Management of non-COVID-19 patients should not be the dark side of the pandemic
Salah D. Qanadli, David C. Rotzinger
With coronavirus disease (COVID-19), the world has entered a new era in the management of modern infectious diseases. After the crashing arrival of the epidemic in Europe, the World Health Organization (WHO) declared the COVID-19 pandemic [1]. The rapid spread of contagion has forced states and health systems to adapt to the emergency. Two priorities had then emerged to deal with the pandemic: slowing the transmission of the virus and reorganising the healthcare system to cope with the massive arrival of COVID-19 patients, especially those who require advanced care.
Although organised at the national level, a joint policy was adopted by the majority of countries to slow down the epidemic, based on containment, physical distancing measures, and the use of protective materials. The reorganisation of healthcare systems aimed to prepare hospitals not only to receive COVID-19 patients, but also to protect other patients from viral transmission during their transit in the facilities and, finally, to ensure that institutions have the resources necessary to care for COVID-19 patients.
Quickly, professional healthcare societies [1–3], as well as institutions, structured the workflow for COVID-19. Despite the temporary changes in workflow, it was mandatory to maintain appropriate services for non-COVID-19 patients [3] who need rapid management. To help healthcare professionals establish priorities, guidance and recommendations have been published [4]. For example, to manage non-COVID-19 candidates for an interventional radiology procedure, a four-point scale was built to identify and prioritise patients. Priority number 1 was assigned to urgent procedures; priority number 2 to those to be performed within 7 days; priority number 3 to procedures to be delivered depending on facility/resource availability, but within 30 days; priority number 4 was for interventions that could be delayed beyond 30 days.
At the social level, communication on COVID-19 using all information channels, traditional and modern such as social networks, was very intensive and overall very effective [5, 6]. On the other hand, although healthcare professionals are well aware of priorities, it is interesting to notice that public communication related to patients not having COVID-19, in particular those in priority groups numbers 2 and 3, has not been sufficient. In our opinion, the COVID-19 communication created a climate of fear of care institutions, with a collateral effect of making patients requiring urgent or semi-urgent care hesitate to consult their doctors or present themselves to emergency departments.
Figure 1 illustrates three examples of non-COVID-19 patients who have been admitted several weeks later than they would have been in usual practice. All three patients presented with an advanced stage of infectious disease, including peritonitis with abdominal abscess (panel a), scrotal abscess (panel b) and peri-prosthethic aortic collection (panels c and d). Such conditions have not been seen in western countries for decades. Whereas the first two patients had a common factor, hesitation to consult earlier because of the COVID-19 outbreak, the third one was an indirect victim of restricted health services due to COVID-19.
Figure 1: Coronal reformatted contrast-enhanced abdominal computed tomography (CT) (a) in a 69-year-old man, presenting with abdominal pain in the right upper quadrant for 2 weeks, shows perforated cholecystitis with a gas-containing perihepatic abscess (white star). Scrotal ultrasound (b) in a 38-year-old man presenting with scrotal pain for 2 weeks shows left testicle (T) with adjacent lobulated hypoechogenic fluid collection consistent with a scrotal abscess (white arrowheads). Coronal (c) and axial (d) aortic CT angiography in an 88-year-old man, shows post-endovascular abdominal aneurysm repair with a type 2 endoleak originating from a lumbar artery (black arrow), heterogeneous density with the presence of gas inside the aneurysmal sac (white arrowhead), and periarortic fat stranding with a small fluid collection (white arrow), indicating acute infection of the aneurysmal sac.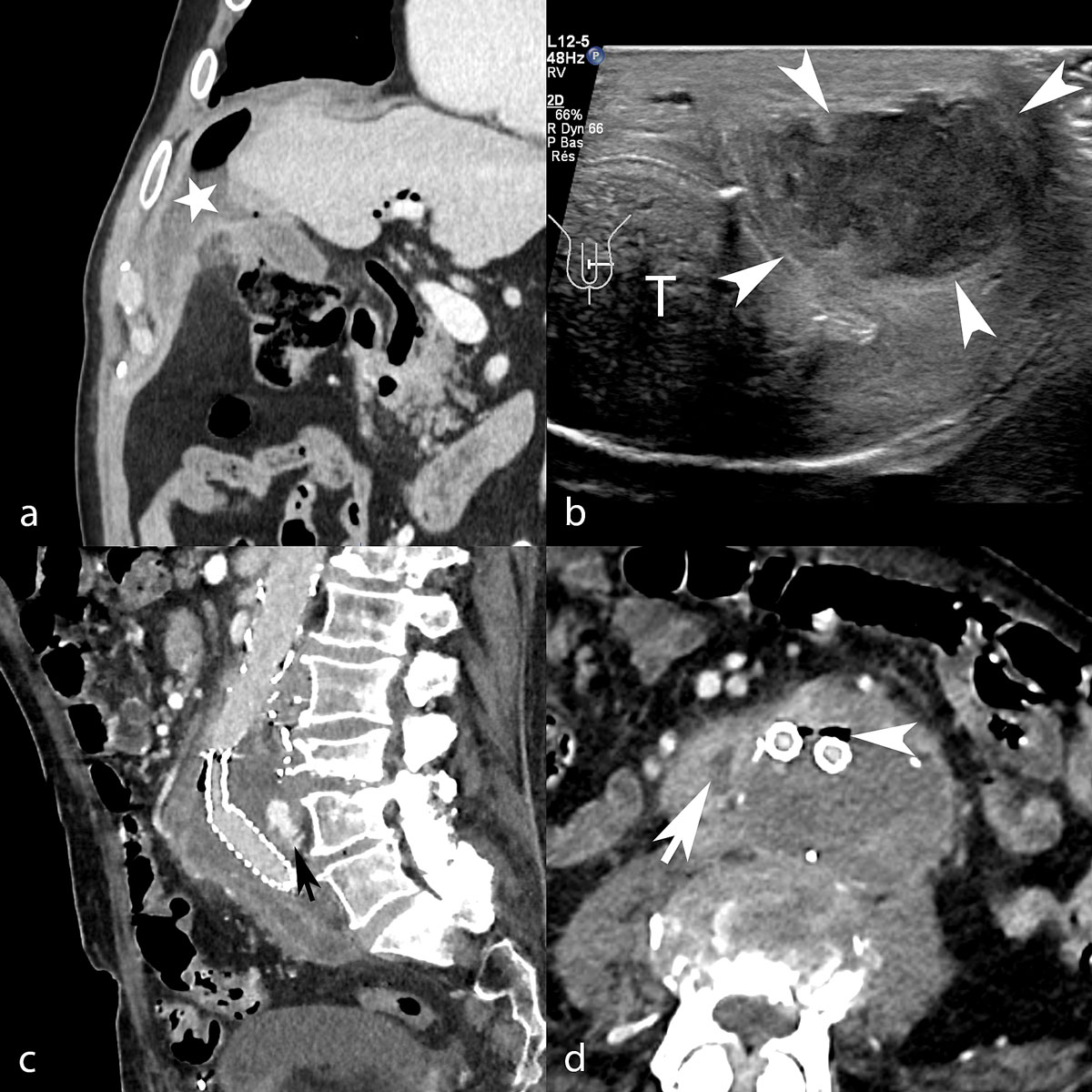
To avoid having more patients suffer from the COVID-19 reorganisation of patient workflows, we think that proper communication should be provided directly to patients to ensure timely management, regardless of the nature of the disease. It also important to consider progressive readjustment of healthcare policies to accept and treat patients, at least those in priority categories 2 and 3. Such strategies should be applied as fast as possible, depending on local conditions. We also think that a certain degree of flexibility should be allowed for institutions to adapt their rules, as the COVID-19 infection is not geographically uniform.
In conclusion, it is time to focus on non-COVID-19 patients who have been at least partially overlooked, to avoid a massive increase in the non-COVID-19-related morbidity and mortality. Flattening the curve of COVID-19 should not be associated with sharpening the curve of complications from non-COVID-19 diseases.
Salah D. Qanadli, Cardiothoracic and Vascular Division, Department of Diagnostic and Interventional Radiology, Lausanne University Hospital and University of Lausanne, Switzerland
David C. Rotzinger, Cardiothoracic and Vascular Division, Department of Diagnostic and Interventional Radiology, Lausanne University Hospital and University of Lausanne, Switzerland
References
- World Health Organization. Coronavirus disease COVID-19 Data. From who.imt/emergencies/disease/novel-coronavirus-2019. Accessed 2020 June 25.
- Mossa-Basha M, Meltzer CC, Kim DC, Tuite MJ, Kolli KP, Tan BS. Radiology Department Preparedness for COVID-19: Radiology Scientific Expert Review Panel. Radiology. 2020;296(2):E106–12 https://doi.org/10.1148/radiol.2020200988. PubMed
- www.sfrnet.org/rc/org/sfrnet/htm/Article/2010/htm-20101118-093059-875/src/htm_fullText/fr/RecosCOVID-19SFR-FRId.pdf. Accessed 2020 June 25.
- Qanadli SD, Zech C, Monnard E, Binkert C, Denys A, Pfammater T. Interventional Radiology workflow during the COVID-19 pandemic: recommendations of the Swiss Society of Vascular and Interventional Radiology. Swiss Med Wkly. 2020;150:w20261. doi:https://doi.org/10.4414/smw.2020.20261. PubMed
- Cuan-Baltazar JY, Muñoz-Perez MJ, Robledo-Vega C, Pérez-Zepeda MF, Soto-Vega E. Misinformation of COVID-19 on the Internet: Infodemiology Study. JMIR Public Health Surveill. 2020;6(2):e18444 https://doi.org/10.2196/18444. PubMed
- Giroux CM, Moreau KA. Leveraging social media for medical education: Learning from patients in online spaces. Med Teach. 2020;42(9):970–2 https://doi.org/10.1080/0142159X.2020.1779920. PubMed
