Figure 1Workflow of General Consent (GC) patient data demography.
DOI: https://doi.org/https://doi.org/10.57187/s.3685
The clinical operations of hospitals generate substantial volumes of (medical) data on a daily basis. Current technical conditions make it possible to access those data for further use in human research. The secondary use of clinical data has the potential to transform medical research, expedite scientific breakthroughs, and enhance patient outcomes. However, there are drawbacks to such research, such as inadequate informed consent procedures.
In Switzerland, General Consent facilitates the secondary use of health-related data and biological samples in research projects that have not been specified [1–3]. However, the topic of General Consent is intricate and influenced by multiple variables. The challenges with General Consent are mainly of an ethical and legal nature, including the complexity and sophistication of the General Consent form [2, 4].
At the University Hospital Zurich, comprehensive patient information encompasses disease details, diagnoses, therapies and (socio-)demographic factors such as age, sex and religion. This information is meticulously recorded in the KISIM – the clinical record system. Since the introduction of General Consent at the University Hospital Zurich in 2015, General Consent status (known/ unknown) and General Consent choice (yes/no) have been systematically documented and displayed in the KISIM. If a patient withdraws their General Consent, the change is registered accordingly.
Building upon an earlier study by Griessbach et al. [1], who explored demographic and clinical factors influencing General Consent choice in the University Hospital Zurich patient population, this follow-up study investigated potential socio-demographic and clinical factors influencing General Consent status and choice. The outcome of this analysis aims to raise awareness among medical staff and researchers and enable more tailored and informed patient communication. In addition, the study results may guide potential adjustments to the General Consent process at the University Hospital Zurich, ensuring better alignment with the diverse needs of patients.
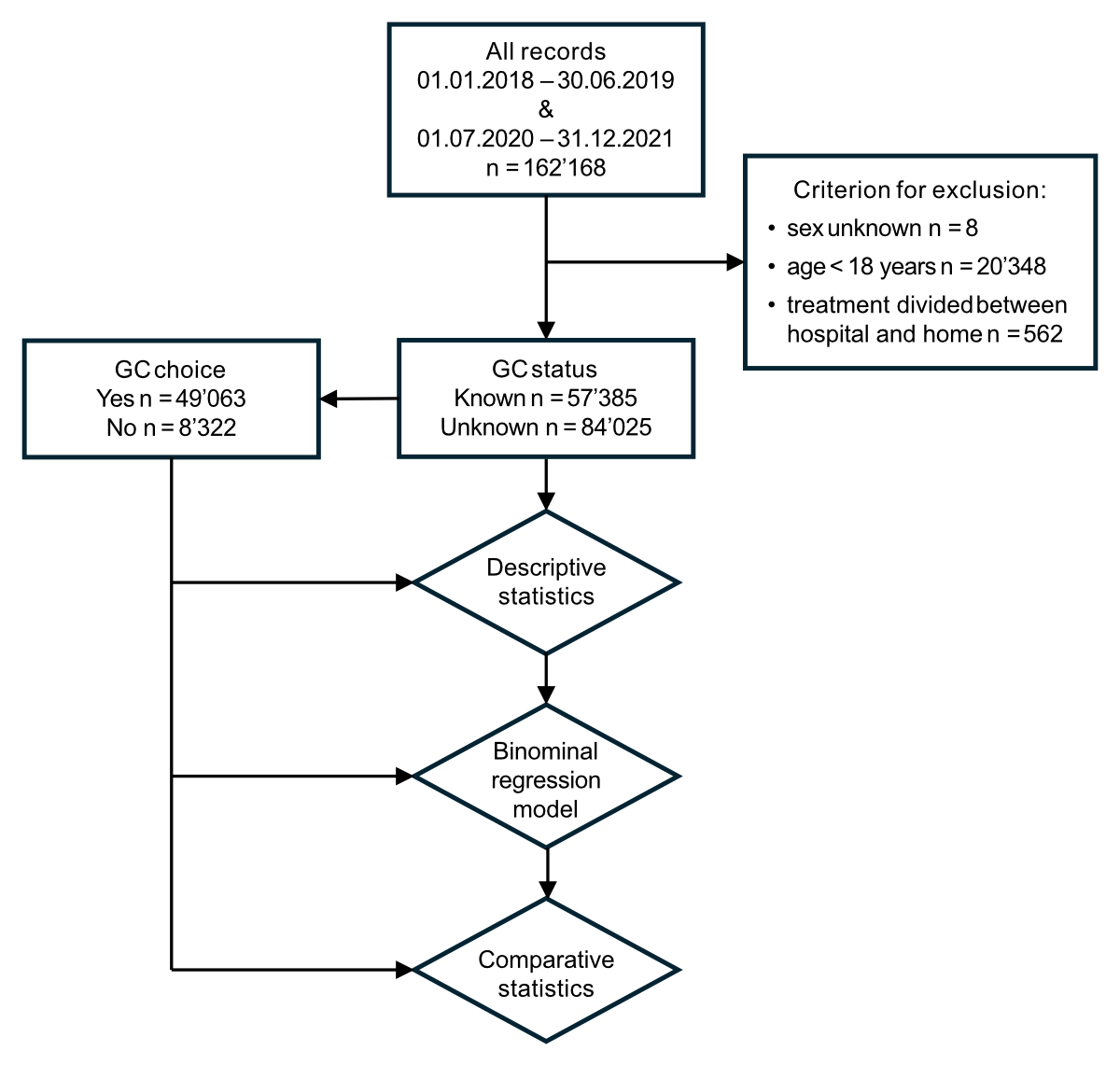
Two data sets comprising the records of all patients who had their first visit to the University Hospital Zurich (a patientʼs initial appointment or admission to the hospital)between January 1, 2018 and June 30, 2019 (before the COVID-19 pandemic), or between July 1, 2020 and December 31 2021 (during the COVID-19 pandemic) were included in the analysis (figure 1). The period of the first dataset was selected to align with the dataset used by Griessbach et al. [1] to ensure the comparability of the results.
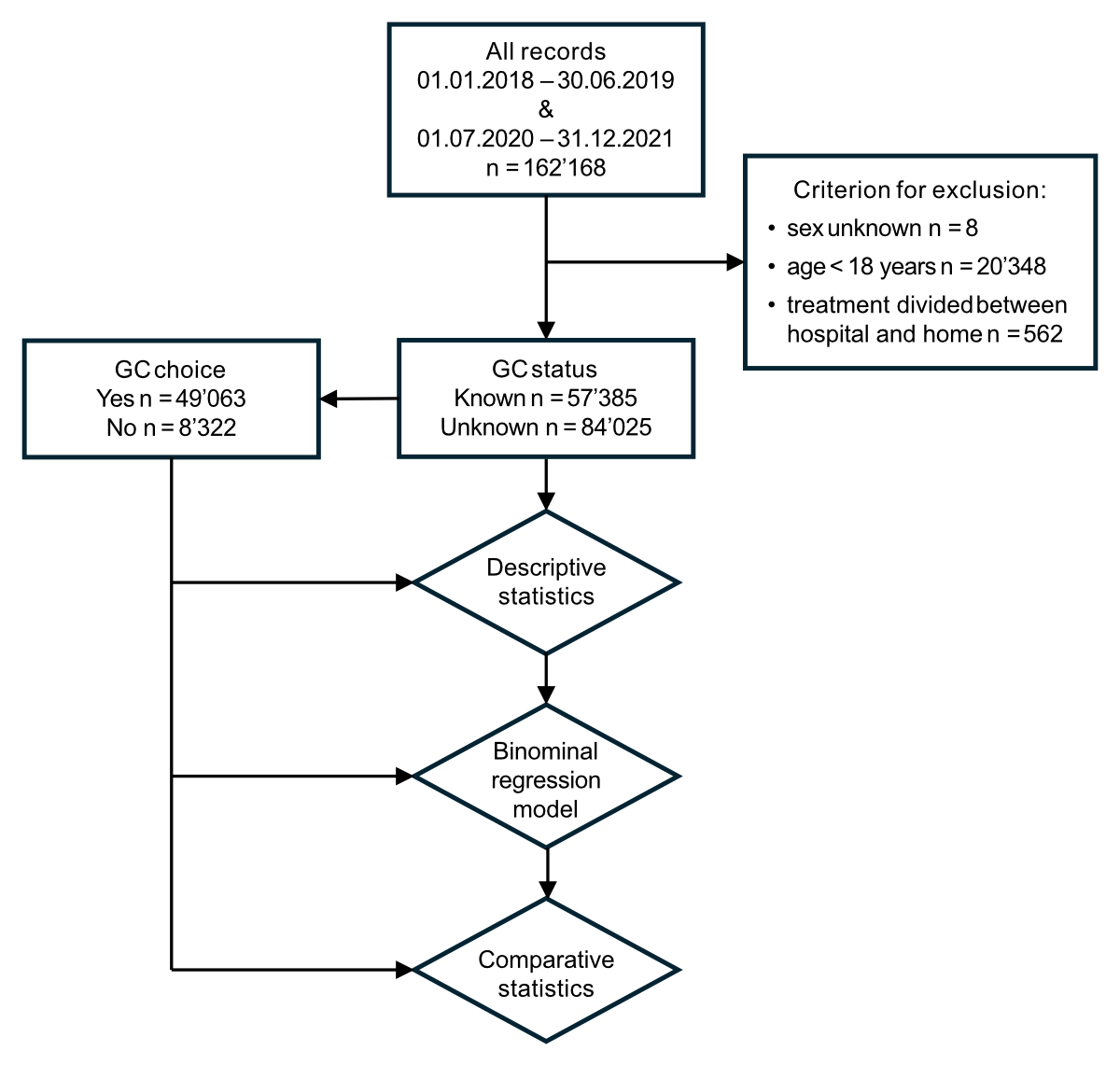
Figure 1Workflow of General Consent (GC) patient data demography.
The datasets were extracted from the KISIM in April 2022 and de-identified by the University Hospital Zurich IT Department. Database management and processing were conducted using structured query language statements to minimise the need for extensive data restructuring during statistical analyses.
Patients with missing values for sex, those under 18 years at their first visit or patients with an unclear declaration of the type of visit were excluded from the analysis via list-wise deletion. The two datasets were merged and descriptive and comparative statistics were used to describe associations between General Consent choice and socio-demographic and clinical factors (table 1).
Table 1Examined factors possibly influencing General Consent status and choice.
| Factor | Categories | Details |
| Sex | Female / male | NA |
| Age | Continuous | NA |
| Nationality | Swiss / not Swiss / not indicated | NA |
| Religion | Buddhism / hinduism / judaism / islam / atheism / not indicated | NA |
| Christianity | Christian catholic / roman catholic / protestant reformed | |
| Other | Free church / Jehovahʼs witnesses / orthodox churches / other religious commune | |
| Civil status | Single | Single / separated / divorced / widowed |
| Married or partnership / not indicated | NA | |
| Health insurance | General / semi-private / private | NA |
| Living will | Known / unknown | NA |
| Resuscitation preference | Known / unknown | NA |
| No. of ICD-10 diagnoses | Continuous | NA |
| Type of visit | In-patient / out-patient | NA |
| Visit during pandemic | Yes / no | NA |
ICD-10: International Statistical Classification of Diseases and Related Health Problems, Version 10.
Two multinomial and logistic regression models were used to investigate the potential associations between various socio-demographic and clinical factors and General Consent status (known/unknown) and General Consent choice (yes/no), respectively. In the first model, “General Consent status = unknown” served as the reference, while in the second model, the reference group was defined as “General Consent choice = no”. P-values of ≤0.001 were considered statistically significant. Associations were deemed clinically relevant if the odds ratios (ORs) were smaller than 0.50 or larger than 2.00. Volcano plots were generated to visually represent the results for General Consent status and choice. All statistical analyses were performed using R software (version 4.1.3, R Foundation for Statistical Computing, Vienna, Austria).
Only de-identified data was used, which conformed to local law and the ethical policies of the University Hospital Zurich [5]. The cantonal ethics committee confirmed that this research project did not fall under the scope of the Human Research Act (HRA) [5] and, therefore, did not require authorisation.
A total of 162,168 in- and out-patients having their first visit at the University Hospital Zurich were included in our analysis. Regarding General Consent status, significant differences (p <0.001) were observed for all variables and most of the categories. However, there were some exceptions. For religion, the categories Buddhism, Hinduism, Judaism, and atheism (with Christianity as the reference category) did not exhibit significant differences. Similarly, within the health insurance class variable, the category semi-private (with general insurance as the reference category) did not exhibit a significant difference. Lastly, for the nationality variable, the category not Swiss (with Swiss as the reference category) did not show a significant difference. For the variables in-/out-patient, number of diagnoses, living will, religion, and the category “not indicated” within the “religion” variable, a relevant difference (OR ≤0.5 or ≥2.0) was found (table 2, figure 2).
Table 2Sociodemographic characteristics associated with a known/unknown General Consent status in the binomial logistic regression analysis.
| Characteristics | Level | Known | Unknown | Odds ratio | Confidence interval | p-value |
| n | 57,385 (40.58%) | 84,025 (59.42%) | ||||
| Sex (%) | Female (= reference) | 31,210 (54.4) | 41,395 (49.3) | |||
| Male | 26,175 (45.6) | 42,630 (50.7) | 1.12 | 1.07; 1.17 | <0.001 | |
| Age, median (IQR) | 41.00 (30.00, 58.00) | 35.00 (27.00, 51.00) | 1.00 | 1.00; 1.00 | <0.001 | |
| Nationality (%) | Swiss (= reference) | 35,977 (62.7) | 55,130 (65.6) | |||
| Other | 16,112 (28.1) | 23,867 (28.4) | 1 | 0.96; 1.05 | 0.76297 | |
| Not indicated | 5296 (9.2) | 5028 (6.0) | 0.84 | 0.78; 0.90 | <0.001 | |
| Religion (%) | Christianity (= reference) | 19,419 (33.8) | 12,846 (15.3) | |||
| Buddhism | 168 (0.3) | 161 (0.2) | 1.19 | 0.81; 1.77 | 0.13525 | |
| Hinduism | 306 (0.5) | 302 (0.4) | 1.32 | 0.99: 1.76 | 0.00167 | |
| Islam | 2607 (4.5) | 2412 (2.9) | 1.24 | 1.11; 1.38 | <0.001 | |
| Judaism | 80 (0.1) | 83 (0.1) | 1.4 | 0.80; 2.44 | 0.04844 | |
| Other | 3941 (6.9) | 5243 (6.2) | 1.5 | 1.38; 1.63 | <0.001 | |
| Atheism | 10,652 (18.6) | 7853 (9.3) | 0.98 | 0.92; 1.05 | 0.32696 | |
| Not indicated | 20,212 (35.2) | 55,125 (65.6) | 2.43* | 2.27; 2.59 | <0.001 | |
| Civil status (%) | Single (= reference) | 21,902 (38.2) | 27,085 (32.2) | |||
| Taken | 21,193 (36.9) | 17,341 (20.6) | 0.84 | 0.79; 0.88 | <0.001 | |
| Not indicated | 14,290 (24.9) | 39,599 (47.1) | 1.38 | 1.29; 1.48 | <0.001 | |
| Living will (%) | Known (= reference) | 967 (1.7) | 294 (0.3) | |||
| Unknown | 56,418 (98.3) | 83,731 (99.7) | 2.11* | 1.67; 2.68 | <0.001 | |
| Resuscitation preference (%) | Known (= reference) | 6288 (11.0) | 4343 (5.2) | |||
| Unknown | 51,097 (89.0) | 79,682 (94.8) | 1.74 | 1.51; 2.00 | <0.001 | |
| Insurance (%) | General (= reference) | 39,528 (68.9) | 69,024 (82.1) | |||
| Semi-private | 635 (1.1) | 488 (0.6) | 1.05 | 0.83; 1.31 | 0.51549 | |
| Private | 17,222 (30.0) | 14,513 (17.3) | 0.74 | 0.71; 0.78 | <0.001 | |
| No. of diagnoses (%) | <2 (= reference) | 50,444 (87.9) | 78,914 (93.9) | |||
| ≥2 | 6941 (12.1) | 5111 (6.1) | 0.45* | 0.39; 0.53 | <0.001 | |
| Type of visit (%) | In-patient (= reference) | 5999 (10.5) | 5100 (6.1) | |||
| Out-patient | 51,386 (89.5) | 78,925 (93.9) | 0.30* | 0.24; 0.36 | <0.001 | |
| No. of patients, median (IQR) | 4251.00 (2589.00, 11,052.00) | 13,126.00 (4779.00, 28,089.00) | 1.00 | 1.00; 1.00 | <0.001 | |
| Pandemic (%) | No (= reference) | 29,210 (50.9) | 29,618 (35.2) | |||
| Yes | 28,175 (49.1) | 54,407 (64.8) | 0.9 | 0.86; 0.94 | <0.001 |
* relevant
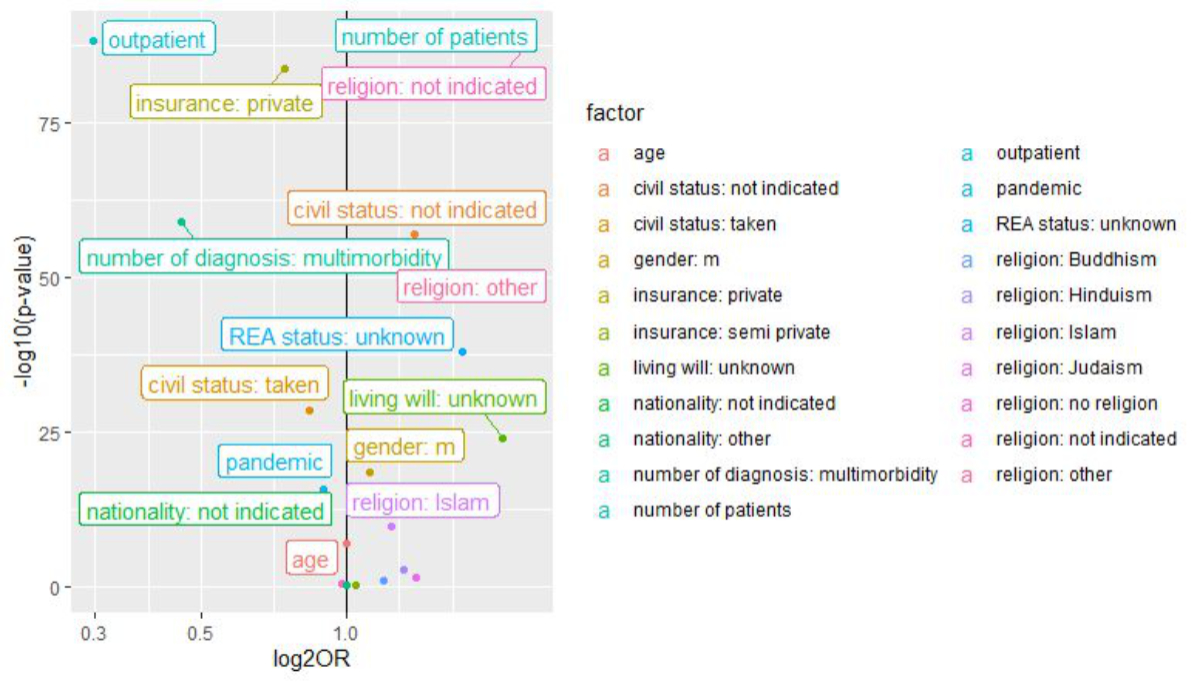
Figure 2Volcano plot: socio-demographic characteristics associated with a known/unknown General Consent status. OR: odds ratio; REA: reanimation.
Regarding General Consent choice, only patients with a known General Consent status (40.58% of all evaluated patients) were analysed. We found significant differences for age, sex, insurance, religion and nationality. However, only differences in the religion category were relevant (table 3, figure 3).
Table 3Socio-demographic characteristics associated with a yes/no response to the General Consent choice in the binomial logistic regression analysis.
| Characteristics | Level | Yes | No | Odds ratio | Confidence interval | p-value |
| n | 49,063 (85.50%) | 8322 (14.50) | ||||
| Sex (%) | Female (= reference) | 26,188 (53.4) | 5022 (60.3) | |||
| Male | 22,875 (46.6) | 3300 (39.7) | 0.78 | 0.72; 0.85 | <0.001 | |
| Age, median (IQR) | 42.00 (30.00, 59.00) | 38.00 (29.00, 54.00) | 1.00 | 0.99; 1.00 | <0.001 | |
| Nationality (%) | Swiss (= reference) | 31,246 (63.7 | 4731 (56.8) | |||
| Other | 13,405 (27.3) | 2707 (32.5) | 1.12 | 1.02; 1.23 | <0.001 | |
| Not indicated | 4412 (9.0) | 884 (10.6) | 1.25 | 1.09; 1.43 | <0.001 | |
| Religion (%) | Christianity (= reference) | 17,176 (35.0) | 2243 (27.0) | |||
| Buddhism | 139 (0.3) | 29 (0.3) | 1.38 | 0.66; 2.61 | 0.117 | |
| Hinduism | 243 (0.5) | 63 (0.8) | 1.68 | 1.02; 2.65 | <0.001 | |
| Islam | 1781 (3.6) | 826 (9.9) | 3.13* | 2.65; 3.69 | <0.001 | |
| Judaism | 70 (0.1) | 10 (0.1) | 1.04 | 0.28; 2.82 | 0.905 | |
| Other | 3231 (6.6) | 710 (8.5) | 1.57 | 1.34; 1.84 | <0.001 | |
| Atheism | 9231 (18.8) | 1421 (17.1) | 1.1 | 0.97; 1.24 | 0.011 | |
| Not indicated | 17,192 (35.0) | 3020 (36.3) | 1.33 | 1.17; 1.52 | <0.001 | |
| Civil status (%) | Single (= reference) | 18,797 (38.3) | 3105 (37.3) | |||
| Taken | 18,056 (36.8) | 3137 (37.7) | 1.03 | 0.93; 1.13 | 0.353 | |
| Not indicated | 12,210 (24.9) | 2080 (25.0) | 0.94 | 0.81; 1.08 | 0.132 | |
| Living will (%) | Known (= reference) | 875 (1.8) | 92 (1.1) | |||
| Unknown | 48,188 (98.2) | 8230 (98.9) | 1.17 | 0.82; 1.73 | 0.156 | |
| Resuscitation preference (%) | Known (= reference) | 5565 (11.3) | 723 (8.7) | |||
| Unknown | 43,498 (88.7) | 7599 (91.3) | 1.23 | 0.96; 1.59 | 0.008 | |
| Insurance (%) | General (= reference) | 33,484 (68.2) | 6044 (72.6) | |||
| Semi-private | 578 (1.2) | 57 (0.7) | 0.79 | 0.48; 1.26 | 0.116 | |
| Private | 15,001 (30.6) | 2221 (26.7) | 0.90 | 0.82; 0.99 | <0.001 | |
| No. of diagnoses (%) | <2 (= reference) | 42,976 (87.6) | 7468 (89.7) | |||
| ≥2 | 6087 (12.4) | 854 (10.3) | 0.98 | 0.75; 1.26 | 0.775 | |
| Type of visit (%) | In-patient (= reference) | 5280 (10.8) | 719 (8.6) | |||
| Out-patient | 43,783 (89.2) | 7603 (91.4) | 0.95 | 0.67; 1.34 | 0.606 | |
| No. of patients, median (IQR) | 4251.00 (2589.00, 11,052.00) | 4779.00 (2813.00, 11,052.00) | 1.00 | 1.00; 1.00 | 0.343 | |
| Pandemic (%) | No (= reference) | 24,990 (50.9) | 4220 (50.7) | |||
| Yes | 24,073 (49.1) | 4102 (49.3) | 1.03 | 0.95; 1.12 | 0.256 |
* relevant
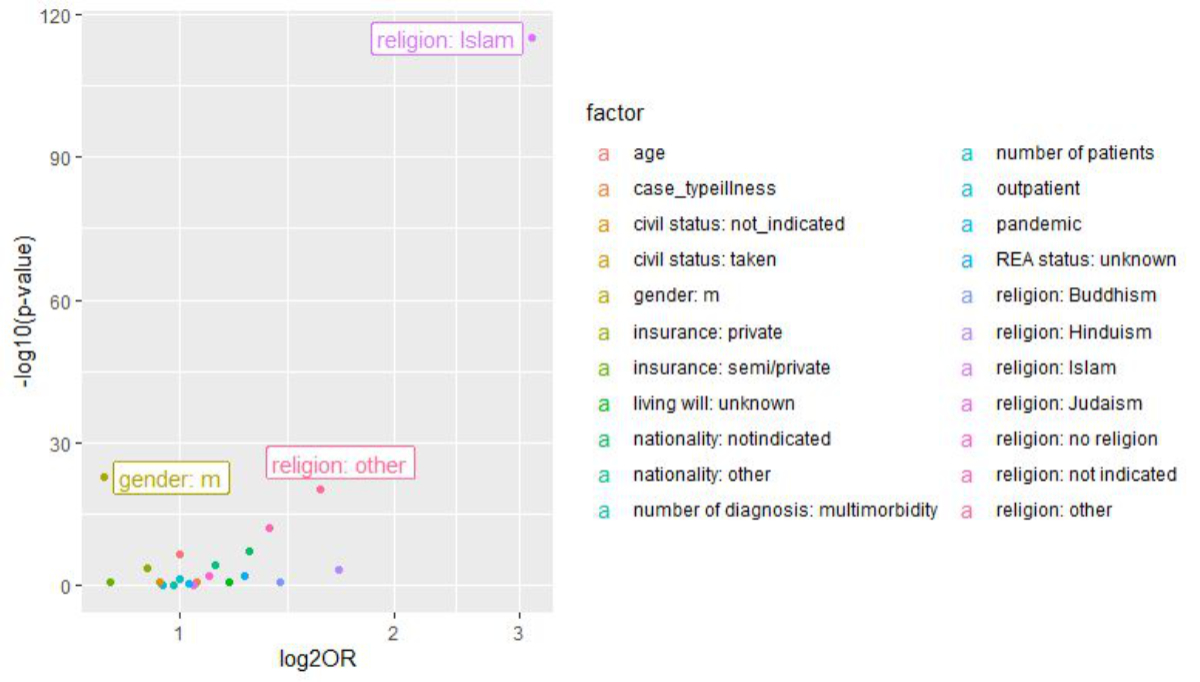
Figure 3Volcano plot: socio-demographic characteristics associated with the yes/no response to the General Consent choice. OR: odds ratio; REA: reanimation.
We observed a significant difference for sex, indicating that, compared with females, the General Consent status of males was more frequently unknown. However, this difference was not relevant (OR 1.12). Our model also indicated that female patients were more likely to decline General Consent than males, and, with increasing age, the odds of a positive General Consent choice increased. However, the strength of this association was not relevant (OR 1.28 and 0.99, respectively).
Our model predicted that if a patient’s nationality was not recorded in the KISIM, the odds of an unknown General Consent status and a negative General Consent choice would increase. Furthermore, not having a Swiss nationality was associated with declined General Consent. Nevertheless, these findings were not relevant.
If a patient’s religion was not recorded in the KISIM, the odds of having an unknown General Consent status were 2.5 times larger than in patients for whom Christianity was indicated as their religion (OR 2.54) (table 2). Furthermore, the model showed that patients who identified with Islam or a different religious denomination other than the five major world religions were more likely to have an “unknown” General Consent status. For both outcomes, we did not consider the OR (1.5) relevant.
In terms of General Consent choice, we identified significant differences between patients who indicated Christianity as their religion compared to those who identified with Hinduism, Islam, no religion, or a different religious denomination other than the five major world religions. The logistic regression model revealed that patients from these religious denominations were less likely to provide General Consent than patients identifying as Christian. However, only the difference between Christianity and Islam was relevant, indicating that patients stating their religion as Islam were three times more likely to decline General Consent than those who identified as Christian.
There were also significant differences for civil status, suggesting that patients with an unreported civil status were more likely to have an unknown General Consent status. We did not investigate any potential influence of civil status on General Consent choice.
If a patientʼs living will was unavailable, the odds of having an “unknown” General Consent status were twice as high as those with a documented living will. This difference was statistically significant and relevant (OR 2.1) (table 2). Additionally, when a patientʼs resuscitation preference was unknown, the odds of having an unknown General Consent status also increased, although not to a relevant degree (OR 1.74).
An OR of 0.74 was not considered a relevant difference in the General Consent status between patients with general and private health insurance. However, the model did show a statistically significant difference, indicating that the General Consent status of patients with private health insurance was more often known compared to those with general health insurance.
For patients with two or more ICD-10 diagnoses recorded at their first visit to the University Hospital Zurich, the odds of having an “unknown” General Consent status were half as likely as those with less than two diagnoses. This difference was statistically significant and relevant (OR 0.45) (table 2).
The odds of an unknown General Consent status differed depending on the type of visit. For in-patients, the odds were more than three times higher than for out-patients (table 2). This association was both statistically significant and relevant. Furthermore, the analysis revealed that patients who had their initial visit at the University Hospital Zurich during the COVID-19 pandemic were more likely to have an unknown General Consent status than those who had their first visit before the pandemic. However, there was no significant clinical difference in the odds of having an unknown General Consent status (OR 0.90).
This study found statistically significant differences for all variables considered in relation to General Consent status. However, relevant differences were only found for the following variables: type of visit, number of diagnoses, living will and religious status. This underlines the multi-faceted nature of factors influencing a patientʼs decision to consent and calls for a nuanced understanding of these aspects.
There was a non-relevant association between age, sex and General Consent status, as older males were more likely to have an unknown General Consent status. This age-related trend might be due to an increased susceptibility to cognitive changes that occur with advanced age [6]. This susceptibility could hinder their comprehension of the complex General Consent form, thereby lowering the completion rate.
For females and younger individuals, the likelihood of declining General Consent was high. A report from the Organisation of Economic and Cultural Development (OECD) has shown that women and younger individuals have low trust in their government and its institutions, which may contribute to a high rate of General Consent refusal among these groups [7].
These findings highlight the importance of enhancing transparency and trust in clinical research through customised education and easily comprehensible information material for various stakeholders. Plain summaries and patient-friendly communication can be effective tools to address challenges associated with understanding the content of the General Consent form and improving its transparency. On average (and across Europe), language proficiency levels fall between 2 and 3 [8, 9]. A proficiency level of 2 means being able to identify words and numbers in context and respond with basic information, such as filling out a form. A proficiency level of 3 entails the ability to identify, understand, synthesise, and respond to information and match information to a question. This level is roughly equivalent to completing high school. Based on research conducted across Europe, it is recommended that a plain- summary text target a literacy proficiency level of 2–3 [8, 9]. This target can be achieved by simplifying technical language and data (figures), as well as incorporating visual aids [8–11]. In fact, there are numerous available guidelines on how to write plain summaries [9–13].
Marital status was identified as influencing General Consent status (but was not relevant), suggesting there is an effect of social relationships on health-related decision-making, which underscores the interconnectedness of personal and social factors in the consent process.
Nationality and religion also emerged as significant factors. Patients who did not have a registered nationality or religion had significantly higher odds of having an unknown General Consent status compared to those with a registered Swiss nationality or those who identified as Christian. Various reasons may have contributed to nationality or religion not being recorded. A patient may not want to indicate their nationality and/or religion, or they were not asked for it, or the information may not have been documented in the KISIM– even when known. Incomplete documentation of socio-demographic and clinical details, often a result of time constraints or insufficient procedural protocols, can also lead to the absence of an enquiry about General Consent. According to our model, patients whose nationality was not registered in the KISIM or were not Swiss tended to decline General Consent more frequently. Previous studies have shown that ethnic minorities are under-represented in clinical research projects [14, 15] due to mistrust in medical research [16–18] and concerns about data abuse [19].
Religion emerged as a significant factor influencing General Consent choice. Specifically, we found a threefold likelihood of declining General Consent in patients identifying as Muslim compared to those identifying as Christian. Given that Muslims constitute a minority population in Switzerland with a migratory background [20], their reasons for declining General Consent may mirror observations made among other ethnic minorities: scepticism towards medical research, cultural differences or concerns about confidentiality [16, 21, 22]. However, there could be multi-faceted explanations for this finding; thus, it warrants further investigation.
These findings emphasise the importance of population-specific information that considers cultural and religious contexts to address patient concerns, improve participation and enhance engagement. To address these issues and better meet community needs, we recommend developing tailored informational materials using input from community representatives.
Patients with private health insurance exhibited a significantly higher response rate to General Consent and a positive General Consent choice than patients with general health insurance. Although the clinical relevance of the differences is unknown, the observed correlations suggest socio-demographic and clinical disparities could affect consent rates. In Switzerland, private health insurance is more expensive than the legally required general health insurance. Given the positive correlation between income and education levels [23], we presume that individuals with a lower educational level are more inclined to opt for general rather than private health insurance [23]. In the context of General Consent, individualsʼ awareness of being disadvantaged and compelled to choose general insurance may diminish their trust in the healthcare system, including clinical research, leading them to intentionally omit information or disregard the General Consent form. Similarly, several studies from the United States have indicated that a higher household income level and level of education positively correlate with trust in biomedical research and participation in clinical research [14, 23, 24].
When the General Consent was introduced at the University Hospital Zurich in 2015, General Consent collection was supposed to become a standard element of the admissions process for in- and out-patients in every clinic. However, our analysis showed a lower General Consent coverage rate among first-time patients and in-patients compared to the overall patient population at the University Hospital Zurich [25]. Furthermore, the probability of patients with two or more diagnoses having an unknown General Consent status was significantly lower than patients with fewer diagnoses. This result reflects the findings of the previous study by Griessbach et al. [1].
Documentation of resuscitation preferences and the presence of a living will significantly increased the odds of having a known General Consent status, though only the latter was deemed relevant. A living will often reflects a patientʼs engagement in medical decision-making, and its absence may indicate limited information about their preferences, including their stance on General Consent. We hypothesise that individuals with more diagnoses are likely to have greater health awareness, prompting them to make key health-related decisions, such as creating a living will and considering General Consent. Additionally, frequent hospital visits and closer patient interactions (associated with multiple diagnoses) may improve the chances of obtaining a response to General Consent over time.
This disparity raises questions about the equitable distribution of General Consent forms during initial visits and emphasises the need for a more standardised approach that ensures all patients have an equal opportunity to provide or decline consent. Therefore, it is crucial to continuously evaluate and adapt the relevant processes by applying plan-do-check-act (PDCA) cycles and raise awareness among medical staff on the importance of General Consent. For the latter, providing informational material explaining the concept and importance of General Consent could prove beneficial. It would also be advantageous to develop national recommendations on institutional General Consent processes to facilitate and harmonise inter-institutional collaborations.
Interestingly, the odds of having an unknown General Consent status decreased when patients had their first University Hospital Zurich visit during the COVID-19 pandemic. Although the decrease was statistically significant, it was not relevant. Nevertheless, the observed difference could be explained by the sensitisation of patients and hospital staff concerning the necessity of research during the pandemic.
For the variables living will, resuscitation preference, civil status, religion and health insurance class, only the status at the moment of data extraction could be analysed, not the status at the first visit. This also applied to General Consent status and choice. However, we assumed that these variables remained relatively constant and do not change regularly.
The incomplete reporting of non-mandatory variables in the KISIM could have introduced bias and obscured true differences between variable categories. This bias may have been further exacerbated by documentation bias, where patients with private health insurance or more frequent hospital visits may have received more meticulous documentation, potentially leading to incorrect conclusions. It was expected that in-patients would have more exhaustive documentation due to their longer hospital stays, but their coverage rate was lower than that of out-patients. Thus, to ensure the validity of the correlations, it is crucial to maintain high data integrity [7]. Therefore, we recommend raising awareness among medical personnel responsible for collecting socio-demographic information to report them in the KISIM, thereby enhancing data integrity for future studies. Finally, it should be noted that this study was based on data from the University Hospital Zurich and may not be generalisable to other populations.
In this study, we showed that University Hospital Zurich in-patients were more likely to have an unknown General Consent status than out-patients. To counteract this, which has also been observed in yearly General Consent numbers [25], we suggest re-evaluating the administrative General Consent process, including documentation practices. We also found that patients engaging with their medical decisions and those with multiple morbidities were more likely to have a known General Consent status. This could be attributed to a greater concern about oneʼs health and medical future and a more extensive interaction with healthcare professionals, which increases the likelihood of discussing and exploring the topic of General Consent. Improving the understanding of General Consent among patients and treating physicians has the potential to increase General Consent coverage rates at the University Hospital Zurich and promote genuine informed consent or dissent among patients at the University Hospital Zurich and beyond. To gain deeper insights into the potential cultural differences influencing General Consent choice, further investigations among specific populations are needed.
In conclusion, we need optimised and harmonised administrative procedures, targeted educational strategies and population-specific information materials to enhance the comprehensibility of the General Consent process. The goal is to promote more informed and engaged participation in medical research by acknowledging the complex interplay of socio-demographic and clinical factors within the healthcare context.
The datasets generated and/or analysed during this study are not publicly available due to the protection of patient data but are available from the corresponding author on reasonable request.
We would like to extend our appreciation to the University Hospital Zurich ICT for extracting the requested data and we thank the Clinical Trials Centre (CTC) Data Research Service Team for providing support in defining the de-identification criteria. Furthermore, we thank the EBPI and Stephan Benke for statistical consulting.
We express our gratitude to Lara Bernasconi and Michelle Sonderer for their valuable input when reviewing the manuscript.
Author contributions: JR, AB and RG contributed to the development of the methods and the analysis. JR and AB performed the literature search. JR and AG performed the data analysis and visualisation. JR and AB wrote the first draft of the manuscript. RG, AB and JR wrote sections of the manuscript. All authors contributed to manuscript revision and have read and approved the submitted version.
Neither the project nor the authors received any direct or indirect funding from public, commercial or non-profit organizations. The University Hospital Zurich has no financial interest in this work.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Griessbach A, Bauer A, Jörger Lebet F, Grossmann R. The concept of General Consent in Switzerland and the implementation at the University Hospital Zurich, a cross-sectional study. Swiss Med Wkly. 2022 Apr;152(1516):w30159.
2. Sprecher F, Talanova V. Verbesserungspotenzial des Generalkonsents. Schweiz Arzteztg. 2020 Sep;101(38):1197–200.
3. Salathé M, Driessen S. Generalkonsent: Eine einheitliche Vorlage soll schweizweite Forschung erleichtern. SAMW Bulletin; 2016. p. 3.
4. De Nardi G, Ehrensberger-Dow M, Matic I, Steiner F. Verständlichkeitsstudie Generalkonsent: Aufklärung und Einwilligung zur Weiterverwendung von biologischem Material und gesundheitsbezogenen Personendaten für die Forschung. Zürcher Hochschule für Angewandte Wissenschaften, Departement Angewantde Linguistik, Winterthur, 2018. Available from: https://digitalcollection.zhaw.ch/server/api/core/bitstreams/56e75bc2-1819-4d15-a0a8-1eacbf92379c/content
5. Swiss Federal Council. Federal Act on Research involving Human Beings (Human Research Act, HRA). (Status as of 26 May 2021). 2014. Available from: https://www.fedlex.admin.ch/eli/cc/2013/617/en
6. Ivashkov Y, Van Norman GA. Informed consent and the ethical management of the older patient. Anesthesiol Clin. 2009 Sep;27(3):569-80, table of contents. doi: .
7. Building Trust to Reinforce Democracy. Main Findings from the 2021 OECD Survey on Drivers of Trust in Public Institutions. Building Trust in Public Institutions: OECD; 2022. doi: . Available from: https://www.oecd.org/en/publications/building-trust-to-reinforce-democracy_b407f99c-en.html
8. OECD skills outlook 2013: first results from the survey of adult skills. Paris: OECD Skills Outlook; 2013. Available from: https://www.oecd.org/en/publications/oecd-skills-outlook-2013_9789264204256-en.html
9. European Commission. Summaries of Clinical Trial Results for Laypersons - Recommendations of the expert group on clinical trials for the implementation of Regulation (EU) No 536/2014 on clinical trials on medicinal products for human use. 26. Januar 2017. Available from: https://health.ec.europa.eu/system/files/2020-02/2017_01_26_summaries_of_ct_results_for_laypersons_0.pdf
10. Clinical Trials Expert Group. Good Lay Summary Practice. European Commission, 9. Juli 2021.
11. Duke M. How to Write a Lay Summary. Digital Curation Centre (DCC), 2012. Available from: http://www.dcc.ac.uk/resources/how-guides.
12. Barnes A, Patrick S. Lay Summaries of Clinical Study Results: an Overview. Pharmaceut Med. 2019 Aug;33(4):261–8.
13. National Institute for Health Research (NIHR). Plain English summaries. April 2021. Available from: https://www.nihr.ac.uk/documents/plain-english-summaries/27363
14. Cunningham-Erves J, Villalta-Gil V, Wallston KA, Boyer AP, Wilkins CH. Racial differences in two measures of trust in biomedical research. J Clin Transl Sci. 2019 Jun;3(2-3):113–9.
15. Sateren WB, Trimble EL, Abrams J, Brawley O, Breen N, Ford L, et al. How sociodemographics, presence of oncology specialists, and hospital cancer programs affect accrual to cancer treatment trials. J Clin Oncol. 2002 Apr;20(8):2109–17.
16. Corbie-Smith G, Thomas SB, St George DM. Distrust, race, and research. Arch Intern Med. 2002 Nov;162(21):2458–63.
17. Brandon DT, Isaac LA, LaVeist TA. The legacy of Tuskegee and trust in medical care: is Tuskegee responsible for race differences in mistrust of medical care? J Natl Med Assoc. 2005 Jul;97(7):951–6.
18. Archibong B, Annan F. We Are Not Guinea Pigs: The Effects of Negative News on Vaccine Compliance. Global Economy and Development at Brookings; Jan 2021;10. Available from: https://www.brookings.edu/wp-content/uploads/2021/12/We-are-not-guinea-pigs_final.pdf
19. Thompson HS, Valdimarsdottir HB, Jandorf L, Redd W. Perceived disadvantages and concerns about abuses of genetic testing for cancer risk: differences across African American, Latina and Caucasian women. Patient Educ Couns. 2003 Nov;51(3):217–27. doi: https://doi.org/10.1016/S0738-3991(02)00219-7
20. Bundesamt für Statistik. Entwicklung der Religionslandschaft. Ständige Wohnbevölkerung ab 15 Jahren. Available from: https://www.bfs.admin.ch/asset/de/23925660
21. Levkoff S, Sanchez H. Lessons learned about minority recruitment and retention from the Centers on Minority Aging and Health Promotion. Gerontologist. 2003 Feb;43(1):18–26.
22. Corbie-Smith G, Thomas SB, Williams MV, Moody-Ayers S. Attitudes and beliefs of African Americans toward participation in medical research. J Gen Intern Med. 1999 Sep;14(9):537–46.
23. Tamborini CR, Kim C, Sakamoto A. Education and Lifetime Earnings in the United States. Demography. 2015 Aug;52(4):1383–407.
24. Unger JM, Hershman DL, Albain KS, Moinpour CM, Petersen JA, Burg K, et al. Patient income level and cancer clinical trial participation. J Clin Oncol. 2013 Feb;31(5):536–42.
25. Zettler S, Jörger F. General Consent inpatient and outpatient Numbers from 2017 to. University Hospital Zurich, University Hospital Zurich-internal Document; 2022.