Figure 1 Screening, inclusion and follow up.
DOI: https://doi.org/10.4414/smw.2019.20120
Alcohol misuse is a major health problem causing a significant burden of avoidable diseases. It accounted for 5.9% of all deaths in 2014, corresponding to 3.3 million deaths worldwide [1]. In the European Union, the trend in alcohol consumption between 1990 and 2014 showed a slight decrease (−18%). Meanwhile, alcohol-attributable mortality increased (+4%), principally related to liver cirrhosis, cardiovascular deaths, cancers and injuries, and followed a west-east gradient [2], with the Mediterranean region showing lower mortality. In the central-western European Union, the standardised death rate decreased from near 40 per 100,000 to near 30 per 100,000. In Europe, alcohol overuse is the third risk factor for disease and mortality, after tobacco and high blood pressure [3]. The economic cost to society is high, varying between $358 and $837 per head in high-income countries in 2007 [4, 5].
In Switzerland also, alcohol misuse is an important public health issue, for example causing 1768 deaths and 42,627 years of life lost in 2011 [6]. A large part of this burden of disease is not related to alcohol dependence but to excessive drinking, defined as drinking that has negative health consequences without signs of alcohol dependence, but also as drinking more than “low risk limits”. Those drinking limits are not the same in all countries and have been reduced recently [7]. At the time of our study they were defined in Switzerland as more than 210 g of alcohol (1 drink containing 10 grams) per week for men, and 140 g for women, according to the World Health Organization recommendations. Only 6% of dependent drinkers receive medical treatment and excessive drinkers often do not recognise their drinking as being so. Consequently, professionals miss opportunities to identify them and thus do not provide timely intervention [8].
Historically, the principal treatment objective for alcohol misuse has been total abstinence, particularly for patients suffering from alcohol dependence. In the 1970s, arguments in favour of considering controlled (or reduced) drinking as a possible treatment alternative emerged, causing a strong emotional debate [9]. Discussion about the validity of controlled drinking as a treatment objective continues. Seventeen randomised controlled studies were analysed in 2000 [10], showing a congruent positive effect in favour of behavioural self-controlled training. A second review article [11] also supported the utility of controlled drinking as an alternative objective of treatment for problematic alcohol drinkers not willing to abstain.
The six-step controlled drinking programme, “Alcochoix+”, was developed in Quebec and implemented in social services there in 2004 by the health minister. Its objectives were to reduce alcohol consumption among excessive nondependent drinkers and prevent alcohol dependence [12]. The underlying theoretical framework includes a motivational and cognitive-behavioural approach, social learning theory and relapse prevention. It comprises six sessions lasting 1 week each, focusing on learning how to measure consumption, written self-observation, recognition of “at-risk” situations and development of individualised strategies, determination for a self-determined objective, alternatives to alcohol to fulfil needs and pleasures, and skills to maintain changes in the future. Formal efficacy studies of this programme are not available, but the implementation of the Alcochoix programme was positively evaluated in Quebec [13].
The Quebec programme was adapted and imported to Switzerland in 2008. Alcochoix+, originally designed for excessive drinkers, was introduced in 12 specialised healthcare structures. After initial enthusiasm, recruitment waned.
The primary objectives of this cohort study were to evaluate the rate of recruitment for a structured controlled drinking programme in the French-speaking part of Switzerland. The evolution of drinking quantities and their pattern was also part of the study. Secondary objectives were to describe the nature of the population, the completion rate of the programme and the quality of life of participants. We also assessed the satisfaction of participants and professionals within the programme. The main hypothesis was that the consumption of people following the Alcochoix+ programme would decrease. The rest of the study was mainly descriptive.
This multicentre prospective observational cohort study was carried out with recruitment between May 2010 and September 2011 in all the centres proposing the Alcochoix+ programme in the French-speaking part of Switzerland. Twelve centres were included in the study, in seven cantons: Geneva (Hôpitaux Universitaires de Genève, Fondation Phénix, Association Argos, Croix-Bleue), Vaud (Fondation vaudoise contre l’alcoolisme, Croix Bleue), Valais (Addiction Valais), Neuchâtel (Centre Neuchâtelois d’alcoologie, Croix-Bleue), Jura (Addiction Jura), Fribourg (Fondation Le Torry), Berne (Santé bernoise).
The professionals providing the programme had principally a psychosocial background and were trained by the GREA (Groupement Romand d’Etudes des Addictions). Included in the two-day course were also a medical doctor and a nurse; it was the former who took the decision as to who should be included in the study.
This six-step controlled drinking programme consists of a 113-page booklet given to the patient after an evaluation session. The booklet contains information, exercises to be completed by the patient and examples to help the patient to understand the process. Each of the six parts can be completed in 1 week or several weeks, if needed, and during this time the participant writes about his/her consumption with the place and conditions in which it occurs. The reduction of alcohol intake takes place between the second and the fifth sessions.
The first step consists of: learning what an alcohol standard unit is and how to measure one’s own consumption; information about the limits of low-risk drinking; an exercise about user’s quality of life; and an exercise to enhance motivation to change alcohol habits.
The second part introduces the “at risk” situation, meaning that the user has to realise that excessive drinking will happen only in given situations. This allows the user to find strategies to control his/her alcohol intake for each of those situations. At the end of this session, the participant is invited to make an alcohol-free break of one to seven days, in order to better understand the situations in which alcohol was felt to be needed and to diminish alcohol tolerance, thus promoting self-confidence and a subsequent behavioural change.
The third step consists mainly of a reflection on abstinence versus controlled drinking in order to help the user to focus on a precise objective of a number of drinking days per week, and an upper limit to the number of alcohol units taken on those days and for all the week. A section proposing strategies for each “at risk” situation is in the middle of the booklet, with the possibility for the users to invent their own strategies.
The fourth step is an appraisal of changes brought about through the programme, with a new evaluation of motivation and quality of life, both compared with the situation in the first step. People facing difficulties are counselled to consider another way to find help with their drinking. An exercise centred on alternative pleasures to alcohol consumption is found at the end of this section.
The fifth section of the booklet contains a part to help understanding of which needs are fulfilled through the consumption of alcohol and how alternatives can prevent it. Unrealised needs causing negative emotions (then managed with alcohol consumption) are sought, and new ways to try to fix the main problem are suggested.
Finally, the sixth step is about keeping a week of self-observation every month for 6 months and creating an emergency plan in case of relapse into the old consumption pattern. The programme can be used by the patient alone, or with the help of a professional in an individual or group setting (“Programme setting” in table 2 below).
Inclusion criteria were to be aged 18 or more and proposed or referred for the controlled drinking programme. Exclusion criteria were pregnancy, any disease contraindicating the consumption of alcohol (e.g., hepatic cirrhosis, pancreatitis) or any medication known to interact with alcohol (disulfiram, metronidazole).
Data were collected in a questionnaire before and after the programme (6 weeks) by the clinician in the presence of the patient. The follow-up questionnaires at 12 months after the end of the programme were completed by a research assistant via telephone calls. The quantities drunk were assessed orally, with the subject estimating an average for the period concerned: usually the last week before the programme, the week directly after the programme, and the last 6 months at the 12 months’ evaluation (number of drinking days per week, number of drinks per day, number of drinks per week and number of heavy drinking episodes, defined as more than six drinks at one occasion).
As the Alcochoix+ programme was designed for excessive, nondependent drinkers, we did not collect the duration of alcohol use disorder, if participants had had previous treatment or if they were taken anti-craving medication.
Participants signed a written consent form and received a compensation of CHF 30 after each of the two telephone surveys. Ethical approval for the study was granted by Geneva cantonal Research Ethics Committee (CER:09-305).
Alcohol use severity was measured at screening using the AUDIT score [14]. This WHO-developed and validated questionnaire contains 10 questions about frequency and quantity of alcohol use, followed by questions regarding dependence and undesired consequences. The cut-off score for alcohol dependence is 13 points [15]. This test does not provide a diagnosis, and has to be interpreted in the light of its sensitivity and specificity. The QBDA (Questionnaire Bref de la Dépendance à l’Alcool) is the French translation of the SADD questionnaire [16]. In the QBDA, a score of 18 or more is considered to justify follow-up in a specialised centre. Quality of life was measured with 14 questions taken from the SF-36 and SIP-2L (Sickness Impact Profile) questionnaires, selected items modifiable by alcohol intake [17]. Selected questions can be found in table 3 below.
Satisfaction with the programme was measured by direct questions as to whether the participants were very satisfied, rather satisfied, neutral, rather unsatisfied or very unsatisfied, and if they would recommend the programme to a close relative.
Sociodemographic characteristics were described as frequencies for categorical measures and as median and interquartile range (IQR) for continuous measures. Successive data (at inclusion, 6 weeks and 1 year follow-up) were compared with the chi-squared test for categorical measures and Student’s t-test for continuous measures.
Evolution between time intervals for self-reported consumption, AUDIT scores, QBDA scores and quality of life scores were evaluated through comparison of the mean difference by testing the null hypothesis with a Wilcoxon test. All the data were also calculated using the maximal bias hypothesis, meaning that patients lost to follow up were considered to have unchanged (high) alcohol consumption.
Possible associations between the difference of AUDIT scores, alcohol consumption over time and the sociodemographic characteristics were tested using a linear model with the difference of consumption or scores as variable data, and initial characteristics of participants as independent data. Type 1 error was set at 0.05 (statistical level of significance). For the results at 1 year, the p-values concern the statistical difference between before the programme and at 1 year follow up.
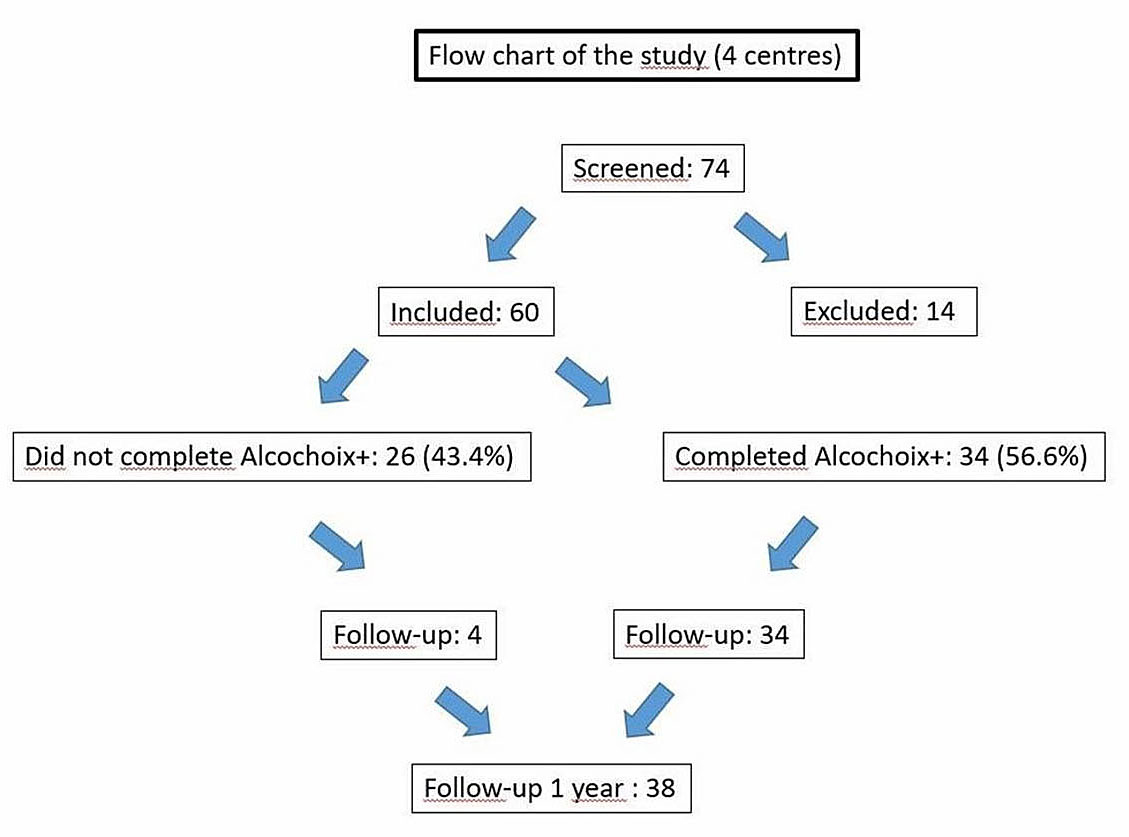
Four out of 12 centres (12 different providers of the programme) offering the Alcochoix+ programme in the French-speaking part of Switzerland included patients for the cohort, representing 12 providers. During the 17-month recruitment period, only 74 patients were screened and 60 included (refusal rate 19%). The flow chart of the study is presented in figure 1.
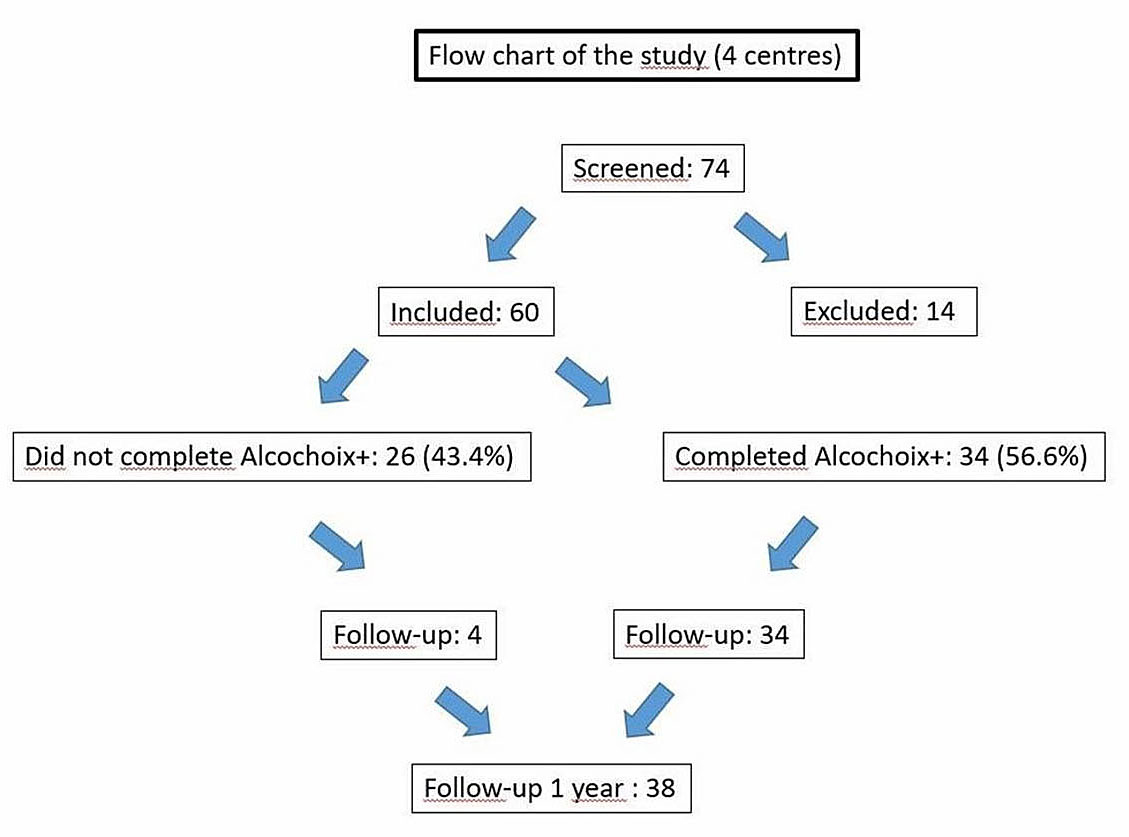
Figure 1 Screening, inclusion and follow up.
A quarter of the participants entered the programme on their own initiative and the remaining 75% through proposal by a health professional. The median age was 48 years and 72% were male. The majority of participants had middle or higher education. The sociodemographic characteristics at inclusion and the way people heard about the programme, are summarised in table 1.
Table 1 Sociodemographic characteristics at baseline.
| Sex | Men | 72% (43) |
| Women | 28% (17) | |
| Median age, years (IQR) | 48 (37–55) | |
| Civil status, % (n) | Married | 42% (25) |
| Single | 32% (19) | |
| Divorced | 17% (10) | |
| Separated | 8% (5) | |
| Widowed | 2% (1) | |
| Education, % (n) | 7 to 9 years | 10% (6) |
| 10 to 13 years | 48% (28) | |
| 14 and more years | 41% (24) | |
| Entry to programme, % (n) | Asked (by the participant) | 75% (45) |
| Proposed (by a professional) | 25% (15) | |
| Known from, % (n) | Newspaper | 0% (0) |
| Radio, TV, Internet | 11% (6) | |
| Notice, flyer | 15% (8) | |
| Parent, friend | 7% (4) | |
| Physician | 41% (22) | |
| Other | 26% (14) | |
IQR = Interquartile Range
The usual drinking frequency at inclusion was 7 days a week with a median of 6 standard units (60 g of alcohol) per day, and a median weekly consumption of 35 units. Frequency of heavy drinking episodes (more than 6 units) was a median of 50 in the last year, an average of 110 and median of 2 per week in the last week. The drinking profile of the participants pointed mainly towards alcohol dependence, 91% of them having an AUDIT score of 13 or more and the median score being 20.5. Only 9% of the participants had an AUDIT score in the range of excessive drinkers (less than 13). The median score on the QBDA questionnaire was 10.5, also suggesting moderate dependence. Fifty-five percent of the participants were smokers. Cannabis was used in the last year by 23% of participants, 8% of them declaring consumption three or more times per week. Seven percent of participants declared having used cocaine in the last year; 32% of them used sedative medication. The drinking and substance use characteristics at inclusion are listed in table 2.
Table 2 Drinking and substance abuse characteristics at inclusion.
| Alcohol consumption during previous week, median (IQR) | Days | 6 (4–7) |
| Units per day | 6 (4–7) | |
| Units per week | 30 (15–42) | |
| Heavy drinking days (>6 U) | 2 (1–4) | |
| Usual alcohol consumption, median (IQR) | Days | 7 (4.5–7) |
| Units per day | 6 (4–8) | |
| Units per week | 35 (20–46.5) | |
| Heavy drinking days (>6 U) per year | 50 (11–150) | |
| QDBA score, median (IQR) | 10.5 (8–14.75) | |
| AUDIT score, median (IQR) | 20.5 (16.25–24.75) | |
| Tobacco | Prevalence, % (n) | 55% (31) |
| Cigarettes per day, median (IQR) | 20 (16.25–30) | |
| Duration (years), median (IQR) | 20 (13–29.5) | |
| Sedative medication, % (n) | No | 68% (40) |
| Less than 3 times a week | 10% (6) | |
| 3 or more times a week | 22% (13) | |
| Cannabis, % (n) | No | 77% (46) |
| Less than 3 times a week | 15% (9) | |
| 3 or more times a week | 8% (5) | |
| Cocaine, % (n) | No | 93% (56) |
| Less than 3 times a week | 7% (4) | |
| Heroin, % (n) | No | 100% (60) |
| Programme setting, % (n) | Individual | 10% (6) |
| Counselled | 83% (49) | |
| Group | 7% (4) | |
AUDIT = Alcohol Use Disorder Identification Test; QBDA = Brief Questionnaire on Alcohol Dependence (in French “Questionnaire Bref sur la Dépendance à l’Alcool”)
About half of the participants considered their quality of life to be satisfying at inclusion, as between 38 to 68% of them reported being “rather satisfied” or “very satisfied” for the different items. The lowest score of 38% was for the sleep quality and main psychological well-being. The two highest scores were for family (68%) and general health (61%). Another 14 to 40% of participants reported to be neither “satisfied” nor “unsatisfied”, depending on the item. Quality of life estimations are presented in table 3.
Table 3 Quality of life estimation at inclusion, % (n).
| Very unsatisfied | Rather unsatisfied | Neither satisfied nor unsatisfied | Rather satisfied | Very satisfied | |
|---|---|---|---|---|---|
| Health in general | 5% (3) | 7% (4) | 27% (15) | 52% (29) | 9% (5) |
| Physical fitness | 4% (2) | 14% (8) | 34% (19) | 39% (22) | 9% (5) |
| Sleep | 13% (7) | 32% (18) | 18% (10) | 20% (11) | 18% (10) |
| Energy level | 5% (3) | 23% (13) | 29% (16) | 27% (15) | 16% (9) |
| Social activities | 5% (3) | 20% (11) | 21% (12) | 39% (22) | 14% (8) |
| Family relationships | 2% (1) | 16% (9) | 14% (8) | 50% (28) | 18% (10) |
| Couple relationship | 5% (3) | 13% (7) | 40% (22) | 33% (18) | 9% (5) |
| Work or study | 15% (8) | 11% (6) | 24% (13) | 36% (20) | 15% (8) |
| Finances | 25% (14) | 18% (10) | 18% (10) | 30% (17) | 9% (5) |
| Psychological well being | 5% (3) | 39% (22) | 18% (10) | 34% (19) | 4% (2) |
| Physical appearance | 2% (1) | 11% (6) | 36% (20) | 41% (23) | 11% (6) |
| Self esteem | 4% (2) | 30% (17) | 21% (12) | 39% (22) | 5% (3) |
| Sexual relations | 16% (9) | 13% (7) | 29% (16) | 32% (18) | 11% (6) |
| Pleasure in life in general | 2% (1) | 21% (12) | 18% (10) | 50% (28) | 9% (5) |
During follow-up, 26 participants (43.3%) quit the programme for unknown reasons. All of them had a follow-up call but were not reachable or declined to pursue the study without giving a reason. We considered these 26 drop-outs to have unchanged alcohol consumption. Table 4 presents the comparison between individuals who quit the programme and those who continued. No difference was found regarding gender, education, way of entering the programme, alcohol consumption or AUDIT score.
Table 4 Comparison of baseline characteristics between people continuing and lost to follow-up.
|
Followed up
(n = 34) |
Lost to follow up
(n = 26) |
p-value | |
|---|---|---|---|
| Men (vs women) | 23 | 20 | 0.43 |
| Education <10 years (vs ≥10 years) | 19 | 15 | 0.85 |
| Referral to programme (vs own initiative) | 25 | 20 | 0.76 |
| Alcohol units/week (mean) | 34.28 | 31.65 | 0.67 |
| AUDIT score (mean) | 20.59 | 19.53 | 0.56 |
AUDIT = Alcohol Use Disorder Identification Test
Thirty-four participants completed the programme. In a maximal bias hypothesis analysis, we observed a reduction in the amount of self-reported alcohol consumption after completing the programme. Twenty-four participants (40%) were considered to have a good outcome as they completed the programme, avoided any heavy drinking episode and reached their objective or did better in terms of drinking days per week (18 and 6 participants, respectively) and units of alcohol per day (15 and 9). One more participant declared not having any episode of heavy drinking at this time, immediately after completing the programme. Sixteen percent of participants reached an AUDIT score of 7 or less (men), and 6 or less (women) after the programme, compared with any other person before.
The weekly consumption for all participants (considering the consumption to patients lost to follow-up unchanged) dropped from a mean of 33.2 drinks (last week) to 21.6 drinks a week (p = 0.001), with a frequency decreasing from 5.4 days to 4.0 days (p = 0.001) and a mean of 6.0 drinks per day before the programme and 3.8 after (p = 0.002). Heavy drinking episodes went from a mean of 3.4 to 1.4 episodes per week (p = 0.03). The decrease in alcohol use for the 34 participants who completed the programme was greater: mean of 34.3 to 14.6 drinks per week (p <0.001), from 6.4 to 2.8 drinks per day (p = 0.002), and the number of binge drinking episodes from 4 to 0.7 per week (p = 0.03). The frequency of consumption decreased from 5.2 to 3 days per week (p <0.001). Mean AUDIT score was 20.8 before the programme and 14.1 upon completion (p = 0.001). We found no correlation between the characteristics of the participants at inclusion and the alcohol reduction after the programme. Self-reported quality of life improved: the score of 9 of the 14 items increased (25% of the basic level) whereas none decreased.
After 1 year, 38 participants were interviewed. A good outcome in terms of the absence of declared heavy drinking episodes was reported by four participants, only 6.7% of the collective; another 16 participants (26.7%) declared 1 or fewer heavy drinking episode per month. Compared with immediately after the programme, in the entire cohort alcohol consumption slightly rose, except for the frequency of heavy drinking episodes. The alcohol intake increased from 21.6 to 24.5 drinks a week (p <0.001), with a mean frequency changing from 4.0 to 4.6 days a week (p <0.001) and a mean number of drinks per day from 3.8 to 4.9 (p = 0.02; maximal bias hypothesis). Heavy drinking episodes were evaluated at an average of 68.5 episodes per year by the participants (p = 0.004).
For the 34 participants who completed the programme, alcohol consumption was lower after 1 year of follow-up, with 20.4 drinks per week (p <0.001), a frequency at 4.1 days a week (p <0.001) and quantity of 4.6 drinks per day (p = 0.01). The number of heavy drinking episodes was evaluated by participants at 1.2 episodes per week (p = 0.003).
Alcohol consumption and AUDIT scores before the programme, after its completion and at 1-year follow-up are illustrated in figure 2, and quality of life measurements in figure 3.
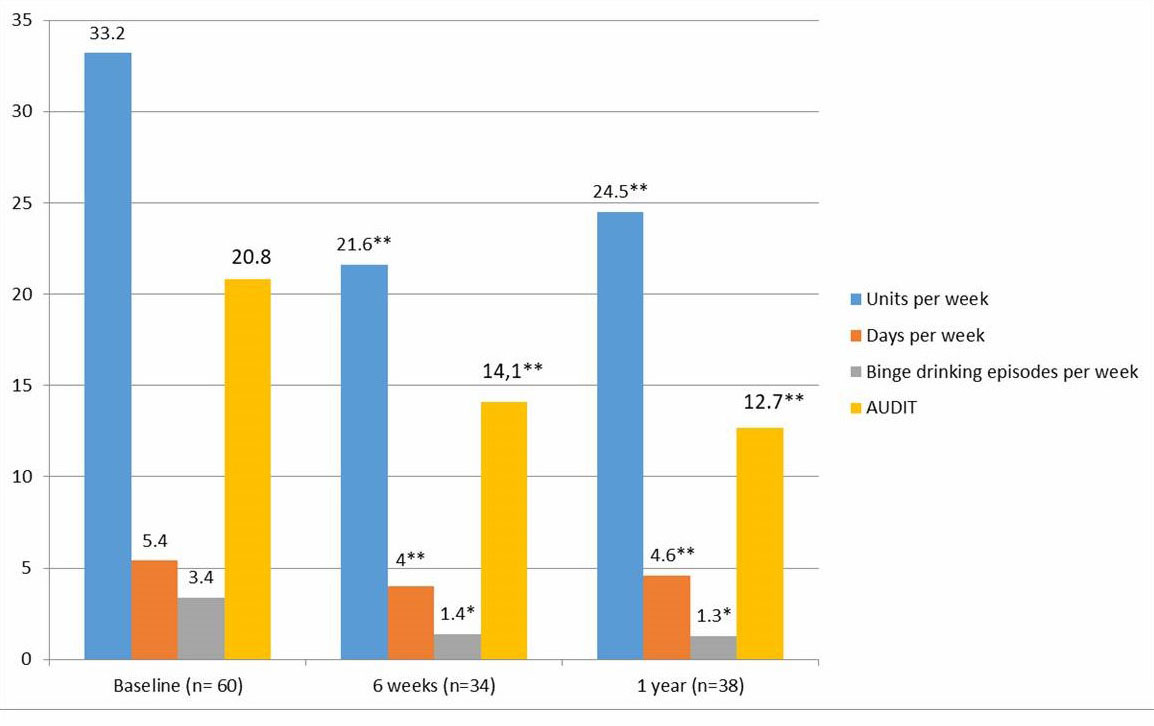
Figure 2 Alcohol consumption and Alcohol Use Disorder Identification Test (AUDIT) score at baseline and follow up. * p <0.05; ** p <0.01
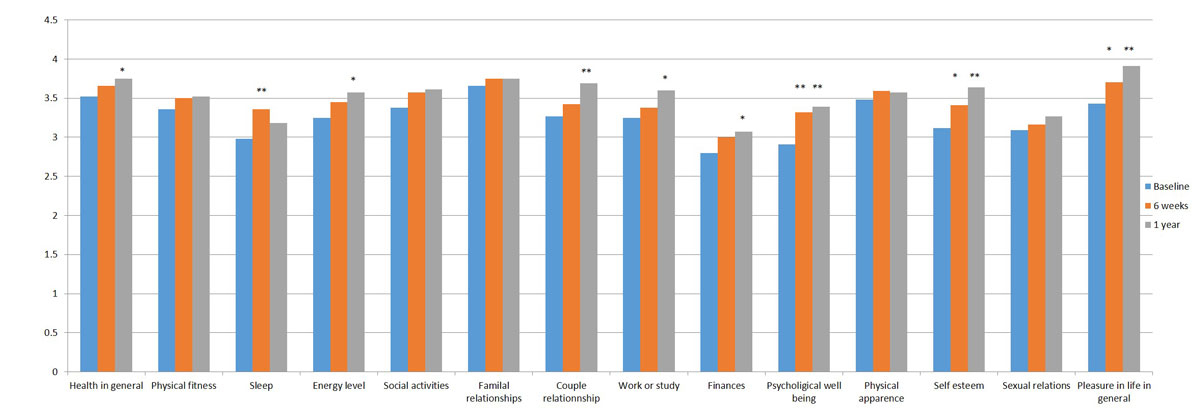
Figure 3 Quality of life at baseline and follow up. * p <0.05; ** p <0.01
Seventy percent of participants who terminated the programme declared that they were satisfied with the programme and would recommend it. All of the providers who took part in the study (n = 12) declared being satisfied with the programme and considered it an improvement in their practices.
The recruitment for this cohort in the French-speaking part of Switzerland was low and slower than expected. Based on the initial success of the programme after media coverage in Geneva in 2009, we postulated that we could include more than 200 participants in the cohort in 5 months. The number of patients included was, in the end, only 60 in 17 months. In Quebec, where implementation of the programme is extensive, not just in treatment centres, but also through large advertising campaigns, recruitment was about four times faster [13]. Our hypothesis to explain our recruitment difficulty is that promotion of the programme was insufficient and that to rely on busy field professionals to recruit people was a study design mistake. The treatment setting also might play a role: in Quebec the programme was implemented in the community, in social action centres, and trained social workers to identify excessive drinkers and to provide the controlled drinking programme even for a few in each centre. In contrast, in Switzerland, this programme was implemented only in specialised treatment centres. This may make it more difficult for excessive drinkers to ask for the programme. The fact that we recruited mostly moderately dependent participants, and not excessive drinkers, suggests a lack of self-recognition of excessive drinking and a lack of motivation to reduce alcohol consumption. The method of the study does not allow us to confirm this hypothesis. A strategy of screening and brief intervention in primary care [8] could be particularly useful for programmes such as Alcochoix+ to create a pool of patients. In addition, easy-to-understand information campaigns targeting drinkers at risk would also be good strategy.
Interestingly, the profile of our participants was quite similar to the Quebec populations formerly evaluated in terms of weekly declared alcohol consumption and dependence score [12]. In this cohort, participants showed other harmful behaviour, being twice more often tobacco and cannabis users than the general population in Switzerland [18], and one third of whom used sedatives.
The change in alcohol consumption (160 g per week reduction, about 40% of the initial amount), was four times higher than following brief interventions in emergency settings (decrease around 40g per week [19], where the patients had a lower initial alcohol consumption compared to our population). An important finding is that we observed users screened as moderately dependent drinkers (91% of the cohort having an AUDIT score at 13 or more), and reduced consumption is generally considered difficult in alcohol dependent drinkers. We can hypothesise that the declared median consumption of 35 units of alcohol per week is quite low for such drinkers reflecting an underestimate related to minimisation of consumption, often seen in dependent drinkers
The alcohol consumption observed in our cohort was similar to that of a cohort in a controlled drinking programme conducted in Alberta between 1994 and 1995 [20] in terms of completion of the programme and alcohol reduction. Our observations add support to controlled drinking as a possible and efficient goal of treatment, even for moderately dependent drinkers. A meta-analysis including all the controlled studies since the 1970s [10] also suggested this, and was confirmed later [21]. Nevertheless, this objective of treatment should be considered as complementary to abstinence and not as a replacement of it. For people with an important and long-lasting dependence – a defining criterion to orientate the goal of therapy [22] – abstinence remains probably the most efficient and safe treatment objective. How far controlled drinking programmes can serve as a motivational tool or a step towards abstinence, as suggested by our clinical observations, remains to be established.
The slight improvement in quality of life of participants over time is an interesting outcome of our controlled drinking programme. Without going into detail on the statistically significant, but of limited clinical relevance, changes in score of the various items, we highlight two items that particularly improved: self-esteem and pleasure in life. One of the goals of Alcochoix+ is to raise self-efficacy; the cognitive behavioural content in the fifth part of the programme is directed towards a search for old or new sources of pleasure as an alternative to alcohol.
The satisfaction observed in this cohort study was high (70% of participants), but the satisfaction rate was even higher (90%) in the implementation study in Quebec [13]. We can only hypothesise on the cause of this difference, but the treatment setting definitely might have played a role. Health professionals were unanimous about the importance of having an additional treatment proposal for patients not willing to abstain from alcohol. Considering the “treatment gap” that exists for people in difficulty with alcohol, we believe this to be particularly relevant. Also, with the changing limits for “low-risk drinking guidelines” [7], there will be a significant increase in excessive drinkers and a need for appropriate approaches.
Our study is one of the first with clinical follow-up data after a controlled drinking programme in a European context. Other strengths of our multicentre project include the large inclusion and limited exclusion criteria. Even if the number of participants was lower than expected, results of the intention-to-treat analysis showed good statistical significance.
There are several limitations of our study. First, its observational nature and the lack of randomisation and control group do not allow a conclusion on any causal relationship between the changes observed and the programme itself. Also, selection bias (recruitment of most motivated individuals) and a declaration bias are possible (an unvalidated questionnaire was used, asking about the average consumption for a period of 6 months at the final follow-up). However, in non-dependant or low-dependent drinkers, the reliability of self-declaration is known to be good and comparable to reports of relatives [23]. We did not use objective markers, such as biological tests, because we were expecting a majority of excessive drinkers for whom the level of alcohol consumption would have been too low to significantly modify blood tests. Finally, there was an important drop-out rate during the study (43.3%).
In conclusion, this prospective cohort study of participants in a structured six-step controlled alcohol drinking programme in the French-speaking part of Switzerland increases arguments for the potential interest of such approaches for excessive and moderately dependent drinkers. Overall, 40% of participants had a good outcome, having completed the programme, avoided any heavy drinking episodes and reached or exceeded their defined drinking objectives. For all, the number of heavy drinking days decreased more than 50%. The participants cut down their alcohol use by 160 g per week after the six steps of the Alcochoix+ programme. These changes remained rather stable after 1 year of follow-up. The quality of life of participants slightly improved over time and their level of satisfaction with the programme was high. Nevertheless, difficulties in recruiting participants, especially excessive drinkers, suggest that harmful alcohol use is poorly recognised in the population and among healthcare workers, and controlled drinking programmes are insufficiently known.
Public health campaigns and training for screening and evaluation of alcohol-use disorder are among the key words here. Finally, randomised controlled studies are still warranted to determine the specific effects and efficacy of controlled drinking programmes.
The results of this research have been addressed in a scientific report delivered to the Swiss Public Health authorities in May 2013 [24].
The research protocol was developed in Quebec at the RISQ (Recherche et Intervention en Substances psychoactives, Québec), in collaboration with H. Simoneau who is the main developer of the Alcochoix+ programme. We thank Anne-Sophie Jannot, MD, for her support in the statistical analyses and interpretation of the data, Kenan Sakbani, MD, and Joan and Sylvain Corderoy for their language corrections.
We received financial support from the Swiss Public Health Service.
No potential conflict of interest relevant to this article was reported.
1World Health Organization. Global status report on alcohol and health 2014. Geneva: World Health Organization; 2014. ISBN 978 92 4 069276 3 (PDF).
2World Health Organization. Public health successes and missed opportunities. Trends in alcohol consumption and attributable mortality in the WHO European Region, 1990-2014. Geneva: World Health Organization; 2016. ISBN 978 92 890 5167 5 (PDF).
3Anderson P, Møller L, Galea G, eds. Alcohol in the European Union Consumption, harm and policy approaches. Geneva: World Health Organization; 2012. ISBN 978 92 890 0264 6.
4 Rehm J , Mathers C , Popova S , Thavorncharoensap M , Teerawattananon Y , Patra J . Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223–33. doi:.https://doi.org/10.1016/S0140-6736(09)60746-7
5 Gustavsson A , Svensson M , Jacobi F , Allgulander C , Alonso J , Beghi E , et al.; CDBE2010Study Group. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(10):718–79. doi:.https://doi.org/10.1016/j.euroneuro.2011.08.008
6 Marmet S , Rehm J , Gmel G , Frick H , Gmel G . Alcohol-attributable mortality in Switzerland in 2011--age-specific causes of death and impact of heavy versus non-heavy drinking. Swiss Med Wkly. 2014;144:w13947. doi:.https://doi.org/10.4414/smw.2014.13947
7 Wood AM , Kaptoge S , Butterworth AS , Willeit P , Warnakula S , Bolton T , et al.; Emerging Risk Factors Collaboration/EPIC-CVD/UK Biobank Alcohol Study Group. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet. 2018;391(10129):1513–23. doi:.https://doi.org/10.1016/S0140-6736(18)30134-X
8 Kaner E . NICE work if you can get it: Development of national guidance incorporating screening and brief intervention to prevent hazardous and harmful drinking in England. Drug Alcohol Rev. 2010;29(6):589–95. doi:.https://doi.org/10.1111/j.1465-3362.2010.00236.x
9 Sobell MB , Sobell LC . Alcoholics treated by individualized behavior therapy: one year treatment outcome. Behav Res Ther. 1973;11(4):599–618. doi:.https://doi.org/10.1016/0005-7967(73)90118-6
10 Walters GD . Behavioral self-control training for problem drinkers: A meta-analysis of randomized control studies. Behav Ther. 2000;31(1):135–49. doi:.https://doi.org/10.1016/S0005-7894(00)80008-8
11 van Amsterdam J , van den Brink W . Reduced-risk drinking as a viable treatment goal in problematic alcohol use and alcohol dependence. J Psychopharmacol. 2013;27(11):987–97. doi:.https://doi.org/10.1177/0269881113495320
12Simoneau H, Landry M, Tremblay J. Alcochoix+: un guide pour atteindre vos objectifs. Quebec: Ministère de la Santé et des Services Sociaux du Québec ; 2004.
13Cournoyer LG, Simoneau H, Landry M, Tremblay J, Patenaude C. Évaluation d’implantation du programme Alcochoix+. Rapport final d’une recherche subventionnée par le Fonds québécois de la recherche sur la société et la culture (FQRSC #2008‐TO‐120890). Québec: Fond de recherche societé et culture; 2009.
14 Saunders JB , Aasland OG , Babor TF , de la Fuente JR , Grant M . Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88(6):791–804. doi:.https://doi.org/10.1111/j.1360-0443.1993.tb02093.x
15 Gache P , Michaud P , Landry U , Accietto C , Arfaoui S , Wenger O , et al. The Alcohol Use Disorders Identification Test (AUDIT) as a screening tool for excessive drinking in primary care: reliability and validity of a French version. Alcohol Clin Exp Res. 2005;29(11):2001–7. doi:.https://doi.org/10.1097/01.alc.0000187034.58955.64
16 Raistrick D , Dunbar G , Davidson R . Development of a questionnaire to measure alcohol dependence. Br J Addict. 1983;78(1):89–95. doi:.https://doi.org/10.1111/j.1360-0443.1983.tb02484.x
17 Foster JH , Powell JE , Marshall EJ , Peters TJ . Quality of life in alcohol-dependent subjects--a review. Qual Life Res. 1999;8(3):255–61. doi:.https://doi.org/10.1023/A:1008802711478
18Gmel G, Kuendig H, Notari L, Gmel C. Monitorage suisse des addictions - Consommation d'alcool, de tabac et de drogues illégales en Suisse en 2016. Lausanne: Addiction Suisse; 2017.
19 Bertholet N , Daeppen JB , Wietlisbach V , Fleming M , Burnand B . Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165(9):986–95. doi:.https://doi.org/10.1001/archinte.165.9.986
20Robson E, Edwards J, Gerry P, Mills K. Drinking decisions, final evaluation report. Capital Health Authority, Public Health Services; 1995.
21 Dawson DA , Grant BF , Stinson FS , Chou PS , Huang B , Ruan WJ . Recovery from DSM-IV alcohol dependence: United States, 2001-2002. Addiction. 2005;100(3):281–92. doi:.https://doi.org/10.1111/j.1360-0443.2004.00964.x
22 Rosenberg H . Prediction of controlled drinking by alcoholics and problem drinkers. Psychol Bull. 1993;113(1):129–39. doi:.https://doi.org/10.1037/0033-2909.113.1.129
23 Sanchez-Craig M , Annis HM , Bronet AR , MacDonald KR . Random assignment to abstinence and controlled drinking: evaluation of a cognitive-behavioral program for problem drinkers. J Consult Clin Psychol. 1984;52(3):390–403. doi:.https://doi.org/10.1037/0022-006X.52.3.390
24Favrod-Coune T, Aebischer G, Grondin-Giletti F, Girod I, Simoneau H, Broers B. Evaluation descriptive du programme «Alcochoix+» en Suisse romande. Available at: https://www.grea.ch/sites/default/files/rapport_evaluation_alcochoix_ofsp.pdf
We received financial support from the Swiss Public Health Service.
No potential conflict of interest relevant to this article was reported.