon volume and risk of complications after total hip arthroplasty: propensity score matched cohort study. BMJ. 2014 May;348(may23 1):g3284.
7. Katz JN, Phillips CB, Baron JA, Fossel AH, Mahomed NN, Barrett J, et al. Association of hospital and surgeon volume of total hip replacement with functional status and satisfaction three years following surgery. Arthritis Rheum. 2003 Feb;48(2):560–8.
8. Scharfe J, Pfisterer-Heise S, Kugler CM, Shehu E, Wolf T, Mathes T, et al. The effect of minimum volume standards in hospitals (MIVOS) - protocol of a systematic review. Syst Rev. 2023 Jan;12(1):11.
9. Oakley CT, Arraut J, Lygrisse K, Schwarzkopf R, Slover JD, Rozell JC. The Effect of Surgeon and Hospital Volume on Total Hip Arthroplasty Patient-Reported Outcome Measures: An American Joint Replacement Registry Study. J Am Acad Orthop Surg. 2023 Feb;31(4):205–11.
10. Hoskins W, Rainbird S, Lorimer M, Graves SE, Bingham R. What Can We Learn From Surgeons Who Perform THA and TKA and Have the Lowest Revision Rates? A Study from the Australian Orthopaedic Association National Joint Replacement Registry. Clin Orthop Relat Res. 2022 Mar;480(3):464–81.
11. Sayers A, Steele F, Whitehouse MR, Price A, Ben-Shlomo Y, Blom AW. Association between surgical volume and failure of primary total hip replacement in England and Wales: findings from a prospective national joint replacement register. BMJ Open. 2020 Sep;10(9):e033045.
12. Glassou EN, Hansen TB, Mäkelä K, Havelin LI, Furnes O, Badawy M, et al. Association between hospital procedure volume and risk of revision after total hip arthroplasty: a population-based study within the Nordic Arthroplasty Register Association database. Osteoarthritis Cartilage. 2016 Mar;24(3):419–26.
13. Amato L, Fusco D, Acampora A, Bontempi K, Rosa AC, Colais P, et al. Volume and health outcomes: evidence from systematic reviews and from evaluation of Italian hospital data. Epidemiol Prev. 2017;41 5-6 (Suppl 2):1–128.
14. Manley M, Ong K, Lau E, Kurtz SM. Effect of volume on total hip arthroplasty revision rates in the United States Medicare population. J Bone Joint Surg Am. 2008 Nov;90(11):2446–51.
15. Vogel JF, Barkhausen M, Pross CM, Geissler A. Defining minimum volume thresholds to increase quality of care: a new patient-oriented approach using mixed integer programming. Eur J Health Econ. 2022 Sep;23(7):1085–104.
16. Beck M, Brand C, Christen B, Zdravkovic V. SIRIS report 2021 - Annual Report of the Swiss National Joint Registry, Hip and Knee 2022. Available from: https://www.swiss-medtech.ch/sites/default/files/2021-12/211130_SIRIS-Report%202021_online.pdf
17. Mufarrih SH, Ghani MO, Martins RS, Qureshi NQ, Mufarrih SA, Malik AT, et al. Effect of hospital volume on outcomes of total hip arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res. 2019 Dec;14(1):468.
18. Battaglia TC, Mulhall KJ, Brown TE, Saleh KJ. Increased surgical volume is associated with lower THA dislocation rates. Clin. Orthop. Relat. Res. Volume 447. Lippincott Williams and Wilkins; 2006. pp. 28–33.
19. Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, et al. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011 Feb;469(2):319–29.
20. Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stöckl B. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br. 2005 Jun;87(6):762–9.
21. Siebenmorgen JP, Stronach BM, Mears SC, Stambough JB. The Use of Intraoperative Digital Radiography Alignment Software to Assess Implant Placement in Total Hip Arthroplasty. Curr Rev Musculoskelet Med. 2021 Dec;14(6):369–77.
22. Wiegers EJ, Sewalt CA, Venema E, Schep NW, Verhaar JA, Lingsma HF, et al. The volume-outcome relationship for hip fractures: a systematic review and meta-analysis of 2,023,469 patients. Acta Orthop. 2019 Feb;90(1):26–32.
23. Katz JN, Wright EA, Wright J, Malchau H, Mahomed NN, Stedman M, et al. Twelve-year risk of revision after primary total hip replacement in the U.S. Medicare population. J Bone Joint Surg Am. 2012 Oct;94(20):1825–32.