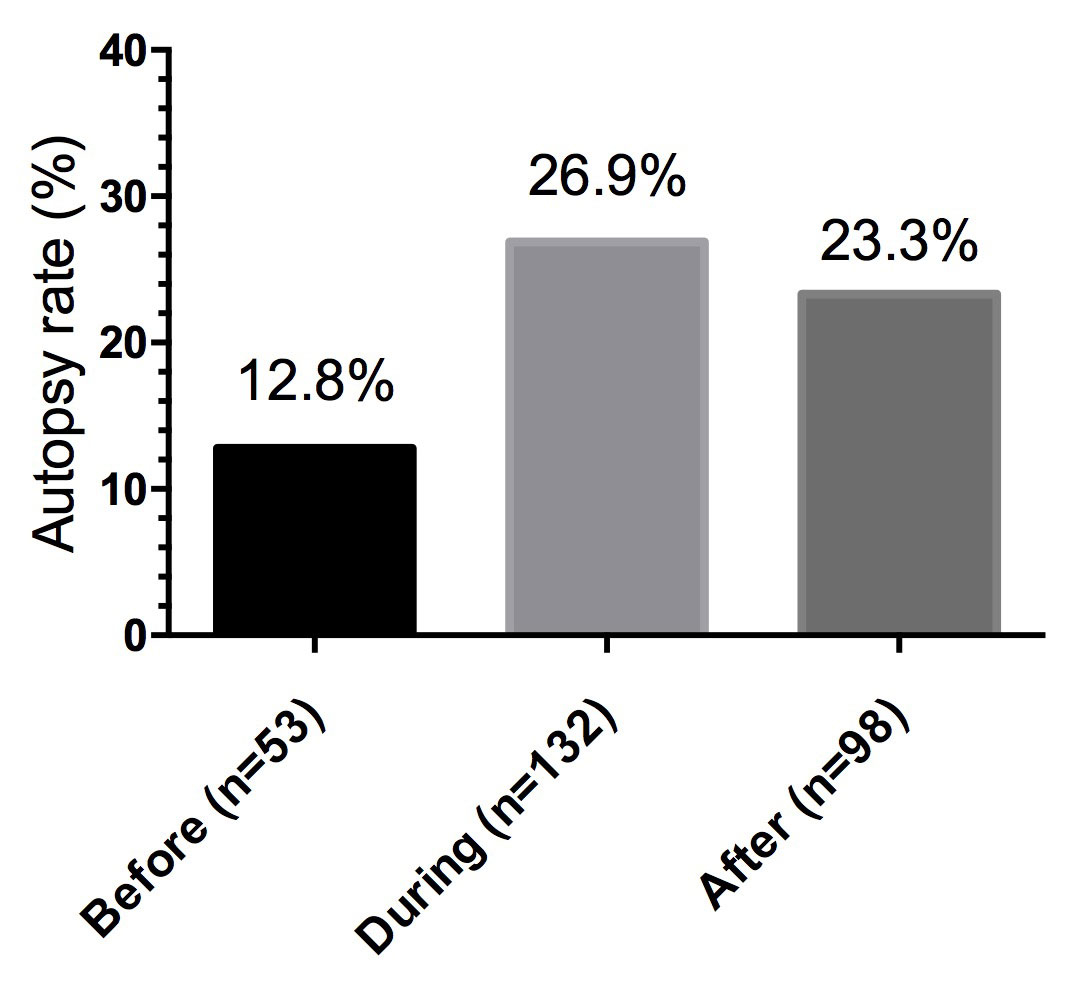
Figure 1 Autopsy rates in 12-month intervals before, during and after the intervention.
DOI: https://doi.org/10.4414/smw.2018.14679
Autopsy (necropsy, post-mortem examination) is an important source of medical knowledge. The main functions of autopsies are: (1) determination of the cause and manner of death and the underlying medical conditions, (2) feedback to clinicians for quality control, (3) teaching tool for medical students and pathologists in training, (4) biomedical research tool, (5) source for tissue banking, (6) source of epidemiological data, (7) source of data for forensic and legal matters, and (8) source of documentation for insurance and workers’ compensation claims.
In Western Europe, the USA and other parts of the world, autopsy rates have declined markedly [1–4]. In the USA, the autopsy rate has dropped from approximately 60% in 1950 to less than 5% over the last decade [5, 6]. In Germany, autopsy rates have decreased by 30% between and 2005 and 2014 [7].
There are several causes for decreasing autopsy rates such as: legal obligations to obtain autopsy consent (usually from relatives), objections to and insufficient knowledge of autopsies among the general public, relatives viewing autopsy as unnecessary, religious beliefs, the cost of autopsies, insufficient reimbursement of pathologists, clinicians’ lack of interest in autopsies, additional workload to clinicians and pathologists’ fear of malpractice litigation [8–12].
Decreasing autopsy rates have serious implications. Numerous studies have demonstrated marked discrepancies between clinical diagnoses and findings at autopsies [13–18]. These data show that autopsies are an essential tool for quality control. Hence, a further decline in autopsy rates is likely to result in a decreased quality of medical care.
The decision of doctors, patients and relatives for or against an autopsy is based on subjectively balancing the potential benefits and disadvantages of an autopsy. Thus, it is likely that an intervention that can resolve this conflict will be more effective in obtaining consent to an autopsy than unstructured counselling. In 1991, Miller and Rollnick introduced a method of counselling clients with substance abuse [19]. The goal of this client-centred and direct approach is changing behaviour by resolving ambivalence in a non-confrontational atmosphere. The counsellor attempts to point out the disadvantages of the client’s present behaviour or values by respectful and non-judgmental counselling in order to create motivation towards change [19]. Numerous empirical studies have documented the efficacy of behavioural interviewing [20, 21].
Motivational interviewing is characterised by four principles: empathy, disclosure of ambivalence, gentle handling of resistance and the promotion of self-confidence in the client’s ability to change their mind. Therapeutic techniques to establish these principles are open questions, affirmation, acknowledgement of the client’s statements and summarising results. Counselling consists of two stages. First, the interviewer exposes the pros and cons of a behavioural pattern or value by guiding the client towards self-reflection on his or her behaviour or values to resolve ambivalence. The second stage consists of drafting binding goals and actions towards change [21, 22].
The request for autopsy permission may create conflicts between two perceptions of autopsy. On the one hand, patients or relatives may conceive autopsy as degrading, mutilating, time-consuming, unnecessary, immoral, expensive, or incompatible with one’s own or the decedent’s religious/moral beliefs and values. On the other hand, patients or relatives may view post-mortem examination as one of the decedent’s last services to society and medical knowledge, altruistically benefiting others [23].
Experts can teach motivational interviewing efficiently and effectively to physicians of all medical specialties in a single, short training session [24]. For this study, the technique of motivational interviewing was adapted to interviews with relatives aimed at obtaining autopsy consent.
Our goals were to identify the attitudes of multimorbid patients and their family members towards autopsies and to determine whether the autopsy rate could be improved by motivational interviewing according to Miller and Rollnick.
The study was performed in accordance with the Declaration of Helsinki.
This prospective, nonrandomised intervention study consisted of two parts:
Tutorials were held on 4 November 2014 (multiple tutorials), 11 November 2014, 18 December 2014 and 29 June 2015 (multiple tutorials). All residents and consulting clinicians of the Department of Medicine participated in at least one tutorial. Few physicians attended two tutorials. The tutorials lasted 1 hour and each was attended by 10 to 11 clinicians.
The goal of the tutorials was to enable physicians to communicate effectively and confidently with grieving relatives in requesting autopsy permission. Tutorials focused on how to point out the importance and benefits of an autopsy in an empathic way based on the following guidelines:
The tutorials emphasised the following reasons to convince grieving relatives to consent to an autopsy:
The participants were also made aware of the following reasons that may cause relatives to reject an autopsy:
From November 2014 to October 2015, motivational interviewing was employed in requesting autopsy permission from a first-degree relative (spouse or child). The goal was to overcome ambivalence towards autopsy by empathy and education about the purpose and conduct of an autopsy to obtain consent.
Interventional interviewing was performed only when relatives expressed ambivalence about permitting an autopsy. If the deceased had conveyed a positive or negative decision towards his or her own autopsy either verbally or in writing, this decision was not questioned. Similarly, no attempt was made to change a decision if the relatives had already decided before talking to the clinician. We did not inquire as to the reasons for finally declining autopsy permission once that decision had been made. No attempts were made to obtain autopsy permission from either the patient or his or her relatives prior to the patient’s death.
All interviews were performed by either the house officer (intern or resident) or the senior physician (attending) assigned to the patient’s ward. If a patient died on a weekend, relatives were asked to come to the interview the following Monday or the interview was performed over the telephone. If a patient died in the emergency room, the interview was carried out by the emergency room physician on duty, who had also been trained in motivational interviewing. A feedback questionnaire was to be completed by each physician after talking to the decedent’s relatives and asking for autopsy permission, in order to determine whether the motivational interviewing had been performed according to the study protocol.
Absolute and relative figures from the opinion poll were presented descriptively and without further statistical analysis. Fisher’s exact test was used to compare the autopsy rates before, during and after the intervention (November 2015 to October 2016). A p-value of <0.05 was considered statistically significant. Microsoft Excel® was used for data collection and statistical evaluations.
Of the 149 multimorbid patients and first-degree relatives who were asked to participate in the survey, 90.6% of the patients but only 55.0% of the relatives completed a questionnaire. On average, the patients were 10 years older than their first-degree relatives. There was a slight preponderance of women over men in both groups (table 1).
Table 1 Participation of multimorbid patients and first-degree relatives in survey.
| Patients | Relatives | |
|---|---|---|
| Asked to participate in survey (n) | 149 | 149 |
| Questionnaire completed (n) | 135 | 82 |
| Age (years, mean) | 65.8 | 55.9 |
| Men (n) | 63 | 34 |
| Women (n) | 72 | 48 |
As shown in table 2, the vast majority of patients and relatives believed that autopsies have a number of different functions.
Table 2 Reasons for performing autopsies as seen by multimorbid patients (n = 91) and their first-degree relatives (n = 55).
| What are reasons for performing autopsies? | Patients (%) | Relatives (%) |
|---|---|---|
| Determining the cause of death | ||
| Yes, definitely | 80 | 87 |
| No, most likely not | 11 | 4 |
| No, definitely not | 6 | 5 |
| No answer | 3 | 4 |
| Detection of treatment errors | ||
| Yes, definitely | 70 | 67 |
| No, most likely not | 13 | 18 |
| No, definitely not | 8 | 9 |
| No answer | 9 | 6 |
| Improvement of future therapies | ||
| Yes, definitely | 89 | 91 |
| No, most likely not | 8 | 5 |
| No, definitely not | 1 | 7 |
| No answer | 2 | 6 |
| Education of medical trainees | ||
| Yes, definitely | 79 | 82 |
| No, most likely not | 12 | 5 |
| No, definitely not | 4 | 7 |
| No answer | 5 | 6 |
| Detection of hereditary diseases | ||
| Yes, definitely | 66 | 56 |
| No, most likely not | 25 | 36 |
| No, definitely not | 3 | 2 |
| No answer | 6 | 6 |
Objections to autopsies were similar in patients and relatives (table 3). They were mostly based on the view that autopsies compromise the integrity of the decedent’s body or represent unnecessary experimentation. Furthermore, it was widely believed that pertinent diagnoses are already known before death. Religions objections were mentioned only in a small minority of patients and relatives.
Table 3 Reasons against performing autopsies as seen by multimorbid patients (n = 91) and their first-degree relatives (n = 55).
| What are reasons against performing autopsies? | Patients (%) | Relatives (%) |
|---|---|---|
| Compromising the integrity of the body | ||
| Yes, definitely | 34 | 25 |
| No, most likely not | 35 | 22 |
| No, definitely not | 14 | 42 |
| No answer | 8 | 11 |
| Unnecessary experimentation | ||
| Yes, definitely | 26 | 29 |
| No, most likely not | 35 | 31 |
| No, definitely not | 22 | 29 |
| No answer | 8 | 11 |
| Unnecessary cost | ||
| Yes, definitely | 6 | 5 |
| No, most likely not | 44 | 47 |
| No, definitely not | 35 | 36 |
| No answer | 6 | 12 |
| Religious objections | ||
| Yes, definitely | 10 | 4 |
| No, most likely not | 20 | 18 |
| No, definitely not | 54 | 65 |
| No answer | 7 | 13 |
| Diagnosis is already known before death | ||
| Yes, definitely | 24 | 31 |
| No, most likely not | 44 | 35 |
| No, definitely not | 15 | 27 |
| No answer | 8 | 7 |
Because the questionnaire was modified during the study, the results to both questionnaires are listed separately. As shown in table 4 and table 5, between 51% and 75% of the patients and approximately 75% of the relatives responded that they would grant permission to their own autopsy. As shown in table 6 and table 7, the majority of patients and relatives stated that they would agree to the autopsy of a relative.
Table 4 Consent to own autopsy (questionnaire 1).
| Would you consent to your own autopsy? | Patients (%) | Relatives (%) |
|---|---|---|
| Yes | 75 | 74 |
| No | 25 | 22 |
| No answer | 0 | 4 |
Table 5 Consent to own autopsy (questionnaire 2).
| Would you consent to your own autopsy? | Patients (%) | Relatives (%) |
|---|---|---|
| Yes, definitely | 51 | 75 |
| No, probably not | 31 | 25 |
| No, definitely not | 18 | 0 |
Table 6 Consent to the autopsy of a relative (questionnaire 1).
| Would you consent to the autopsy of a relative? | Patients (%) | Relatives (%) |
|---|---|---|
| Yes | 75 | 63 |
| No | 25 | 33 |
| No answer | 0 | 4 |
Table 7 Consent to the autopsy of a relative (questionnaire 2).
| Would you consent to the autopsy of a relative? | Patients (%) | Relatives (%) |
|---|---|---|
| Yes, definitely | 52 | 62 |
| No, probably not | 26 | 33 |
| No, definitely not | 22 | 3 |
| No answer | 0 | 2 |
During the intervention, 489 patients died in the Department of Medicine. In 353 cases (72.2%), a questionnaire was returned by the interviewing physician after the interview documenting that motivational interviewing had been performed according to protocol. No questionnaire was returned in 136 cases (27.8%). In these cases, it is uncertain whether motivational interviewing had been performed. It is also not known whether a decision to refuse or grant autopsy permission had been reached prior to talking to the physician. There was no overlap between the interviewees in the opinion poll and the relatives asked for autopsy permission.
From 2010 to 2017, a total of 3,499 patients died in the Department of Medicine of the Kantonsspital Winterthur. In 625 of these cases (17.9%), an autopsy was performed. The numbers for each year are shown in table 8.
Table 8 Autopsy rates from 2010 to 2017.
| Year | Deaths (n) | Autopsies (n) | Autopsy rate (%) |
|---|---|---|---|
| 2010 | 412 | 78 | 18.9 |
| 2011 | 403 | 70 | 17.4 |
| 2012 | 406 | 49 | 12.1 |
| 2013 | 435 | 54 | 12.4 |
| 2014* | 436 | 72 | 16.5 |
| 2015* | 493 | 117 | 23.7 |
| 2016 | 440 | 96 | 21.8 |
| 2017 | 474 | 89 | 18.8 |
* Motivational interviewing was performed from November 2014 to October 2015.
In accordance with institutions worldwide, there was a decline in the autopsy rate from 2010 to 2013. During the intervention, the autopsy rate almost doubled. After motivational interviewing was terminated, the autopsy rate dropped again. However, in 2017, more than one year after terminating formal motivational interviewing, it was still above that before the intervention.
The time interval during which motivational interviewing was performed (November 2014 to October 2015) includes parts of two calendar years. Therefore, the numbers for 12-month intervals before, during and after the intervention are shown in figure 1 and table 9.
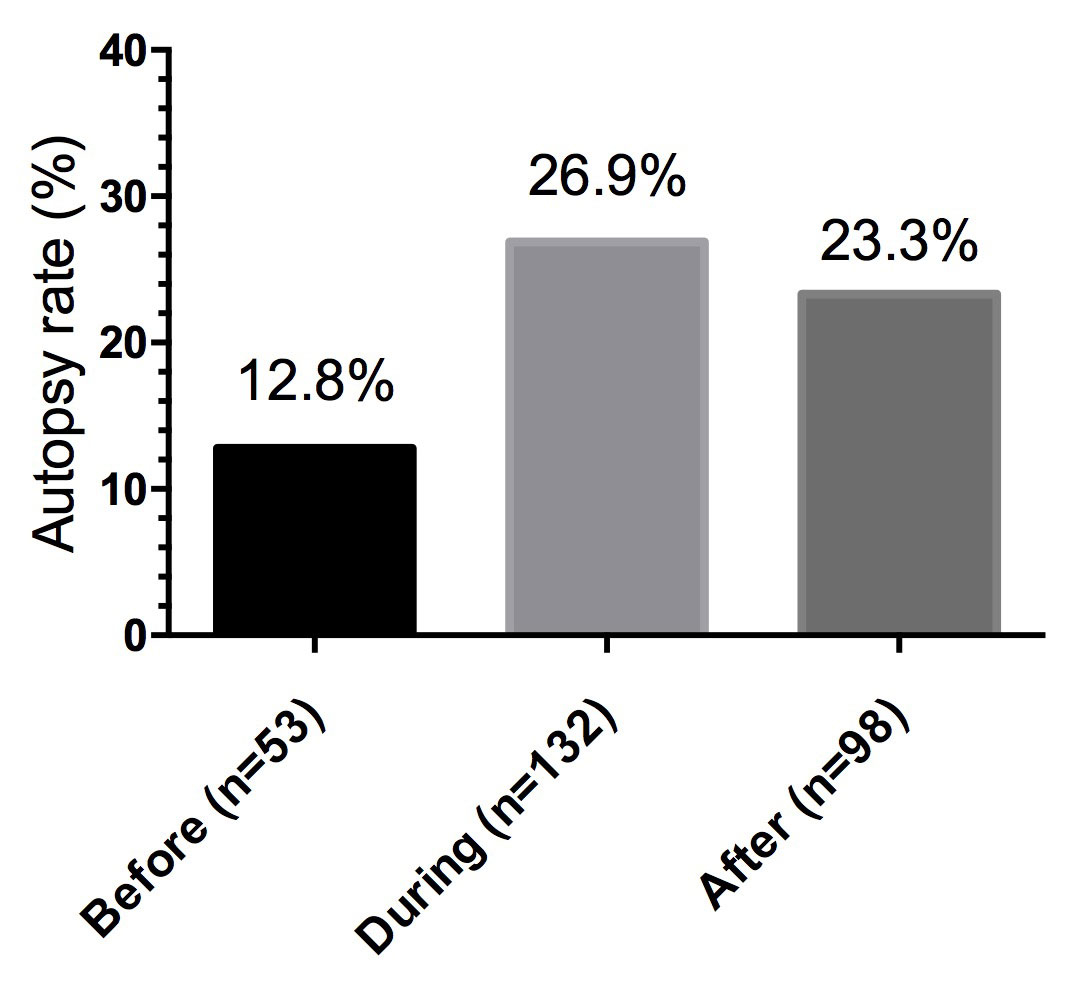
Figure 1 Autopsy rates in 12-month intervals before, during and after the intervention.
Table 9 Number of deaths and autopsies in 12-month intervals before, during and after the intervention. The difference was statistically highly significant (Fisher’s exact test: p <0.0001).
| Autopsy | Sum | ||
|---|---|---|---|
| Yes | No | ||
| Before intervention | 53 | 359 | 412 |
| During intervention | 132 | 357 | 489 |
| After intervention | 98 | 333 | 431 |
During the 12-month intervention, the autopsy rate increased from 12.8% to 26.9%. This represents a 110% increase. During the 12-month period after motivational interviewing had been terminated, there was a decrease in the number of autopsies from 26.9% to 23.3% of all patients who died in the Department of Medicine.
As determined by Fisher’s exact test, the difference between the autopsy rate before and during the intervention was highly statistically significant (p <0.0001). Similarly, the difference between the autopsy rate before and after the intervention was highly statistically significant (p <0.0002). In contrast, the decrease in the autopsy rate after the intervention was not statistically significant (p = 0.174).
In the present study, the vast majority of patients and relatives were aware of the importance of autopsies and stated that they would consent to their own autopsy or to the autopsy of a relative. These numbers are consistent with data from Germany: in 2010, a representative telephone poll was conducted by the German polling institute Forsa. In this poll, 1003 German citizens 18 years old or older were interviewed. Eighty-four percent supported the performance of autopsies, 72% stated that they would consent to their own autopsy and 65% indicated consent to the autopsy of a relative. Of those respondents who had been asked in the past about consenting to the autopsy of a relative, 66% had agreed to an autopsy. These data indicate that the low autopsy rates are only in part the result of objections among the general population. Structural reasons within the health care system, including a lack of motivation to increase the autopsy rate among clinicians and pathologists, appear to play a critical role [9, 25, 26].
The most important result of this study is the increase in the autopsy rate from 13% before the intervention to 27% when motivational interviewing was used in asking relatives for autopsy permission. Furthermore, there was only a small and statistically insignificant decline in the autopsy rate during the twelve months after formal motivational interviewing was terminated in order to determine the impact of this interviewing technique.
These data raise several questions. Was the increase in the autopsy rate truly due to motivational interviewing or was it completely or partially caused by something else? Most clinical studies answer the question of causation through randomised double-blind trials [27, 28]. This approach was not feasible in the present study, as there would have been marked cross contamination by the intervention. However, there is strong evidence in favour of a causative role of motivational interviewing. First, as shown in reference 8, there was a continuous decline in the autopsy rate in the years before this study. A pattern of alternating increases and decreases did not occur. Second, healthcare providers in this region similar to our own institution report a constant decline in autopsy rates (data not shown). Therefore, it is almost certain that the increased autopsy rate was due to an increase in the attention and commitment of physicians to the matter, and improved skills in communicating with grieving relatives to obtain autopsy permission. A cluster randomised trial to further corroborate this would be interesting. However, a cluster trial was not performed in the present study due to limited resources (in-house funding only). The fact that the autopsy rate remained relatively high in the twelve months after the formal technique of motivational interviewing was terminated is of great interest. It indicates that the communication skills and the motivation to obtain autopsy permission were not lost, but extended beyond the intervention period. This is a very encouraging observation.
Nevertheless, surveillance bias could have increased the autopsy rate even without motivational interviewing. Surveillance bias refers to the fact that participants in a study receive more attention than non-participants [29]. Whether motivational interviewing per se or other factors associated with the intervention increased the autopsy rate remains open. Others have also reported increased autopsy rates due to various measures. Gardner et al. have reported that autopsy rates could be increased if physicians were taught how to communicate with grieving relatives and ask for autopsy consent more effectively [30]. Souza et al. were able to increase the autopsy rate from 7.5% to 16.8% during a 6-month intervention consisting of three steps: (1) a 2-hour tutorial to residents on how to obtain autopsy permission; (2) if no permission was obtained by the resident, a second attempt was made by the chief resident; (3) if autopsy was finally denied, the resident who signed the death certificate had to complete a questionnaire asking why autopsy had not been permitted [31]. Rothe et al. reported that their autopsy rate was increased from 3.3% to 26% by a set of measures such as mandatory flow charts and standard operating procedures for the entire hospital. Furthermore, the hospital asked relatives to complete a questionnaire on autopsies. An attending physician talked with the relatives, probably the decisive intervention. Physicians participated in informal tutorials on how to talk to grieving families. Although motivational interviewing was not specifically used, the autopsy rate increased from 3.3% to 26%, a similar order of magnitude to the present study [23]. Champ et al. compared two neighbouring district hospitals with autopsy rates of 11% and 40-50% respectively. The two hospitals were comparable except for the handling of deaths, interaction with the decedents’ families and the organisation of the mortuary. At the hospital with the high autopsy rate, all death certificates were centralised within the mortuary and the family was contacted by the certifying physician in a bereavement room. Relatives, clinicians and pathologists were coordinated by autopsy technicians. Clinicopathological conferences were held regularly and clinicians had a positive attitude to autopsies [32].
The increase in the autopsy rate from 13% to 27% in the present study can be considered evidence of a successful intervention. The development of a standardised interviewing procedure based on this study’s findings and online tutorials on motivational interviewing may be able to stabilise the higher autopsy rate and contribute to improvements in the quality of medical care.
A significant number of patients and relatives declined to participate in the survey in the first place or did not complete their questionnaires. This may indicate a non-response bias. Non-response bias is a systematic error due to differences between responders and non-responders [29]. In the present study, participants of the survey may not fully represent the multimorbid patients in the hospital and their relatives. Non-participants may have had reservations towards autopsies and may have declined to be bothered with this issue, while individuals with a more positive view on the procedure may have completed the questionnaires. Participation in the survey was declined by only 14 of 149 patients (9.4%) but by 67 of 149 relatives (44.9%). These numbers indicate that a non-response bias may be of some significance. In particular, the mostly positive responses by relatives must be interpreted with great care. In the vast majority of cases, it is the relatives’ decision whether an autopsy will be performed. Thus, a non-response bias may in part explain the striking discrepancy between the mostly positive attitude towards autopsies in the survey and the low autopsy rate at this institution and in general. However, the magnitude of this bias cannot be determined from the data of this study.
Reporting bias is a systematic error because participants in a study do not give honest answers. This is frequently the case with questions dealing with unpleasant or morally delicate issues [29]. Undoubtedly, questions dealing with fatal disease, death, cadavers, autopsy and funeral arrangements belong to this category. In our survey, patients and relatives mostly consented to hypothetical questions about permitting the autopsy of a relative or their own autopsy. In contrast, if relatives were faced with the real loss of a beloved family member, the consent rate was only 27%, even after intervention. This suggests a socially desirable response pattern, i.e., a bias towards consenting to an autopsy. When faced with the decision on the autopsy of a loved one, however, these rational considerations may have been superseded by different thoughts and feelings. Again, the magnitude of a presumed reporting bias cannot be determined from the data available. However, it is likely that the combined impact of a non-response bias and a reporting bias explains most of the discrepancy between the positive response to hypothetical questions and the low consent rate when faced with the actual death of a family member.
Training physicians in how to communicate with grieving relatives effectively and how to ask for autopsy permission may substantially increase autopsy rates. Motivational interviewing is an easy-to-learn and effective technique to reach this goal. Maximising the results of this approach in a cost-efficient manner may involve a standardised procedure using online training for medical practitioners and uniform questionnaires available to all hospitals. Moreover, the training should be done regularly due to the constant fluctuation of medical staff.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Brinkmann B , Du Chesne A , Vennemann B . Aktuelle Daten zur Obduktionsfrequenz in Deutschland [Recent data for frequency of autopsy in Germany]. Dtsch Med Wochenschr. 2002;127(15):791–5. Article in German. doi:.https://doi.org/10.1055/s-2002-25021
2 Modelmog D , Goertchen R . Der Stellenwert von Obduktionsergebnissen. Dtsch Arztebl. 1992;89:3434–40. Article in German.
3 Habeck JO , Waller H . Die Anzahl der Obduktionen im Institut für Pathologie Chemnitz vor und nach der Wiedervereiningung (1987-1992) [The number of autopsies at the Chemnitz Institute of Pathology before and after unification (1987-1992)]. Pathologe. 1993;14(4):188–92. Article in German.
4 Shojania KG , Burton EC , McDonald KM , Goldman L . Changes in rates of autopsy-detected diagnostic errors over time: a systematic review. JAMA. 2003;289(21):2849–56. doi:.https://doi.org/10.1001/jama.289.21.2849
5 Burton S , Dalby JT . Psychological autopsy in the investigation of serial neonaticides. J Forensic Sci. 2012;57(1):270–2. doi:.https://doi.org/10.1111/j.1556-4029.2011.01934.x
6 Rosenbaum GE , Burns J , Johnson J , Mitchell C , Robinson M , Truog RD . Autopsy consent practice at US teaching hospitals: results of a national survey. Arch Intern Med. 2000;160(3):374–80. doi:.https://doi.org/10.1001/archinte.160.3.374
7 Grassow-Narlik M , Wessolly M , Friemann J . Obduktionszahlen in Deutschland [Autopsy rates in Germany]. Pathologe. 2017;38(5):422–9. Article in German. doi:.https://doi.org/10.1007/s00292-017-0340-7
8 Petros K , Wittekind C . Die Obduktion - ein Verfahren der Medizingeschichte? [Autopsy—a procedure of medical history?] Med Klin Intensivmed Notf Med. 2014;109(2):115–20. Article in German. doi:.https://doi.org/10.1007/s00063-013-0214-6
9 Groß D , Wilhelmy S . Klinische Obduktionen aus medizinethischer Sicht [Clinical autopsies from a medical ethics perspective]. Pathologe. 2017;38(5):396–401. Article in German. doi:.https://doi.org/10.1007/s00292-017-0328-3
10 Birdi KS , Bunce DJ , Start RD , Cotton DW . Clinician beliefs underlying autopsy requests. Postgrad Med J. 1996;72(846):224–8. doi:.https://doi.org/10.1136/pgmj.72.846.224
11 Cox JA , Lukande RL , Kateregga A , Mayanja-Kizza H , Manabe YC , Colebunders R . Autopsy acceptance rate and reasons for decline in Mulago Hospital, Kampala, Uganda. Trop Med Int Health. 2011;16(8):1015–8. doi:.https://doi.org/10.1111/j.1365-3156.2011.02798.x
12 Kahl A . Die Einstellung der Bevölkerung zur klinischen Sektion: Ergebnisse einer repräsentativen Erhebung [Public perceptions of hospital autopsies]. Pathologe. 2011;32(4):345–8. doi:.https://doi.org/10.1007/s00292-011-1428-0
13 Sonderegger-Iseli K , Burger S , Muntwyler J , Salomon F . Diagnostic errors in three medical eras: a necropsy study. Lancet. 2000;355(9220):2027–31. doi:.https://doi.org/10.1016/S0140-6736(00)02349-7
14 Battle RM , Pathak D , Humble CG , Key CR , Vanatta PR , Hill RB , et al. Factors influencing discrepancies between premortem and postmortem diagnoses. JAMA. 1987;258(3):339–44. doi:.https://doi.org/10.1001/jama.1987.03400030055031
15 Goldman L , Sayson R , Robbins S , Cohn LH , Bettmann M , Weisberg M . The value of the autopsy in three medical eras. N Engl J Med. 1983;308(17):1000–5. doi:.https://doi.org/10.1056/NEJM198304283081704
16 Stevanovic G , Tucakovic G , Dotlic R , Kanjuh V . Correlation of clinical diagnoses with autopsy findings: a retrospective study of 2,145 consecutive autopsies. Hum Pathol. 1986;17(12):1225–30. doi:.https://doi.org/10.1016/S0046-8177(86)80564-0
17 Modelmog D , Rahlenbeck S , Trichopoulos D . Accuracy of death certificates: a population-based, complete-coverage, one-year autopsy study in East Germany. Cancer Causes Control. 1992;3(6):541–6. doi:.https://doi.org/10.1007/BF00052751
18 Shojania KG , Burton EC , McDonald KM , Goldman L . The autopsy as an outcome and performance measure. Evid Rep Technol Assess (Summ). 2002;(58):1–5.
19 Rollnick S , Miller WR . What is motivational interviewing? Behav Cogn Psychother. 1995;23(04):325–34. doi:.https://doi.org/10.1017/S135246580001643X
20 Burke BL , Arkowitz H , Menchola M . The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003;71(5):843–61. doi:.https://doi.org/10.1037/0022-006X.71.5.843
21 Rubak S , Sandbaek A , Lauritzen T , Christensen B . Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305–12.
22 Apodaca TR , Longabaugh R . Mechanisms of change in motivational interviewing: a review and preliminary evaluation of the evidence. Addiction. 2009;104(5):705–15. doi:.https://doi.org/10.1111/j.1360-0443.2009.02527.x
23Rothe A. Möglichkeiten der Steigerung der Autopsierate am Krankenhaus der Regelversorgung. Dissertation, Universität Leipzig. 2015.
24 Dunhill D , Schmidt S , Klein R . Motivational interviewing interventions in graduate medical education: a systematic review of the evidence. J Grad Med Educ. 2014;6(2):222–36. doi:.https://doi.org/10.4300/JGME-D-13-00124.1
25 Harrington DE , Sayre EA . Managed care and measuring medical outcomes: did the rise of HMOs contribute to the fall in the autopsy rate? Soc Sci Med. 2010;70(2):191–8. doi:.https://doi.org/10.1016/j.socscimed.2009.09.018
26 Kahl A . Klinische Sektionen. Umfrage zeigt allgemeine Zustimmung. Dtsch Arztebl. 2010;107:2492–3.
27 Hill AB . The environment and disease: association or causation? Proc R Soc Med. 1965;58:295–300.
28 Rothman KJ . Causes. Am J Epidemiol. 1976;104(6):587–92. doi:.https://doi.org/10.1093/oxfordjournals.aje.a112335
29Harms V. Medizinische Statistik. 8 ed. Lindhöft: Harms Verlag; 2012. 543 p.
30 Gardner R , Peskin L , Katz JL . The physician, the autopsy request, and the consent rate. J Med Educ. 1973;48(7):636–44.
31 Souza VL , Rosner F . Increasing autopsy rates at a public hospital. J Gen Intern Med. 1997;12(5):315–7. doi:.https://doi.org/10.1007/s11606-006-5069-6
32 Champ C , Tyler X , Andrews PS , Coghill SB . Improve your hospital autopsy rate to 40-50 per cent, a tale of two towns. J Pathol. 1992;166(4):405–7. doi:.https://doi.org/10.1002/path.1711660413
No financial support and no other potential conflict of interest relevant to this article was reported.